Integrated dual diagnosis treatment is the modern, effective solution that treats both substance use and mental health disorders at the same time, viewing them as interconnected parts of a whole person. This unified approach moves beyond treating symptoms in isolation to create a single, cohesive strategy for a recovery that actually lasts.
Decoding Integrated Dual Diagnosis Treatment

Imagine trying to fix a car's engine and its electrical system separately, without ever acknowledging how they work together. You might fix one part, only for the other to cause a new problem a week later. That’s the challenge of treating mental health and substance use in isolation—an outdated approach that often leads to frustration and relapse.
The core idea of integrated dual diagnosis treatment is simple but profound: mental health and substance use aren't two separate problems, but two sides of the same coin. This model rejects the fragmented care of the past, where someone was often told to get sober before they could get help for their anxiety or depression.
A Unified and Cohesive Strategy
This approach creates a single, cohesive strategy where every therapy and intervention addresses the complex dance between mental health and addiction. Instead of two separate teams working in different locations with different philosophies, one multidisciplinary team collaborates on a single treatment plan.
This unified team typically includes:
- Psychiatrists who can manage medications for both mental health symptoms and cravings.
- Addiction Counselors who understand the psychological drivers of substance use.
- Therapists specializing in modalities like CBT or DBT to teach new coping skills.
- Case Managers who help coordinate care and address practical needs like housing or employment.
By working together, this team ensures that progress in one area supports progress in the other. It prevents the all-too-common scenario where untreated depression triggers a substance use relapse, or vice-versa.
Moving Beyond Parallel Services
It’s important to distinguish true integration from programs that simply offer separate services under one roof. True integrated care means the same clinicians are trained to address both conditions in the same sessions.
For instance, a therapy session might explore how panic attacks (mental health) lead to alcohol use (substance use) and then teach skills to manage the panic without drinking. This is fundamentally different from seeing one therapist for anxiety and another one, down the hall, for addiction.
Before integrated care became the standard, individuals with co-occurring disorders were often bounced between separate systems, leading to gaps in care and poorer outcomes. This table shows the key differences.
Comparing Treatment Models for Co-Occurring Disorders
| Feature | Sequential or Parallel Treatment | Integrated Dual Diagnosis Treatment |
|---|---|---|
| Philosophy | "Treat the addiction first, then the mental health." | "Treat both conditions simultaneously, as they are intertwined." |
| Treatment Team | Two separate teams (e.g., mental health clinic and an addiction center). | One cohesive, cross-trained team works together. |
| Plan of Care | Two separate, often conflicting, treatment plans. | A single, unified treatment plan addressing both issues. |
| Patient Experience | Fragmented, confusing, and often feels like a revolving door. | Holistic, person-centered, and feels seamless. |
| Outcomes | Higher rates of relapse, dropout, and hospitalization. | Improved engagement, better symptom management, and higher rates of recovery. |
The integrated model has proven far more effective because it reflects the reality of how these conditions truly function in a person's life.
An integrated approach acknowledges that healing isn't linear. It provides a flexible and compassionate framework that meets individuals where they are, addressing the intertwined roots of their struggles rather than just the visible symptoms.
This model is particularly effective in an outpatient setting. Many people benefit from understanding the structure of a dual diagnosis outpatient treatment program, which allows them to build recovery skills while still managing the demands of daily life. Ultimately, this approach is about treating the whole person, paving the way for a more resilient and sustainable recovery.
Why Integrated Care Is More Important Than Ever
The need for integrated dual diagnosis treatment isn't just some new trend in behavioral healthcare; it's a critical response to a public health challenge that’s getting more complex by the day. When a mental health condition like depression and a substance use disorder show up together, they don’t just sit side-by-side. They twist into a destructive, powerful cycle that can feel impossible to break.
Think of it like one condition acting as fuel for the other. Someone battling social anxiety might start leaning on alcohol to get through parties or meetings. But over time, that self-medication can spiral into an alcohol use disorder, which then cranks up their anxiety even higher. It’s a brutal feedback loop that traps them.
The Destructive Cycle of Co-Occurring Disorders
This vicious cycle makes the symptoms of both conditions far more severe. For instance, a person with bipolar disorder might misuse stimulants during a manic episode because of impulsivity, only to find their depressive episodes become deeper and last longer as a result. This toxic interaction makes recovery incredibly complicated.
