Dual diagnosis outpatient treatment offers a way to tackle both a mental health disorder and a substance use disorder at the same time, without having to put life on pause. It’s a framework that provides structured therapy and support while you continue to live at home, stay connected to your job, and be there for your family. This model is absolutely essential for untangling the deeply interconnected nature of these co-occurring conditions.
Understanding Integrated Treatment for Dual Diagnosis
Imagine trying to fix a leaky pipe but completely ignoring the dangerously high water pressure that’s causing it. You can patch one leak, sure, but another one is bound to spring up somewhere else. This is a perfect picture of what it’s like to treat substance use without addressing an underlying mental health issue, or vice versa. When these two issues exist together, it's called a dual diagnosis, or co-occurring disorder.
For years, treatment systems were completely siloed. A person might see one specialist for their depression and go to a totally separate program for their drinking. This fragmented approach created huge roadblocks, forcing people to navigate two different—and often conflicting—paths to get well. You can learn more about this historical challenge from research on integrated care models.
Integrated treatment completely flips that outdated model on its head. It’s one unified approach where a single team of professionals addresses both conditions at the same time, under one cohesive plan.
The Interconnected Cycle of Co-Occurring Disorders
The relationship between mental health and substance use is almost always a complex, self-fueling cycle. Someone with chronic anxiety, for example, might start using a substance to quiet their racing thoughts and find a moment of peace. Over time, this self-medication can spiral into dependence, and the substance itself can actually make the original anxiety even worse.
On the flip side, heavy substance use can trigger or intensify the symptoms of a mental health condition like depression or bipolar disorder. Breaking this cycle requires a treatment philosophy that sees and addresses this deep-rooted connection.
An integrated approach acknowledges that you can't effectively treat one condition while the other runs wild. Lasting recovery depends on healing the whole person, not just patching up isolated symptoms.
Key Principles of an Integrated Approach
A quality dual diagnosis outpatient treatment program is built on a few core principles. These pillars work together to create an environment where real, sustainable recovery can happen.
- Simultaneous Treatment: This is the big one. Both the mental health disorder and the substance use disorder are addressed at the same time, by the same clinical team. No more bouncing between appointments.
- Personalized Care Plans: Treatment is never one-size-fits-all. A good plan is tailored to meet the specific psychological, biological, and social needs of each person.
- Long-Term Perspective: The goal isn't just about getting sober for a few weeks. The focus is on building durable coping skills that support lifelong mental and emotional wellness.
- Evidence-Based Therapies: Programs should use proven methods like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT). These aren't just buzzwords; they provide practical tools for managing thoughts, feelings, and behaviors.
This modern, holistic method provides a much stronger foundation for getting better. By untangling the threads of both conditions together, people can achieve not just sobriety, but genuine mental stability and a far better quality of life.
Understanding Levels of Outpatient Care
Deciding to seek help for a dual diagnosis is a huge first step, but recovery doesn’t follow a one-size-fits-all map. Just like a doctor prescribes different levels of care for a physical illness, dual diagnosis outpatient treatment is built on different levels of intensity. This approach ensures you get the right amount of support exactly when you need it.
Think of it like the recovery process after a major surgery. You start with more intensive care and, as you heal and get stronger, you gradually step down to greater independence. This method allows for a safe, steady return to daily life while keeping a strong therapeutic safety net firmly in place.
Each level of care—Partial Hospitalization, Intensive Outpatient, and Standard Outpatient—comes with its own time commitment, structure, and ideal patient profile. Getting clear on these differences is the key to finding the right starting point for your own journey.
Partial Hospitalization Programs (PHP)
The highest and most structured tier of outpatient care is the Partial Hospitalization Program (PHP). It’s designed to bridge the gap between 24/7 residential treatment and less intensive outpatient options. A PHP provides a highly structured therapeutic environment during the day, but you get to return home each evening.
This model works incredibly well for people who need significant daily support and medical oversight but have a stable and supportive home to go back to. It’s often a critical step down for those leaving a residential program or for anyone who needs more structure than an IOP can offer to prevent a relapse.
- Time Commitment: Usually 5 days a week for 4-6 hours per day.
- Therapeutic Structure: A packed schedule of individual therapy, group sessions, psychiatric check-ins, and medication management.
