Struggling with substance use often feels like you're fighting on two fronts. On one hand, there's the substance itself. On the other, there’s a silent, often unseen battle with anxiety, depression, or past trauma. This powerful link is known as a dual diagnosis, where addiction and a mental health condition show up at the same time. For healing to really take hold, addiction and mental health treatment has to tackle both issues together.
Why Addiction and Mental Health Are Deeply Connected
Think of addiction like a big, unhealthy tree. The parts you can see—the trunk, the branches, the wilting leaves—are the outward signs of substance use. This is what most people, maybe even you, tend to focus on.
But beneath the surface, there's a sprawling, tangled root system. Those roots are the underlying mental health struggles—the anxiety, depression, or trauma—that anchor the addiction and keep it fed.
Simply treating the substance use is like trimming the branches. The tree might look a little better for a while, but as long as the roots are still there, the unhealthy growth is bound to come back. This is exactly why so many people relapse after only addressing their drinking or drug use. The real problem was never unearthed.
Understanding the Cycle of Self-Medication
For many, this connection starts as a way to cope. Someone wrestling with crippling social anxiety might discover that a few drinks makes it possible to get through a party. A person haunted by unresolved trauma might find that opioids can numb the emotional pain, even if just for a little while.
Over time, the brain learns to connect that substance with a feeling of relief. This kicks off a dangerous cycle: the mental health symptoms trigger the urge to use, and the substance use eventually makes the original mental health symptoms even worse. It’s a trap.
This isn't just a theory; the numbers bear it out. In the United States, about 48.5 million people aged 12 or older had a substance use disorder in the past year alone.
A dual diagnosis isn’t two separate problems happening at once. It’s one deeply interconnected struggle. Lasting recovery depends on healing both the visible symptoms and the hidden wounds that fuel them.
Common Pairings You Might Recognize
Certain mental health conditions and substance use disorders show up together so often because of how they feed off each other. Seeing these patterns can help you make sense of your own experience.
- Alcohol and Depression: People often use alcohol to lift their spirits, but since it’s a central nervous system depressant, it ultimately drags them deeper into hopelessness and sadness.
- Stimulants and Anxiety: While a stimulant might offer a temporary burst of focus or energy, the inevitable crash can send feelings of panic, paranoia, and anxiety through the roof.
- Marijuana and PTSD: Someone with trauma might use marijuana to dissociate from painful memories, but this escape prevents them from actually processing the trauma and moving forward.
Recognizing this connection is the first, most critical step toward finding an addiction and mental health treatment plan that actually works. You can learn more about how specialized programs address these overlapping issues in our guide on dual diagnosis outpatient treatment.
How Integrated Treatment Heals The Whole Person
Imagine trying to fix a car engine by only working on the transmission. No matter how much you tinker with the gears, the real problem—the misfiring cylinders—goes completely ignored. This is a perfect picture of what separate, disconnected treatment for addiction and mental health often feels like. You end up addressing one symptom while the root cause keeps running haywire.
Integrated treatment is the modern, far more effective solution. Think of it as having a single, coordinated pit crew for your well-being. Instead of sending you to one specialist for your anxiety and another for your substance use, this approach brings a dedicated team together under one roof to treat both conditions at the same time.
This model is built on a simple but powerful truth: substance use is very often a symptom of deeper emotional pain. It's a coping mechanism someone develops to manage anxiety, depression, or trauma. By addressing the root causes and the substance use simultaneously, integrated care offers a much more complete and lasting path to recovery.
The Problem With Disconnected Care
In the past, treatment was often sequential. A person would be told, "Get sober first, then we can work on your depression." This created a dangerous gap. Without the substance to numb their feelings, the underlying mental health symptoms would often come roaring back, leading directly to a relapse.
This fragmented system created a revolving door where people never truly got a handle on the interconnected nature of their struggles. It was inefficient and, for so many, deeply ineffective.
Integrated care closes this gap by acknowledging that you can't heal the mind without also healing the habits it has formed to survive. It's a commitment to treating the whole person, not just isolated symptoms.
Core Components Of Integrated Treatment
A strong integrated program weaves several key elements together to create a powerful fabric of support. This ensures every aspect of your well-being is seen and addressed.
The image below highlights some of the common hurdles people face, showing just how prevalent stigma is and how long the average delay is before someone gets the help they need.
