The trauma informed care principles aren't just a new technique; they represent a fundamental shift in how we approach care. It’s the difference between asking, "What's wrong with you?" and the far more insightful question, "What happened to you?" This isn't a specific type of therapy, but a complete framework for creating environments where healing is actually possible for everyone.
Understanding the Core Shift to Trauma Informed Care
Think of it like universal design in architecture. When architects build a ramp next to a flight of stairs, they aren't just helping people in wheelchairs. They're also helping parents with strollers, delivery workers with dollies, and anyone with a temporary injury. The ramp makes the building accessible and easier for everyone, regardless of their specific situation.
That’s exactly what trauma informed care principles do for a healing environment. You don't need to know a client's specific trauma history to apply them. Instead, you operate with the understanding that trauma is widespread and build a system that anticipates the needs of survivors. In doing so, you create a space that feels safer and works better for every single person who walks through your door.
This approach builds from a foundation of safety, which then allows for trust, collaboration, and empowerment to take root.
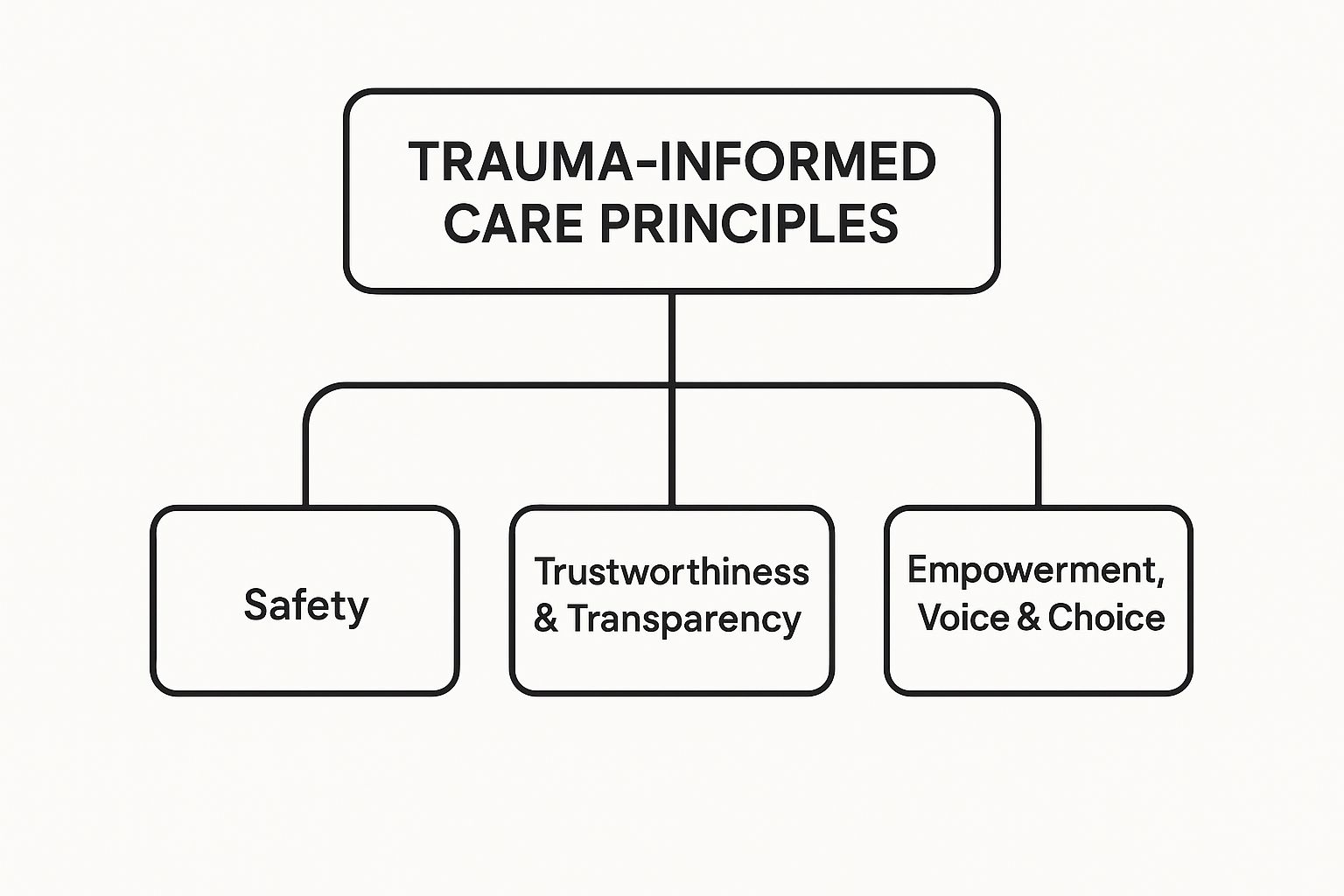
As the diagram shows, one principle logically flows into the next. You can't ask for trust or collaboration without first establishing a genuine sense of safety.