- Best Suited For: Individuals who need daily medical and clinical oversight but don’t require 24/7 supervision.
Intensive Outpatient Programs (IOP)
Taking a step down from PHP, the Intensive Outpatient Program (IOP) delivers a powerful level of care with a lot more flexibility. This is one of the most common and effective formats for dual diagnosis treatment because it allows you to keep up with work, school, or family life.
An IOP gives you a solid foundation of therapy and skill-building while pushing you to apply those new coping strategies in your real-world environment. This immediate, real-time application helps cement what you learn in sessions, making the transition to full independence feel much smoother.
An IOP strikes a critical balance. It delivers the therapeutic intensity needed to address complex co-occurring disorders while empowering individuals to remain connected to their daily lives and responsibilities.
According to a national survey, 82% of U.S. treatment facilities offered some form of outpatient program in 2020. Finding specialized care is the real challenge, as less than half (45%) provided intensive outpatient treatment properly equipped to handle the complexities of a dual diagnosis.
Standard Outpatient Programs (SOP)
The most flexible level of care is the Standard Outpatient Program (SOP). This is often the final phase in a step-down treatment plan. It can also serve as a starting point for individuals who have less severe symptoms and a strong, reliable support system already in place.
SOPs are all about maintaining the progress you’ve made in more intensive programs and tackling ongoing challenges as they pop up. Sessions are less frequent, which allows for maximum autonomy while still providing that vital connection to professional support.
This infographic shows the core benefits that make outpatient treatment such an effective and accessible option for so many people.
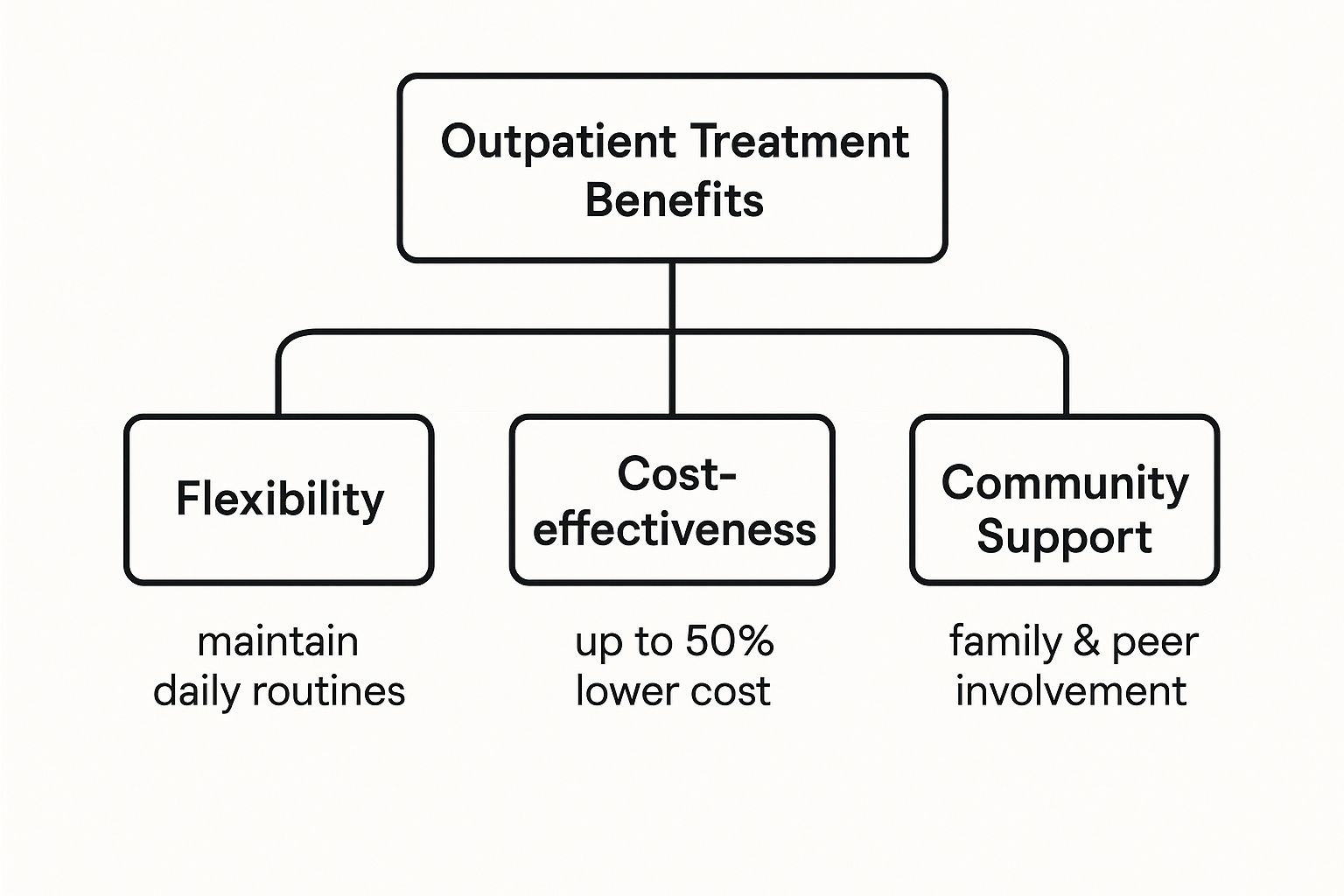
It really highlights how flexibility, affordability, and the ability to stay connected to your community all work together to create a sustainable path to recovery.