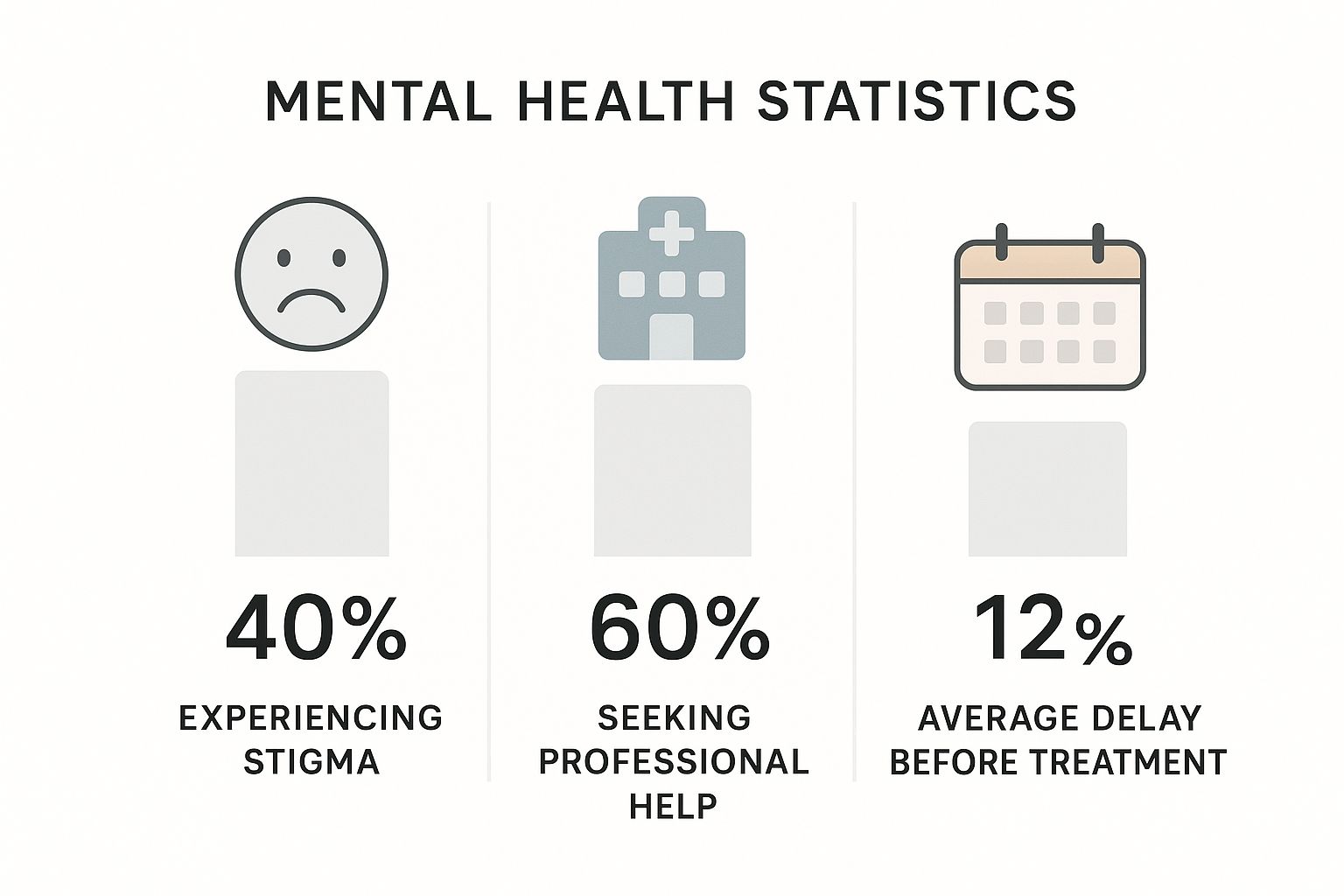
The data really drives home the gap between needing and receiving timely care, a delay often fueled by stigma and other barriers in the system.
So, how does integrated treatment bridge this gap? It's all about a coordinated approach that includes:
- Unified Treatment Planning: Your therapist, psychiatrist, and recovery coach all work from the same playbook. Your care is consistent and targeted, with no mixed signals.
- Dual Diagnosis Expertise: The clinical team is specially trained to understand the complex dance between conditions like PTSD and alcohol use, or anxiety and stimulant dependency.
- Simultaneous Therapies: You’ll engage in therapies that address both your substance use triggers and your mental health symptoms in the same sessions. A group might explore, for example, how social anxiety fuels the desire to drink.
- Medical and Psychiatric Oversight: Medication management is handled by a team that gets how psychiatric medications can affect recovery, and vice versa.