When these conditions are treated separately, any progress made in one area is often erased by the untreated issue. Someone might successfully finish a detox program, but if their underlying trauma isn't addressed, the emotional pain will almost certainly trigger a relapse. This is exactly why a fragmented approach so often fails to deliver lasting change.
Individuals with a dual diagnosis often experience more severe clinical symptoms, poorer treatment outcomes, and higher risks of relapse compared to those with a single disorder. Addressing both issues simultaneously is not just beneficial—it is essential for sustainable healing.
The real-world consequences are stark. This cycle is directly linked to higher rates of hospitalization, legal trouble, unemployment, and homelessness. It puts an immense strain not just on the individual but on their families and the entire community, highlighting the urgent need for a better way forward.
A Necessary Evolution in Behavioral Healthcare
The number of people facing a dual diagnosis is staggering and continues to climb. Global data suggests that roughly 30-50% of individuals with severe mental illnesses also have a substance use disorder, a reality that makes treatment far more challenging. You can dive deeper into the research on the global impact of co-occurring disorders from the National Institutes of Health to see the sheer scale of the issue.
This data drives home a vital point: integrated care isn't a niche service for a select few. It represents a necessary evolution in how we approach behavioral health, designed to offer real, tangible hope to people caught between two tangled struggles. The goal is to create one unified path forward that breaks the cycle for good.
Benefits of Addressing Both Conditions Together
Treating co-occurring disorders at the same time, within a single cohesive program, produces far better outcomes. This approach is central to understanding what rehab is in the modern era, where the focus has shifted from fixing isolated symptoms to healing the whole person. By tackling both issues at once, individuals can:
- Learn Healthier Coping Mechanisms: Therapy teaches practical skills for managing anxiety or depression without turning to substances.
- Achieve Greater Stability: A coordinated medication plan can address psychiatric symptoms and substance cravings at the same time.
- Experience Reduced Relapse Rates: By treating the root causes fueling the addiction, the likelihood of relapse drops significantly.
- Build a Stronger Foundation for Recovery: A single, unified treatment team provides consistent support, preventing people from falling through the cracks between separate care systems.
Ultimately, integrated dual diagnosis treatment accepts the complex reality of human struggle. It provides a compassionate and effective framework that empowers people to reclaim their lives from the grip of both mental illness and addiction.
The Blueprint for Effective Integrated Treatment

A truly effective integrated dual diagnosis treatment program is built on a set of core principles that go way beyond just having different specialists in the same building. It’s a complete shift in philosophy—one that treats the whole person with a single, unified strategy. This blueprint ensures care isn't just coordinated, but also compassionate, flexible, and grounded in the messy realities of recovery.
Think of it like the difference between a bunch of talented musicians all playing their own songs in the same room versus a conductor leading an orchestra. A high-quality program acts as the conductor, making sure every part of the treatment—from therapy and medication to life skills—works in perfect harmony to create one clear path toward wellness.
Meeting People Where They Are
One of the most foundational principles is a stage-wise approach to treatment. This acknowledges a simple but critical truth: not everyone is in the same place on their recovery journey. Someone who is just beginning to contemplate change needs a totally different kind of support than a person actively working to prevent a relapse.
Instead of a rigid, one-size-fits-all plan, treatment is customized to match the individual’s readiness and motivation. This approach respects their autonomy and builds trust, making them a partner in their own recovery rather than just a passive recipient of care. That flexibility is absolutely key to keeping people engaged for the long haul.
Assertive Outreach and Continuous Engagement
Effective programs don’t just open their doors and wait for people to show up; they practice assertive outreach. This means the clinical team proactively and persistently engages with clients, especially during moments of crisis or when they start to pull away.
An integrated team understands that missed appointments or periods of struggle are part of the recovery process, not signs of failure. They respond with supportive follow-up, helping individuals reconnect with their treatment goals and reinforcing that they are not alone.
This principle is crucial for building a strong therapeutic bond. It sends a powerful message of unwavering support and helps people stay connected to care even when their motivation dips—a common and expected challenge for anyone with co-occurring disorders.
Comprehensive and Holistic Services
Healing doesn't happen in a clinical vacuum. A person's recovery is deeply tied to their environment and everyday life circumstances. That's why top-tier integrated dual diagnosis treatment provides comprehensive services that address the whole person, not just the diagnosis.
This often means rolling up our sleeves to help with the practical, real-world needs that can so easily derail recovery. These wrap-around services transform treatment from a purely clinical exercise into a tangible plan for building a stable, fulfilling life.