Seeing how these levels of care stack up against each other can help you figure out which program might be the right fit. The table below breaks down the key differences at a glance.
Comparing Dual Diagnosis Outpatient Program Levels
| Feature | Partial Hospitalization (PHP) | Intensive Outpatient (IOP) | Standard Outpatient (SOP) |
|---|---|---|---|
| Time Commitment | 20-30 hours per week | 9-15 hours per week | 1-3 hours per week |
| Typical Schedule | 5 days/week, 4-6 hours/day | 3-5 days/week, 3 hours/day | 1-2 sessions/week |
| Primary Goal | Stabilize acute symptoms & build foundational skills | Reinforce skills & integrate recovery into daily life | Maintain progress & provide long-term support |
| Ideal Candidate | Stepping down from inpatient or at high risk of relapse | Needs structure but must maintain work/school | Has strong coping skills & a stable environment |
| Medical Oversight | Regular psychiatric & medical check-ins | As-needed psychiatric & medication management | Primarily therapeutic; medical care is separate |
While this guide gives you a solid overview of the landscape, it’s important to understand all the nuances of what rehab truly involves. You can get a deeper understanding by reading our article on what is rehab. Ultimately, each program offers a unique structure tailored to different recovery needs, ensuring you can find the path that works for you.
Core Therapies in Dual Diagnosis Treatment
Real dual diagnosis outpatient treatment isn't just about talking through problems. It’s about building a toolkit of practical, real-world skills to manage both mental health symptoms and substance use triggers at the same time. The foundation of this work is evidence-based therapy—structured, proven methods that create lasting change.
Think of it like learning to play an instrument. You don't just pick it up and play a symphony. You start with the basic scales (identifying negative thoughts), then practice chords (challenging those thoughts), and eventually, you can improvise during a tough moment (managing a high-stress situation without turning to a substance). This is exactly how recovery skills are built: step-by-step, with consistent practice in a supportive setting.
Unpacking Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy, or CBT, is one of the most trusted and effective tools in dual diagnosis care. It works on a simple but profound idea: our thoughts, feelings, and behaviors are all linked. By learning to change destructive thought patterns, we can directly change our emotional responses and, ultimately, our actions.
For someone dealing with social anxiety and an alcohol use disorder, a CBT session might zero in on a specific fear, like going to a company party sober. The therapy helps them catch that automatic negative thought—"Everyone will think I'm boring"—and then systematically dismantle it with logic and evidence. Over time, this practice actually rewires the brain’s response, making healthier choices feel more natural and less like a battle.
CBT provides a roadmap to understanding the relationship between thought and action. It empowers you to become a detective of your own mind, identifying and dismantling the cognitive traps that fuel both addiction and mental health struggles.
Building Skills with Dialectical Behavior Therapy (DBT)
While CBT is fantastic for changing thought patterns, Dialectical Behavior Therapy (DBT) adds another crucial layer: acceptance and emotional regulation. DBT is a game-changer for people who experience intense, overwhelming emotions, which is incredibly common in dual diagnosis. It teaches concrete skills across four key areas, giving you a sturdy framework for handling life’s inevitable distress.