To really illustrate the difference, here's a quick comparison of the old and new models:
Comparing Treatment Models for Co-Occurring Disorders
This table breaks down the key differences between the traditional, sequential approach and modern, integrated care for individuals with a dual diagnosis. It shows why treating both issues at once is so much more effective.
| Feature | Sequential (Traditional) Treatment | Integrated (Modern) Treatment |
|---|---|---|
| Philosophy | Treats substance use and mental health as separate, unrelated issues. | Views both conditions as intertwined and addresses them simultaneously. |
| Team Structure | Two separate teams (one for addiction, one for mental health) with little communication. | A single, unified team of dual-diagnosis experts collaborating on one care plan. |
| Treatment Order | "Get sober first, then we'll address your anxiety." (Or vice-versa). | Treatment for both conditions begins at the same time and is woven together. |
| Client Experience | Often feels fragmented, confusing, and contradictory. | Feels seamless, supportive, and holistic. |
| Typical Outcome | High rates of relapse as the untreated condition undermines progress. | Higher rates of sustained recovery and improved overall well-being. |
Ultimately, the integrated model removes the guesswork and the gaps that people so often fell through in the past, offering a much more direct and stable path forward.
Integral to healing the whole person, effective treatment also emphasizes the transformative power of lifestyle changes, which are critical for overall well-being and sustained recovery. This focus on the whole person—mind, body, and daily habits—is what makes integrated care so powerful. It doesn’t just patch the wall; it fixes the leaky pipe and strengthens the foundation for good.
Evidence-Based Therapies That Build Resilience
Real addiction and mental health treatment isn't just about stopping a behavior; it’s about building an entirely new foundation for your life. This new groundwork is laid with proven, evidence-based therapies designed to give you the skills and resilience to handle life’s curveballs without turning back to old habits.
Think of these therapies less as abstract conversations and more as hands-on training for your mind. Each one offers a different set of tools to untangle the complex knots between your thoughts, feelings, and actions. The goal is to move beyond simply managing symptoms and start creating lasting, positive change from the inside out.
This approach is so critical that it's driving massive growth in the recovery field. The global drug addiction treatment market, recently valued at USD 18.91 billion, is on track to hit USD 31.20 billion by 2032. Therapy-based methods make up over half of that market, which tells you just how vital they are for successful, long-term recovery.
Cognitive Behavioral Therapy: Rebuilding Your Mental Framework
Cognitive Behavioral Therapy (CBT) is a cornerstone of dual diagnosis treatment for a reason. It’s built on a simple but powerful idea: our thoughts, feelings, and behaviors are all connected. CBT helps you spot and challenge the automatic negative thought patterns that fuel both substance cravings and mental health struggles.
Imagine your mind is running on a set of old, faulty blueprints that always lead to the same destructive outcomes. CBT is like getting a new set of architectural plans. You learn to catch flawed thinking in the act—like catastrophizing a small mistake or jumping to the worst possible conclusion—and actively replace it with more balanced, realistic perspectives.
This process gives you the power to break cycles that once felt unbreakable. For example, instead of an anxious thought immediately triggering the urge for a drink, you learn to pause, question that thought, and choose a healthier response.
Dialectical Behavior Therapy: Mastering Your Emotions
While CBT is fantastic for challenging thoughts, Dialectical Behavior Therapy (DBT) shines when it comes to managing intense emotions and improving relationships. It was first developed for borderline personality disorder, but its skills are incredibly effective for anyone who struggles with emotional dysregulation—a common thread in co-occurring disorders.
DBT hands you a practical toolkit for getting through emotional storms without resorting to self-destructive behaviors. It’s all built on four key skills:
- Mindfulness: Learning to stay in the present moment, observing your thoughts and feelings without judgment.
- Distress Tolerance: Building strategies to survive painful moments without making things worse.
- Emotion Regulation: Understanding your emotions and learning how to reduce your vulnerability to painful ones.
- Interpersonal Effectiveness: Learning to communicate your needs and set boundaries in a way that protects your self-respect and strengthens your relationships.
Mastering these skills gives you healthy alternatives when you feel overwhelmed, building your confidence to handle stress constructively. It’s also a journey that loved ones need to understand. For more on that, check out our guide on how to support someone in recovery.
Specialized Therapies For Deeper Healing
Beyond CBT and DBT, we use specialized therapies to target specific underlying issues. Trauma, in particular, is a common driver of addiction that requires a focused approach.
Eye Movement Desensitization and Reprocessing (EMDR) is a powerful therapy designed to help people process and heal from traumatic memories. Using bilateral stimulation, like guided eye movements, it helps the brain reprocess "stuck" memories, effectively reducing their emotional charge.