Why This Approach Is Essential
This isn't just a philosophical preference; it’s a statistical reality. A global study highlighted by the World Health Organization found that a staggering 70.4% of people have experienced at least one traumatic event. With numbers that high, assuming a client has a trauma history is simply the safer, more effective starting point for care.
A trauma-informed approach allows the client to feel safe and helps avoid any re-traumatization. It flips the script for a clinician from seeking out what is wrong with the patient to asking what is happening to the patient.
This perspective moves us beyond just managing symptoms and gets to the root causes of distress, paving the way for genuine healing. While the principles themselves are universal, they come to life through specific therapeutic methods. You can see exactly how these ideas are put into practice in our guide on what is trauma-informed therapy.
A Shift in Perspective From Traditional to Trauma Informed Care
To really get a feel for how different this is, it helps to see the two mindsets side-by-side. The traditional model often looks at behaviors as symptoms of a disorder that needs fixing. In sharp contrast, a trauma-informed model reframes those same behaviors as understandable—and often brilliant—adaptations to overwhelming experiences.
| Aspect | Traditional Care Approach | Trauma Informed Care Approach |
|---|---|---|
| Guiding Question | "What's wrong with you?" | "What happened to you?" |
| View of Behavior | Behaviors are symptoms of a pathology. | Behaviors are coping mechanisms for trauma. |
| Focus of Care | Diagnosis and symptom reduction. | Safety, building trust, and empowerment. |
| Client Role | Patient receiving expert treatment. | Partner in their own healing process. |
| Goal of Interaction | Compliance with the treatment plan. | Collaboration and shared decision-making. |
This small but profound shift changes everything—from the tone of the first phone call and the layout of the waiting room to the structure of every single therapy session. It’s all about creating an environment where clients can regain a sense of control and agency, which are often the very things that trauma stripped away in the first place.
Creating Physical and Emotional Safety
Think of Safety as the non-negotiable foundation for the entire therapeutic process. It’s the concrete slab poured before any walls go up. Before a client can even begin to trust a therapist, collaborate on a treatment plan, or feel empowered to make changes, they must first feel genuinely safe.
And we're not just talking about physical safety. We mean emotional and psychological safety, too. For someone with a history of trauma, the world often feels unpredictable and dangerous, keeping their nervous system locked in a state of high alert—a constant hum of hypervigilance.
Creating a safe environment starts long before a client ever sits down for their first session. It’s in the clear, easy-to-find directions on your website. It’s the calm, warm tone of the person who answers the phone. True safety is woven into the very fabric of the care experience from the absolute first point of contact.

This principle goes way beyond just having secure doors and a clean facility. It’s about intentionally designing a space and a process that helps calm a dysregulated nervous system rather than accidentally activating it.
What Physical Safety Looks Like in Practice
Physical safety involves all the tangible aspects of the environment. The goal is to create a setting that is predictable, calm, and welcoming—the direct opposite of the chaos and threat that often define traumatic experiences.
Put yourself in the client's shoes and walk through their journey, from the parking lot to the therapy room. Every single detail matters.
- A Welcoming Entry: Is the waiting room quiet? Is the seating comfortable and the lighting soft? Spaces that are overly bright, loud, or crowded can be incredibly overwhelming for a trauma survivor.