- Mindfulness: This is about learning to stay in the present moment, observing your thoughts and feelings without judging them. This skill creates that critical pause between feeling a trigger and reacting impulsively.
- Distress Tolerance: Think of this as your emotional first-aid kit. It’s a set of strategies for getting through a crisis without making things worse—practical, in-the-moment tools for surviving emotional pain when it feels unbearable.
- Emotion Regulation: Here, you learn to understand your emotions and dial down their intensity. This module helps you build a more balanced emotional life, reducing the need to self-medicate with substances.
- Interpersonal Effectiveness: This is all about building better relationships. You’ll learn skills to communicate your needs clearly, set healthy boundaries, and navigate conflict, which helps repair connections and build a stronger support system.
A Day in the Life of an IOP Patient
So, how do all these therapies come together? Let’s look at a typical afternoon for someone in an Intensive Outpatient Program (IOP). The whole experience is structured to reinforce these new skills through a mix of individual work and group support.
Their day might kick off with a group therapy session focused on DBT, where a therapist leads a discussion on distress tolerance techniques. Right after, they could have a one-on-one counseling session to apply CBT methods to a personal challenge, like mapping out a plan to handle a specific craving. The day might wrap up with a skills-building workshop on healthy communication, giving them a safe space to practice what they've learned with their peers.
Each part of the program is designed to build on the others, creating a cohesive and powerful healing experience. This integrated approach is what makes a high-quality dual diagnosis outpatient treatment so effective. It ensures that recovery is happening on every level—cognitive, emotional, and relational.
Is Outpatient Treatment the Right Fit for You?
Choosing the right level of care is one of the most critical decisions you'll make on the road to recovery. Dual diagnosis outpatient treatment is a powerful and flexible option, but its success hinges on whether it truly matches your current needs. An honest look at your situation is the key to finding a path with enough support to keep you safe without being more restrictive than necessary.
Think of it like building a bridge to your new life. You need the right materials and support structures to make sure it holds up under pressure. For many, outpatient care provides that perfect balance, letting them rebuild their lives while staying connected to work, family, and community.
Who Is an Ideal Candidate for Outpatient Care?
Outpatient treatment works best for people who have a stable foundation and a genuine motivation to get better. While everyone's journey is different, strong candidates for programs like an IOP or PHP tend to share a few key traits. These factors create the support system needed to heal and grow outside of a 24/7 residential facility.
Ask yourself if these points describe your current situation:
- A Stable and Supportive Home Life: Your living environment is safe, sober, and free from major triggers. You have family or friends who are actively cheering you on.
- Medical and Psychological Stability: You aren't facing an acute medical crisis, severe withdrawal that requires medical detox, or a psychiatric emergency (like being a danger to yourself or others).
- A Foundation of Motivation: You have a real desire to show up, do the work, and be accountable for your recovery.
- The Ability to Manage Daily Responsibilities: You can handle basic life tasks and are able to structure your time to prioritize treatment sessions alongside your other commitments.
This isn't about being "strong enough" for outpatient care. It's about matching the level of clinical support to your current needs to create the safest, most effective environment for healing.
Signs a Higher Level of Care May Be Needed
Just as it’s vital to know who thrives in outpatient treatment, it’s equally important to recognize when a more intensive setting is the right call. Inpatient or residential treatment offers a highly structured, 24/7 environment that removes you from daily stressors, allowing you to focus completely on your health. For some, this is the safest and most effective place to start.
Be honest with yourself. A higher level of care might be the best first step if you’re experiencing any of these challenges:
- An Unsafe or Triggering Home Environment: Trying to recover in a home where substance use is common or relationships are chaotic can feel like swimming against a current.
- Severe Co-Occurring Disorders: If your mental health symptoms are intense, unstable, or require close medical supervision, a residential setting provides that necessary round-the-clock oversight.
- A History of Relapse: If you've tried outpatient programs before and struggled to stay sober, the immersive structure of an inpatient program could provide the breakthrough you need.
- Lack of a Sober Support System: Without a reliable network of supportive friends or family, the isolation of early recovery can be overwhelming. Residential treatment helps you build that community from day one.