For someone whose substance use is a way to numb traumatic flashbacks, EMDR can be life-changing. By healing the original wound, it can remove one of the main reasons the addiction took hold in the first place.
Alongside these core therapies, many people find it helpful to explore complementary methods for managing daily stress. Learning different stress relief and relaxation techniques can be a valuable part of building a resilient, well-rounded life. By combining proven clinical therapies with supportive self-care practices, you create a powerful, personalized strategy for a healthier future.
What a Day in Outpatient Recovery Looks Like
The idea of starting recovery can feel pretty intimidating, especially when you have no idea what to expect. A lot of people picture a sterile, hospital-like place, completely cut off from real life. But that’s not what outpatient treatment is about at all. It’s designed to fit into your life, not pull you out of it, giving you a structured, supportive place to heal while you still handle your day-to-day responsibilities.
At Altura Recovery, a typical day follows a steady rhythm that blends intensive therapy, practical skill-building, and genuine connection with peers. The whole point is to create a predictable, safe routine that lets you focus completely on getting well. With both day and evening programs, this structure is built to work around your existing commitments, whether that’s a job, school, or family.
Morning Arrival and Check-In
Your day starts when you walk into our facility—a place where you’ll be greeted by staff who get it, who understand the journey you’re on. The first thing you’ll do is a brief check-in, which is a moment to ground yourself and set an intention for the day ahead. This isn’t just about marking yourself present; it's a chance to share how you're feeling, talk through any challenges from the night before, and connect with your support system before the real work begins.
That quick check-in keeps our clinical team tuned in to your immediate needs, making sure the day's sessions are as relevant and effective as they can be. It’s a small but powerful habit that builds accountability and a sense of community right from the start.
From there, you’ll move into the core therapeutic work, which might kick off with an educational group on a topic like understanding your triggers or the neuroscience behind addiction.
Mid-Day Individual and Group Sessions
The heart of the day is all about evidence-based therapy. Outpatient programs are built on a rich mix of one-on-one attention and group support, with each piece playing a crucial, complementary role.
- Individual Therapy: This is your dedicated time with a primary therapist. It’s a confidential space to explore the personal issues and underlying mental health conditions that might be driving your substance use. Here, you can work on personalized treatment goals, process trauma with methods like EMDR, or build practical coping skills using CBT.
- Group Therapy: Group is where the realization hits: you are not alone. Led by a licensed clinician, you'll join discussions with peers who understand your struggles because they’ve lived them, too. These sessions create a powerful sense of connection and give you a safe place to practice new communication skills, support others, and hear different perspectives on recovery.
At its core, outpatient care is about building a new, healthier life while still living in the real world. The blend of individual and group therapy equips you with the tools to navigate daily challenges without resorting to old patterns.
This structured yet flexible approach is key to making treatment stick. For a deeper look at different treatment settings, you might find our article exploring what exactly is rehab helpful.
Afternoon Skill-Building and Planning
As the day winds down, the focus often shifts from intensive emotional processing to practical, real-world application. This part of the schedule is dedicated to building tangible life skills that support long-term sobriety and mental wellness.
Activities during this time could include:
- Relapse Prevention Workshops: Identifying your personal triggers and creating a concrete plan to manage them when they show up.
- Mindfulness and Stress Reduction: Practicing meditation or other techniques to regulate your emotions without turning to a substance.
- Life Skills Training: Working on practical areas like setting healthy boundaries, communicating effectively, or managing your time.
You'll end with a check-out session, giving you a chance to reflect on what you learned and set a few goals for the evening. This structured departure helps you transition back home with a clear head and a sense of accomplishment. You leave not just with insights, but with an actual plan for continuing your recovery journey, one step at a time.
Finding the Right Level of Support for Your Needs
Choosing the right addiction and mental health treatment isn't about finding the single "best" program—it's about finding the one that provides the perfect amount of structure for your unique situation. Outpatient care isn’t just one thing; it's a whole spectrum of support designed to meet you exactly where you are in your recovery.
Think of it like learning to swim. Someone just starting out needs a lot of direct support in the shallow end. A more experienced swimmer, on the other hand, might only need a lifeguard keeping a watchful eye from a distance. Each level of outpatient care provides a different intensity of support, making sure you feel both safe and challenged in just the right ways.
Partial Hospitalization Programs (PHP)
The most intensive level of outpatient care is the Partial Hospitalization Program (PHP). This option offers a highly structured, immersive therapeutic environment. It often serves as a crucial step down from residential treatment or as a powerful way to prevent hospitalization in the first place.