Key areas of support often include:
- Housing Assistance: Helping individuals find and keep a safe, stable, and sober-supportive place to live.
- Vocational Training: Providing guidance on finding a job, building a resume, and practicing interview skills to foster financial independence.
- Family Education and Therapy: Bringing loved ones into the process to heal damaged relationships and build a strong support network at home.
- Medical and Dental Care Coordination: Making sure physical health needs, which are often neglected during active addiction, are also addressed.
By tackling these interconnected issues head-on, the program removes major barriers to recovery and helps people build a solid foundation for their future.
Adopting a Long-Term Perspective
Finally, the most effective programs operate with a long-term perspective. Recovery isn't a 30-day event; it's a lifelong process of growth and management. Because of this, treatment is designed as a continuum of care that adapts over time as a person’s needs change.
This means that as someone becomes more stable, the intensity of services can be stepped down—moving from a partial hospitalization program to an intensive outpatient program, and eventually to supportive aftercare. This long-term view ensures that support is always there when new life challenges pop up, drastically reducing the risk of relapse and promoting sustainable well-being. This approach doesn't just equip people to get well; it equips them to stay well.
Proven Therapies That Power Integrated Recovery
Effective integrated dual diagnosis treatment isn’t based on guesswork. It’s built on a foundation of proven, evidence-based therapies that give people practical tools for getting better. These aren't just abstract theories discussed in a quiet room; they are the powerful, hands-on methods clinicians use to demystify recovery and empower you with real skills for lasting wellness.
Instead of just talking endlessly about problems, these therapies offer a clear roadmap for changing the thoughts, behaviors, and emotional responses that keep people stuck. They help untangle the complex knot of mental health symptoms and substance use, creating new, healthier ways to cope when life gets hard.
Cognitive Behavioral Therapy for Dual Diagnosis
Cognitive Behavioral Therapy (CBT) is a cornerstone of integrated treatment because it gets straight to the point: our thoughts, feelings, and actions are all connected. For someone with a dual diagnosis, that connection often creates a destructive feedback loop.
Think of it like this: a person with social anxiety has the thought, "I can't handle this party," which triggers intense feelings of panic. That panic then leads to the action of taking a drink to calm their nerves. It works for a moment, but in the long run, it just reinforces the idea that they can't cope without a substance, making the cycle stronger next time.
CBT works by helping people methodically break that cycle. You learn to:
- Identify Negative Thought Patterns: Become a detective of your own mind, spotting the automatic, distorted thoughts that fuel both the anxiety and the urge to use.
- Challenge and Reframe Thoughts: Actively question those negative thoughts. Are they 100% true? You then learn to replace them with more balanced and realistic perspectives.
- Develop New Behavioral Skills: Practice healthier strategies for managing stress and difficult situations without reaching for a substance.
By systematically severing the link between anxious thoughts and self-defeating behaviors, CBT equips people with the practical tools to regain control.
Dialectical Behavior Therapy for Emotional Regulation
Dialectical Behavior Therapy (DBT) is another powerhouse, especially for individuals who feel like their emotions are constantly overwhelming them. While originally developed for borderline personality disorder, its skills are incredibly effective for anyone struggling with the kind of emotional dysregulation so common in dual diagnosis.
DBT provides a framework for building a life you actually want to live by teaching four key skill sets:
- Mindfulness: Learning to observe your thoughts and feelings without judging them, helping you stay grounded in the present moment instead of getting swept away.
- Distress Tolerance: Building skills to get through a crisis without making things worse through impulsive actions, like using a substance.
- Emotion Regulation: Understanding where your emotions come from and learning how to change unwanted emotional responses.
- Interpersonal Effectiveness: Gaining the ability to communicate your needs clearly, set boundaries, and manage relationships in a healthy way.
For someone with a co-occurring disorder, these skills are life-changing. They offer concrete, reliable alternatives to using substances when faced with emotional pain. This strong focus on building practical, real-world skills is also a key feature of an intensive outpatient program, where clients learn and apply these tools while still navigating their daily lives.
Motivational Interviewing to Inspire Change
While CBT and DBT provide the "how-to" of recovery, Motivational Interviewing (MI) tackles the "why." This collaborative, respectful counseling style is designed to help a person find and strengthen their own motivation to change. Instead of a therapist telling you that you must change, they act as a guide, helping you explore and resolve your own mixed feelings.