- Clear and Consistent Routines: Does the intake process follow a predictable sequence? Explaining what will happen next—"First, we'll review this form together, then I’ll give you a brief tour"—hands a sense of control back to the client.
- Respect for Personal Space: Staff should be trained to maintain a respectful physical distance and always ask for permission before entering a client's personal space, even for something as routine as taking a blood pressure reading.
These small, intentional actions send a powerful message. They communicate respect and predictability, signaling to the client’s brain that this is a place where they can finally begin to let their guard down.
Fostering Essential Psychological Safety
While physical safety is crucial, psychological safety is where the deepest healing becomes possible. It’s the assurance that a client can be vulnerable—sharing their most painful experiences, fears, and shames—without being judged, dismissed, or re-traumatized.
Psychological safety is the bedrock of a therapeutic relationship. It’s the unspoken promise that a client's story will be handled with care and that their emotional well-being is the absolute top priority.
This kind of safety is built slowly, through consistent, reliable, and compassionate interactions. For example, a therapist who clearly explains the limits of confidentiality during the very first session is building trustworthiness from minute one. When a client expresses a difficult emotion and is met with empathy instead of a clinical diagnosis, they learn that their feelings are valid and welcome here.
This is especially vital when addressing co-occurring disorders, where the tangled web of addiction and mental health creates unique vulnerabilities. You can learn more about how to support these clients in our guide to integrated dual diagnosis treatment.
By prioritizing both physical and psychological safety, we co-create a therapeutic sanctuary. This environment doesn’t just prevent further harm; it actively fosters the conditions necessary for a client to engage with their trauma and begin the real work of recovery. It is, without a doubt, the essential first step.
Building Trust Through Transparency
Once you’ve established a safe environment, the next critical layer is trust. For so many people with a history of trauma, trust hasn’t just been damaged—it’s been shattered. Often, it was broken by the very people or systems meant to protect them, which makes it an incredibly precious and fragile thing to rebuild.
Trustworthiness isn't some abstract ideal you talk about in a team meeting. It’s a set of active, observable behaviors. Building it isn't about making grand promises or guaranteeing a cure. Instead, it’s about showing up with consistency, reliability, and unflinching honesty in every single interaction, no matter how small.
You have to operate from the understanding that for a trauma survivor, the default expectation is often betrayal or disappointment. Every action you take can either reinforce that fear or begin to carefully dismantle it, creating a new, healthier blueprint for what a supportive relationship can actually look like.

Putting Trustworthiness Into Action
Transparency is how you make trustworthiness real and tangible. It means demystifying the entire care process. You pull back the curtain so there are no surprises, no hidden agendas, and no confusing jargon. When a client understands what’s happening and why, it returns a sense of control that trauma so often strips away.
This principle is all about clear, consistent, and open communication at every single stage of the client’s journey.
- Intake and Onboarding: An intake coordinator should do more than just hand over a clipboard of forms. They can take five minutes to walk a new client through exactly what to expect in their first few appointments, who they’ll meet, and what the purpose of each step is. Simple, but it makes a world of difference.
- Defining the Relationship: From the very first session, a therapist needs to clearly explain the limits of confidentiality. Discussing when information must be shared (like a risk of harm to self or others) isn't just a legal formality; it's a profound act of respect and honesty.
- Explaining Decisions: When a clinician recommends a specific therapy group or a change in medication, they should explain their reasoning in plain language. This isn't about justifying their expertise; it's about inviting the client into the decision-making process as an informed, respected partner.
By making every part of the process predictable and clear, you actively fight against the chaos and uncertainty that define traumatic experiences.
Trust is built in drops and lost in buckets. In trauma-informed care, every transparent conversation, every kept promise, and every moment of consistent follow-through adds a crucial drop to the foundation of a healing relationship.
Why This is Essential for Healing
When your team operates with genuine transparency, the entire power dynamic shifts. You move away from that old, tired model where the clinician is the all-knowing expert and the client is just a passive recipient of care. It fosters a real, collaborative partnership where the client feels respected, heard, and valued.