Making this decision takes some real self-reflection. An admissions coordinator or a mental health professional can walk you through a thorough assessment to help guide you to the right level of dual diagnosis outpatient treatment or recommend a higher level of care if it’s a better fit.
How to Choose the Best Dual Diagnosis Program

Finding the right dual diagnosis outpatient treatment can feel like searching for a needle in a haystack, especially when you’re already feeling overwhelmed. But with the right checklist, you can confidently sort through your options and find a program that offers genuine, integrated care—not just a center that treats symptoms, but one that addresses the whole person.
Think of it like hiring a specialist to fix a complex problem with your home’s foundation. You wouldn’t just call a general handyman. You’d want an expert with the right credentials, proven methods, and a clear plan. That same level of diligence is critical when you're choosing a provider who will guide you toward lasting recovery.
Start with the Non-Negotiables
Before you even get into the details of a program, a few foundational elements have to be in place. These are the absolute deal-breakers. Verifying them first will save you a ton of time and keep you focused on high-quality options right from the start.
- Proper Licensing and Accreditation: The program absolutely must be licensed by the state. Ideally, it should also be accredited by a national body like The Joint Commission or CARF, which means they meet rigorous standards for safety and quality care.
- Certified Dual Diagnosis Staff: The clinical team needs professionals who are certified and experienced in treating both mental health and substance use disorders at the same time. Don’t be afraid to ask if their therapists, psychiatrists, and counselors have specific credentials in co-occurring conditions.
- Use of Evidence-Based Therapies: A quality program builds its entire curriculum around proven therapeutic models. Look for names like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Eye Movement Desensitization and Reprocessing (EMDR).
Questions to Ask an Admissions Coordinator
Once you’ve confirmed the basics, it’s time to get a feel for how the program actually runs. Your first phone call with an admissions coordinator is a golden opportunity to ask pointed questions that reveal the true quality and philosophy of their care. This conversation can tell you everything you need to know.
Truly integrated care is still surprisingly rare. A 2014 study found that only 18% of addiction treatment programs and 9% of mental health programs were truly equipped for dual diagnosis care, meaning most treated these issues separately. These findings underscore the importance of asking direct questions to ensure a program offers truly comprehensive support. Learn more about the challenges in finding integrated care.
Here are the key questions that will help you gauge a program's effectiveness and its commitment to your individual recovery:
- How do you create individualized treatment plans? You're listening for an answer that involves a comprehensive initial assessment and regular updates based on your progress—not a one-size-fits-all curriculum they push everyone through.
- What does family involvement look like? Effective treatment always recognizes the role of the family system. Ask about family therapy sessions, educational workshops, and other resources designed to heal relationships and build a strong support network back home.
- What kind of aftercare planning and support do you offer? Recovery doesn’t stop the day you finish the program. A great center will help you build a detailed aftercare plan, connecting you with support groups, therapists, and community resources to ensure a smooth transition.
- How is progress measured and communicated? There should be a clear process for tracking clinical milestones and adjusting your treatment plan as needed. Most importantly, you should be an active participant in those conversations.
Understanding the mechanics of treatment is also essential for setting realistic expectations. For a clearer picture of the entire process, from intake to aftercare, explore our detailed guide on how rehab works. This broader context can help you frame your questions and better understand the answers you receive. Making an informed choice is your first major step toward building a sustainable foundation for recovery.
Common Questions About Outpatient Treatment
Making the decision to get help is a huge first step, but it almost always kicks off a wave of new questions. When you start looking into dual diagnosis outpatient treatment, the options can feel a little overwhelming. Getting straight answers is the best way to move forward with confidence.
Think of this section as your practical guide. We’re tackling the most common questions people ask when they're considering an outpatient program, breaking down the logistics and expectations so you know exactly what to expect.
How Long Does Dual Diagnosis Outpatient Treatment Last?
This is usually the first question on everyone's mind. Unlike a college semester, treatment doesn’t run on a fixed calendar. Instead, the length of your program is tailored to your personal progress and clinical needs. It's a dynamic process, not a rigid one.
Most high-quality programs use a step-down model. You’ll likely start with more intensive care and gradually move to less frequent sessions as you gain new skills and feel more stable.