Motivational Interviewing isn't about convincing someone to change; it's about helping them find their own reasons to do so. This approach honors their autonomy and builds a powerful, internal drive for recovery that is far more sustainable than external pressure.
This compassionate, non-confrontational approach is vital in integrated dual diagnosis treatment. It helps people build the internal resolve needed to fully engage with skill-building therapies like CBT and DBT, creating a powerful synergy that drives recovery forward.
The effectiveness of combining these approaches isn't just theory—it's well-documented. Since the mid-1990s, controlled research on comprehensive dual diagnosis programs has consistently shown positive effects on substance use, psychiatric symptoms, housing stability, and overall quality of life. By using these proven therapies together, integrated care provides a structured yet flexible path to healing both conditions at once.
What to Expect on Your Treatment Journey
Stepping into an integrated dual diagnosis treatment program can feel like a big, uncertain step. Knowing what the journey actually looks like can take the edge off the anxiety and set clear, manageable expectations. This process isn't a mystery; it’s a structured, supportive path designed to address your unique needs right from day one.
The entire journey is built on one core idea: treating your mental health and substance use as interconnected parts of a whole. There are no separate paths or conflicting messages—just one unified plan and one dedicated team working with you every step of the way.
The First Step: A Comprehensive Assessment
Your journey kicks off with a comprehensive assessment. This is way more than just filling out forms; it’s a deep dive into your history, symptoms, and what you want to achieve. Clinicians will carefully look at both your mental health and substance use patterns together to create a complete picture.
This initial evaluation is critical. It helps the clinical team understand how your conditions feed each other—for example, how a depressive episode might trigger substance cravings, or how anxiety gets worse after using. This detailed understanding becomes the bedrock of your personalized treatment plan.
Creating a Single, Unified Treatment Plan
After the assessment, your multidisciplinary team gets together to create a single, unified treatment plan. This isn't two separate plans awkwardly stapled together. It’s a cohesive roadmap where the goals for your mental health and substance use are woven together.
This plan will outline the specific therapies, support services, and any medications needed to help you heal. For instance, a goal to reduce anxiety might be directly linked to a goal of preventing relapse, with specific strategies designed to tackle both at the same time.
A unified plan ensures that every member of your team—from your psychiatrist to your therapist and case manager—is working from the same playbook. This coordinated effort prevents fragmentation and provides consistent, seamless support as you move through different levels of care.
Your Multidisciplinary Support Team
You won't walk this path alone. A key piece of integrated dual diagnosis treatment is the multidisciplinary team of specialists dedicated to your recovery. This team often includes:
- Psychiatrists who manage medications for both mental health symptoms and substance cravings.
- Licensed Therapists who lead individual and group sessions using proven, evidence-based methods.
- Addiction Specialists who provide targeted support for the unique challenges of substance use.
- Case Managers who help coordinate all your care and connect you with practical resources for things like housing or employment.
This collaborative approach makes sure all aspects of your well-being are covered. The team meets regularly to discuss your progress, ensuring your treatment plan evolves as you do. For those who need it, this may include medication-assisted treatment (MAT), which can be a vital tool in recovery. You can learn more about what medication-assisted treatment is and how it fits into a comprehensive plan.
The diagram below shows how your progress is continuously monitored and used to fine-tune your care plan.