This approach directly repairs the deep-seated expectation of betrayal. When a client learns that their provider will actually do what they say they will do—call back when they promise, have the paperwork ready, follow up on a question—it creates a powerful corrective emotional experience. They begin to learn that it might just be possible to rely on someone, to be vulnerable without being harmed, and to trust again.
This foundation of trust isn't just a "nice-to-have." It's the very ground upon which all other therapeutic work is built. Without it, clients may stay guarded, withhold critical information, or just disengage from treatment entirely. By prioritizing trustworthiness and transparency, we create the conditions that allow a client to finally become a true, empowered partner in their own recovery.
Integrating Peer Support and Lived Experience
While safety and trust build the foundation for healing, this next principle introduces a uniquely powerful element: the voice of someone who has walked the same path. Clinical expertise is absolutely vital, but sometimes the most profound healing comes from hearing the simple, life-changing words, "I've been there, too."
This is the heart of peer support. It’s a mutual relationship between people who share similar experiences with trauma, mental health challenges, or addiction recovery. It’s not a traditional therapeutic dynamic. Instead, it levels the playing field, creating a powerful connection through shared humanity rather than a hierarchy of knowledge.
For someone who feels utterly alone, convinced no one could possibly understand their story, connecting with a peer is immediate proof that they aren’t isolated. That connection can instantly dissolve shame and crack the door open to hope.
The Unique Power of Shared Humanity
A therapist provides essential guidance, clinical insight, and evidence-based tools. A peer support specialist, however, offers something different but equally valuable: a living, breathing example of resilience. They are tangible proof that recovery isn't just possible, but achievable.
Think of it this way: a mountain guide (the therapist) can give you a map, show you the safest routes, and teach you how to use your equipment. But a fellow hiker who has already climbed that same treacherous mountain (the peer) can tell you where the loose rocks are, how it feels to finally reach the summit, and offer encouragement when you feel like turning back.
Both roles are indispensable. By integrating peer navigators or recovery coaches into outpatient addiction and mental health settings, we bring this dynamic directly into the care model.
Peer support is the embodiment of hope. It transforms recovery from an abstract concept discussed in therapy into a real, attainable future that a client can see and connect with on a human level.
This approach validates a person's experience in a way that clinical support sometimes cannot, making them feel deeply seen and understood.
Integrating Peer Support in Outpatient Care
Bringing peer support into a clinical setting is about more than just starting another support group. It means thoughtfully weaving individuals with lived experience into the very fabric of the care team, creating a more rounded and compassionate environment for everyone.
Here’s how this principle is put into action:
- Peer Navigators: These specialists can help new clients navigate the often-overwhelming process of starting treatment. Having someone who has been through it explain what to expect can dramatically reduce anxiety and improve engagement from day one.
- Recovery Coaching: A recovery coach with lived experience works alongside a client to set realistic goals, build coping skills, and find community resources. They act as a mentor, an ally, and a source of practical, real-world wisdom.
- Co-Facilitating Groups: When a clinician and a peer specialist lead a group together, they create a powerful blend of clinical knowledge and relatable experience. The peer can offer insights and perspectives that resonate deeply with group members.
This principle is also crucial in broader social systems, such as child welfare. Experts emphasize that success should not be measured solely by the number of children entering or exiting foster care, but by reducing maltreatment rates and shortening time spent outside a permanent family. Trauma-informed principles stress that comprehensive support for these children and families must include emotional safety, trust-building, and healing from past adversities. You can discover more insights about foster care and adoption statistics on adoptioncouncil.org.
Ultimately, integrating peer support is a formal recognition that lived experience is a valid and vital form of expertise. It doesn't just talk about the path forward—it illuminates it, showing that healing is not just a clinical goal but a shared human journey.
Fostering Collaboration and Mutuality
If you've spent any time in traditional healthcare, you know the script. The clinician is the expert, holding the map, and the client is expected to follow the directions. But one of the most important trauma-informed care principles flips that script entirely. It's about dismantling that old hierarchy.