- Partial Hospitalization (PHP): This is the highest level of outpatient care. It usually lasts for several weeks, giving you a strong, structured foundation before you transition to a more flexible program.
- Intensive Outpatient (IOP): Most people are in an IOP for about 8 to 12 weeks. This phase is all about learning to apply your recovery skills to the challenges of everyday life.
- Standard Outpatient (SOP): This is a longer-term support phase that can go on for several months, or even longer if needed, to help you maintain your momentum and troubleshoot challenges as they arise.
A good program will constantly check in on your progress and adjust your care plan as you go. The whole point is to make sure you have a rock-solid set of coping skills and a reliable support system before you finish.
Does Insurance Cover Dual Diagnosis Treatment?
Cost is a real and valid concern for most families. The short answer is yes—the vast majority of major health insurance plans cover treatment for co-occurring disorders. We can thank laws like the Mental Health Parity and Addiction Equity Act (MHPAEA) for that.
This federal law mandates that insurance plans can't be more restrictive with coverage for mental health and substance use than they are for medical or surgical care. It’s been a game-changer for making treatment more accessible.
While coverage is required by law, the details are in your specific plan. Things like your deductible, copayments, and out-of-pocket maximum will be different for everyone. It's crucial to verify your benefits directly with your insurance company or have the treatment center's admissions team handle it for you. This one step can save you from any financial surprises.
Many insurance plans also require pre-authorization before you start. A reputable treatment center will have a team that knows exactly how to handle this, taking care of the paperwork so you can put all your energy into getting better.
Can I Still Work or Go to School?
Yes, absolutely. In fact, this is one of the biggest benefits of dual diagnosis outpatient treatment. The entire model is designed for flexibility, allowing you to get the intensive clinical care you need without pressing pause on your entire life.
Programs are intentionally built to fit around real-world schedules. Many centers offer IOP and SOP groups during both the day and evening. This structure means you can attend your therapy sessions and still keep up with your commitments at work, school, or home.
This isn’t just about convenience—it’s a core therapeutic advantage. It gives you a chance to immediately use the skills you’re learning. You can face a stressful day at the office or a tough conversation with family, then process that exact experience with your therapist and peers just a few hours later.
While a PHP schedule is more demanding and can make full-time work tricky, it's a short-term commitment. The goal is always to help you stabilize and then step down to a level of care that fits seamlessly into your life.
What Is the Difference Between Individual and Group Therapy?
A solid outpatient program will always use a powerful blend of individual and group therapy. They aren't interchangeable; they each play a unique and vital role in building a well-rounded recovery.
Individual Therapy is your private, one-on-one time with a therapist. This is the space where you can safely dig into deeply personal topics—things like past trauma, specific anxieties, or family issues you might not be ready to talk about in a group setting. It's where the highly personalized work on the root causes of your conditions happens.
Group Therapy is all about connection and community. You'll join a small group of peers who are also figuring out how to manage a dual diagnosis. It’s an incredibly powerful tool for breaking through the shame and isolation that addiction and mental health struggles thrive on.
In a group setting, you can:
- Share what you're going through and realize you’re not alone.
- Hear different perspectives from people who get it.
- Practice new communication and relationship skills in a safe space.
- Build a sober support network that can last a lifetime.
Using both is the gold standard for dual diagnosis outpatient treatment. Individual therapy offers the depth, while group therapy provides the community and real-world practice you need for lasting change.
What Role Does Medication Play in Treatment?
Medication can be an essential piece of the puzzle, but it’s always used to support therapy, never as a standalone fix. For many people, medication helps stabilize brain chemistry, which in turn makes it possible to show up and get the full benefit of counseling. For a deeper look at this, you can learn more about what medication-assisted treatment entails.
The process usually starts with a detailed psychiatric evaluation to see if medication is a good fit. If so, a psychiatrist or doctor will manage your prescriptions, keeping a close eye on how they’re working and adjusting as needed. This integrated approach ensures your mental and physical health are treated together, as a whole.
At Altura Recovery, we know that no two recovery paths are the same. Our compassionate team of dually certified clinicians is here to provide personalized outpatient care that addresses the whole person. We offer flexible schedules, evidence-based therapies, and a supportive community to help you build a foundation for real healing and lasting freedom. Contact us today to learn how we can support you.