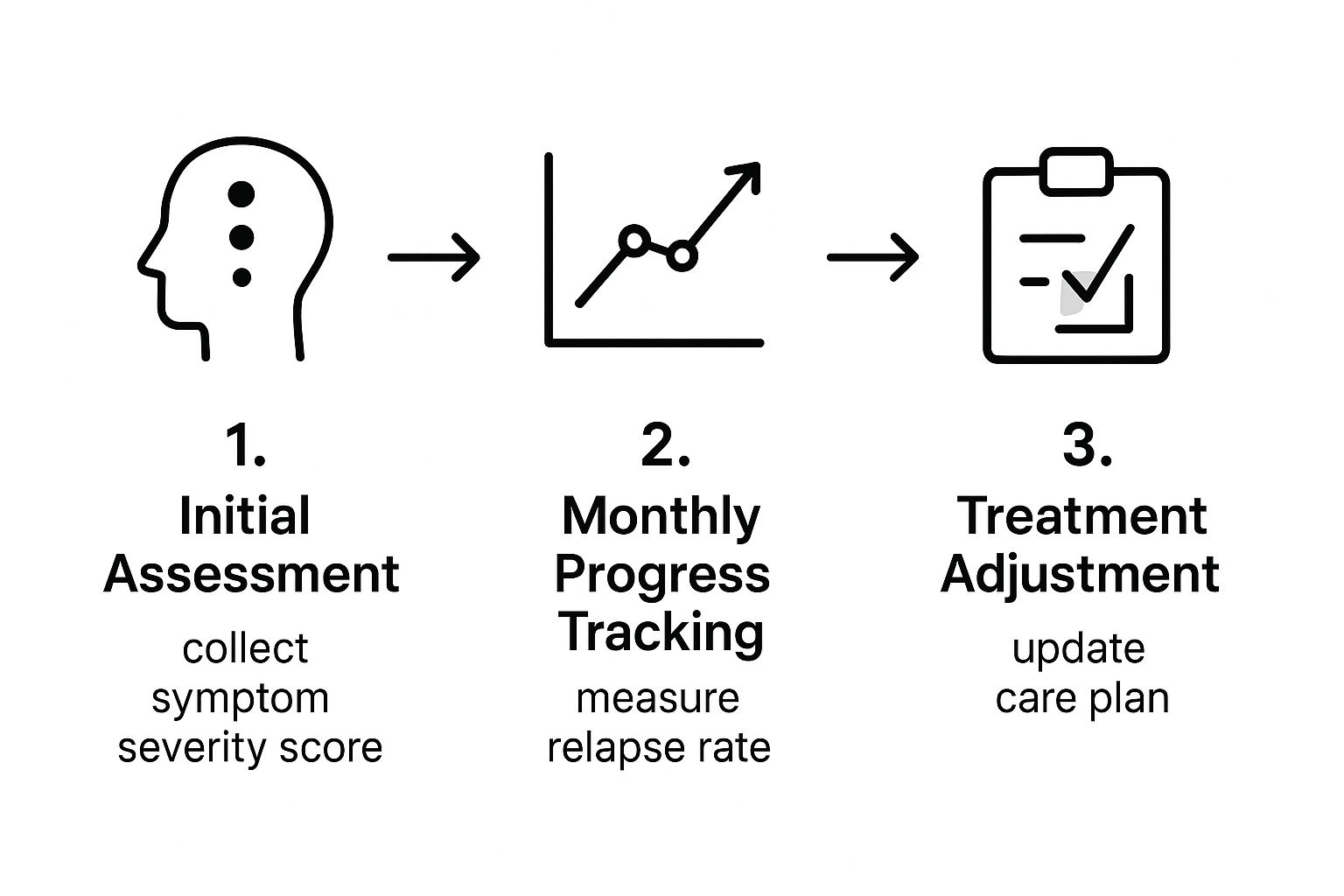
This feedback loop ensures that your treatment stays dynamic and responsive, adjusting right alongside you as your needs change.
Navigating the Barriers to Finding Integrated Care
While the benefits of integrated dual diagnosis treatment are clear, finding a high-quality program can feel like searching for a needle in a haystack. Many people run into frustrating dead ends, from outdated healthcare systems and insurance hurdles to a simple shortage of properly trained providers.
These barriers aren't just minor speed bumps; they can delay or completely block access to the life-saving care that people with co-occurring disorders desperately need. Understanding what you're up against is the first step toward breaking through those walls.
Why Quality Care Can Be So Hard to Find
Historically, mental health and addiction services grew up in completely separate silos. It was like having one mechanic for your car’s engine and another, in a different town, for its electrical system—and they never, ever spoke to each other. This split created deep divides in funding, professional training, and treatment philosophy that we're still dealing with today.
Even though the healthcare landscape is slowly shifting, the echoes of that old system persist. Many facilities still lack the resources or expertise to treat both conditions with equal skill. This forces individuals into a maddening cycle of being told they’re "not a good fit" for one program because of their other diagnosis.
The result is a huge gap in care. While there has been a 4% increase over six years in programs offering integrated services, only around 16% of substance abuse treatment centers provide the intensive mental health care essential for effective dual diagnosis treatment. This scarcity highlights just how urgent the need for truly comprehensive programs is. You can explore more statistics on dual diagnosis care from Michael's House to see the full picture.