Fostering collaboration and mutuality means we stop talking at clients and start working with them. It’s a move from a top-down directive to a side-by-side partnership.
This whole idea rests on a simple, powerful belief: the client is the ultimate expert on their own life. They carry the wisdom of their experiences—their strengths, their fears, their hopes. The clinician brings essential tools and guidance, absolutely, but the healing journey is a shared project, not a prescription to be filled.
It turns the one-way flow of information into a genuine conversation. It's about honoring a client's power to heal themselves, because you can't force lasting change on someone from the outside.
From Directive to Dialogue
In real life, this shift from a "telling" model to an "asking" model changes everything about how we interact with clients. It’s the difference between creating a treatment plan for someone versus building one with them.
This is huge. For someone whose power was taken away by trauma, being in a setting where the power dynamic feels lopsided can be inadvertently re-traumatizing. Leveling that dynamic is essential.
Just look at the language:
- The Old Way: "Here is your treatment plan. You need to attend these three groups and see your therapist once a week."
- A Collaborative Way: "Based on the goals we've discussed, here are a few options that might be helpful. Let's talk through them. What feels like the right next step for you?"
That small change in wording sends a massive signal. It communicates respect for the client’s autonomy and invites them to be an active architect in their own recovery.
What Mutuality Looks Like in Practice
Mutuality pushes collaboration even further. It's the recognition that healing is a two-way street; both the provider and the client learn and grow from working together. The clinician isn't some untouchable authority but a real person engaged in a meaningful relationship. This doesn't mean blurring professional boundaries—it means enriching them with authenticity.
Mutuality recognizes that every interaction holds the potential for shared learning. A clinician learns about resilience from a client's story, and the client learns new coping skills, creating a partnership where both individuals are enriched by the process.
This principle is mission-critical in settings that deal with complex, overlapping issues. For clients with co-occurring disorders, a collaborative approach ensures that both their mental health and substance use challenges are addressed with equal weight, guided by their own priorities. You can see more about how this works in our discussion of dual diagnosis outpatient treatment.
By leveling the power dynamic, you create a space where clients feel safe enough to share their real concerns and take ownership of their care. This partnership taps into their unique strengths and wisdom, transforming the therapeutic relationship into a powerful engine for navigating recovery, together. It’s a fundamental shift from treating a condition to partnering with a person.
Empowering Through Voice and Choice
Trauma, at its core, is an experience of profound powerlessness. It rips away a person's sense of control, their agency, and the belief that their voice even matters. That’s why one of the most vital trauma informed care principles is all about actively restoring that power through empowerment, voice, and choice.
This principle forces us to reframe every single interaction. Each conversation, decision, and moment of care becomes an opportunity—we can either reinforce a feeling of helplessness or we can intentionally build up a client's autonomy. It’s a fundamental shift away from a system that values simple compliance and toward a mission of cultivation. We are cultivating a client's capacity to advocate for themselves.
The end goal is to help them reclaim authorship of their own life story, moving from a passive role defined by past events to an active one shaped by their present choices.
This Is More Than Just Scheduling Preferences
When we talk about providing choice, it goes far beyond asking about preferred appointment times. Meaningful choice means embedding autonomy into the very fabric of the therapeutic process. It's about recognizing and honoring the client's inherent right to self-determination in their own healing journey.
In an outpatient addiction and mental health setting, this can look like many different things:
- Offering Treatment Options: Instead of just assigning someone to a therapy group, a clinician might present a few different modalities. They could explain the focus of a Cognitive Behavioral Therapy (CBT) group versus a mindfulness-based one, letting the client select the path that truly resonates with them.
- Co-Creating Goals: Treatment planning becomes a collaborative dialogue, not a top-down directive. The clinician brings their expertise, but the client brings their lived experience. The conversation shifts from, "Here are your goals," to, "What matters most to you right now, and how can we work toward that together?"
- Respecting the Right to Say 'No': True empowerment means honoring a client's decision to decline a suggestion or express discomfort. This simple act validates their boundaries and teaches them that their voice will be respected, not overridden—a crucial corrective experience for many trauma survivors.