Actionable Strategies for Your Search
Navigating this complex system requires you to become a proactive and informed advocate for yourself or your loved one. Instead of feeling powerless, you can take concrete steps to find and access the right kind of care.
It all starts with asking direct, specific questions when you're vetting any potential treatment center. Don't be afraid to dig deeper than their glossy brochures. A genuinely integrated program will have clear, confident answers.
Here are the key questions you need to ask:
- "Do you have a single, unified treatment plan for both conditions?" A "yes" signals a cohesive, effective approach. A "no" or a vague answer suggests a fragmented, less effective model.
- "Is your clinical team cross-trained in both mental health and addiction?" This confirms that the staff has the specialized expertise required to handle both sides of the coin.
- "Will the same therapist address both my anxiety and my substance use in our sessions?" The answer reveals whether they offer truly integrated therapy or just two separate services running in parallel.
Navigating insurance can be one of the biggest hurdles. Always call your provider directly and ask for a "benefits verification" specifically for "co-occurring disorder treatment" at both an intensive outpatient (IOP) and partial hospitalization (PHP) level of care. Get everything in writing, including authorization numbers.
By arming yourself with this knowledge and asking the right questions, you can cut through the confusion. This empowers you to identify genuinely effective integrated dual diagnosis treatment programs and successfully advocate for the comprehensive care you deserve.
Got Questions About Integrated Treatment? We've Got Answers
Stepping into the world of recovery can feel overwhelming, especially when you’re trying to sort out the best approach for a co-occurring disorder. Getting clear, straightforward answers is the first step toward making a confident decision. Let’s tackle some of the most common questions people have about integrated dual diagnosis treatment.
How Can I Tell If a Program Is Truly Integrated?
This is a fantastic question, and the answer is simpler than you might think. A truly integrated program has one treatment plan, one clinical team, and one primary location for both your mental health and substance use care. The magic is in the unified, simultaneous approach.
The best way to know for sure is to ask a potential provider directly: "Do you treat co-occurring disorders at the same time, with a single, cross-trained team?" If their answer involves referring you out to a separate therapist for mental health or sending you to another clinic for addiction services, that’s a red flag. That’s a parallel or sequential model, not a genuinely integrated one. You want a team where psychiatrists, addiction specialists, and therapists are all in the same building, collaborating on your care every single day.
Is Integrated Treatment More Expensive?
It's natural to worry about cost, but this is one of those cases where the upfront investment saves a fortune down the road. While a specialized integrated program might seem like a bigger initial expense, it's dramatically more cost-effective in the long run. Why? Because it actually works. By getting to the root of both conditions at the same time, it massively cuts the risk of relapse, re-hospitalization, and the painful cycle of bouncing between different programs that don't talk to each other.
Think of it like this: you can either pay for a dozen cheap, temporary patches on a leaky pipe, or you can invest once in a comprehensive repair that fixes the core problem for good. Integrated treatment is that comprehensive repair. It leads to stronger, more sustainable outcomes, which means lower overall healthcare costs over a lifetime. The good news is that many insurance plans now recognize its effectiveness and provide coverage.
How Long Does Integrated Treatment Last?
There’s no one-size-fits-all timeline for healing. The length of treatment is always shaped by your specific needs, your progress, and your personal goals. Recovery is a journey, a continuum of care, not a single event with a fixed end date.
The whole process is designed to give you the right amount of support exactly when you need it. The path often looks something like this:
- Residential or Partial Hospitalization (PHP): This is usually the starting point—a highly structured, intensive phase that might last anywhere from 30 to 90 days.
- Intensive Outpatient (IOP): As you gain stability, you might step down to an IOP. This level offers robust support but with more flexibility to start reconnecting with work, school, or family life.
- Supportive Outpatient & Aftercare: This is the long game. It involves less frequent, long-term support designed to help you maintain your hard-won stability and navigate life’s challenges without relapse.
The ultimate goal isn’t to keep you in treatment forever; it’s to build the skills and resilience you need for the long haul. As you get stronger and more independent, the level of care adjusts right along with you, ensuring you have a solid foundation for a healthy, fulfilling life.
At Altura Recovery, we know that real, lasting healing can only happen when you treat the whole person. Our team of compassionate, cross-trained clinicians is dedicated to providing true integrated care, addressing both mental health and substance use at the same time. If you’re tired of the cycle and ready to build a life in recovery, we’re here for you. Discover our approach to dual diagnosis treatment by visiting https://www.alturarecovery.com.