Building Autonomy Through Active Listening
Here's the thing: empowerment isn't something a provider can just "give" to a client. It's something we help a client rediscover within themselves. This process is fueled by active listening and a genuine strengths-based perspective. When a provider truly listens to a client’s point of view, validates their feelings, and points out their inherent strengths, they hold up a mirror reflecting the client's own resilience.
Empowerment is the process of helping individuals recognize the strength and agency they already possess. It’s about shifting the focus from deficits to capabilities, allowing clients to see themselves as resourceful survivors rather than just victims of circumstance.
This approach lines up perfectly with techniques used in motivational interviewing, which is all about drawing out a person's own motivation and commitment to change. You can explore this powerful connection further in our guide to motivational interviewing therapy. By building on what the client themselves identifies as important, we reinforce their role as the primary agent in their own recovery.
The research backs this up, time and time again. Specific, targeted trauma-informed interventions built on these principles yield significant results. For example, models like Trust-Based Relational Intervention (TBRI) have shown measurable reductions in trauma symptoms. Studies have documented that children undergoing TBRI showed significant decreases in trauma symptoms on validated scales, unlike control groups. To learn more about these findings, you can read the full research about trauma symptom reduction. By giving clients a real voice and meaningful choices, we don’t just offer better care—we help them rebuild the very foundation of self-trust and personal power.
Putting Trauma-Informed Principles into Practice
Theory gives you the roadmap, but practice is where the real journey begins. To see how all six trauma-informed care principles actually work together, let’s walk through the first few moments of a client’s experience at a clinic that truly gets it. We’ll call him Alex.
This isn’t just a story. It’s a blueprint for what compassionate, effective care looks like on the ground.
When Alex first calls the clinic, he’s not met with a rushed, scripted voice. Instead, the person on the other end is calm and unhurried, walking him through the intake process step-by-step. This simple act of Transparency dials down his anxiety right away.
When he arrives for his first appointment, the waiting room is quiet and the lighting is soft. He’s offered a choice of where to sit—a small gesture, but a meaningful signal of Empowerment and control.
The First Session: A New Experience
During the intake session, the clinician, Maria, doesn't jump into a sterile checklist of diagnostic questions. She starts the conversation by saying, "We’re going to go at your pace. You are in control of this conversation." With that single statement, she establishes Psychological Safety and hands the power back to Alex.
Maria explains the clinic’s services and what Alex can expect, reinforcing Trustworthiness. Then she asks a question that shifts the entire dynamic: "What would feel most helpful for you to focus on first?" This is the heart of Collaboration, treating Alex as the expert on his own life from the very beginning.
This approach moves away from a clinical assessment focused on "What's wrong with you?" and into a human-centered conversation guided by "What happened to you, and what do you need to feel supported?"
It's a subtle shift in language, but it completely changes the therapeutic relationship, building a genuine partnership from moment one.
Building a Plan Together
Together, Alex and Maria co-create an initial care plan. Maria doesn't dictate; she presents options. She explains individual therapy, a skills-based group, and a group led by a peer specialist, letting Alex make an informed Choice.
Alex is drawn to the peer-led group. The idea of connecting with others who have been through similar struggles resonates with him. This integration of Peer Support immediately validates his experience and offers a tangible source of hope that he’s not alone.
Throughout their talk, Maria is mindful of Alex's cultural background and identity. She asks questions that honor his unique perspective, showing a real commitment to addressing Cultural, Historical, and Gender Issues. The care isn't just informed by trauma in general, but by the whole person sitting in front of her.
From that first phone call to the final treatment plan, every single touchpoint is intentional. Alex leaves his first appointment feeling not like a patient with a diagnosis, but like a respected partner in his own recovery. This is what it looks like when trauma-informed care moves from a checklist to a living, breathing culture of healing.
At Altura Recovery, we don't just talk about these principles—we live them. Our outpatient programs are built on a foundation of safety, trust, and collaboration, providing a path to lasting recovery. If you or a loved one is ready to take the next step, visit us at https://www.alturarecovery.com to learn how we can support your journey.