- Time Commitment: This is the most significant time investment, typically requiring clients to attend treatment for 5-6 hours per day, 5 days a week.
- Intensity: PHP provides comprehensive clinical services that can include daily group therapy, individual counseling, psychiatric oversight, and workshops to build coping skills.
- Ideal Candidate: Someone who needs daily structure and robust support but has a stable and safe home to return to each evening.
Intensive Outpatient Programs (IOP)
The next step down is the Intensive Outpatient Program (IOP). This level offers a strong treatment schedule but with more flexibility, allowing individuals to start integrating their recovery work with daily responsibilities like work, school, or family.
An IOP strikes a crucial balance. It provides more therapeutic contact than traditional weekly therapy but allows you to actively practice your new coping skills in your real-world environment each day.
An IOP lets you build a solid foundation for lasting recovery without having to put your entire life on pause. Peer connection is a huge part of this stage, and many find that exploring resources on building supportive online communities can open up valuable new avenues for support.
- Time Commitment: An IOP usually involves 3-4 hours of treatment per day, 3-5 days a week. Many programs offer morning or evening sessions to work around job schedules.
- Intensity: The focus is heavily on group therapy, individual sessions, and relapse prevention. It's less immersive than a PHP but still provides substantial, consistent support.
- Ideal Candidate: A person who has completed a higher level of care or someone whose condition doesn't require daily medical monitoring but who needs more than just once-a-week therapy.
Standard Outpatient Programs (SOP)
Standard Outpatient Programs (SOP) represent the most flexible level of care. This is often the final phase of a structured treatment plan, designed to provide ongoing support as you gain more and more confidence in your recovery.
An SOP is all about maintaining the progress you've made while navigating the real challenges of everyday life. The schedule is minimal, but that connection to a clinical team remains a vital anchor. It’s the long-term support system that helps solidify new, healthy habits for good. To get a better sense of the full range of support available, you can explore our detailed overview of mental health and addiction services.
Why Seeking Help Is More Important Than Ever

If you’re wrestling with substance use and mental health issues, it’s easy to feel like you’re the only one going through it. The isolation can be overwhelming. But the truth is, you’re part of a massive, growing movement toward healing. Reaching out has never been more vital, and more people are doing it every single day.
This isn't a sign of failure; it’s a powerful signal of progress. It means the walls of stigma that kept people suffering in silence are finally starting to crumble.
Thanks to greater awareness and more open conversations, millions are finding the courage to acknowledge their struggles and take that first brave step. Seeing this shift validates your own decision to look for support. It’s a collective recognition that real, compassionate solutions exist and are becoming easier to find.
A Growing Network of Support
This rising demand has fueled serious growth in the addiction and mental health treatment field. The global market, recently valued at around USD 9.44 billion, is expected to hit USD 16.22 billion by 2034. That’s more than just a number—it’s a worldwide commitment to tackling substance use disorders head-on. You can dig into the specifics in this detailed report on the addiction treatment market.
This expansion means a tangible increase in resources, expertise, and new approaches designed to help people get better. It translates to more specialized programs, more trained clinicians, and a stronger, more robust support system ready to meet you where you are.
Understanding that you are not alone is a game-changer. Every person who seeks help contributes to a culture of healing, making it easier for the next person to find their way.
Your journey is part of a larger, positive trend. By seeking help, you are joining a community of people who are reclaiming their lives and rewriting their futures.
What This Means for Your Recovery
The expanding landscape of addiction and mental health treatment offers more personalized and effective options than ever before. This positive momentum ensures that when you're ready to take action, a strong and evolving support system is there to catch you.
This growth signifies:
- More Specialized Care: Programs are increasingly equipped to handle the complexities of a dual diagnosis.
- Reduced Stigma: As more people openly discuss their recovery, the shame tied to getting help diminishes for everyone.
- Improved Accessibility: With more providers and flexible options, finding the right fit for your life becomes much more manageable.
Choosing to seek help is a courageous act, not just for yourself but for the broader community. It reinforces the idea that recovery is possible and that a network of dedicated professionals and supportive peers is ready to guide you. The tools you need are out there, waiting for you to begin.
Got Questions About Treatment? We've Got Answers.
Stepping toward recovery always brings up questions. It's completely normal. Uncertainty about how treatment works, what it costs, or if it's truly private can feel like a huge barrier. We want to clear that path by giving you straight, honest answers to the questions we hear most often.
Getting clear on the facts is about more than just information—it's about feeling confident enough to make a move.
How Do I Know If I Need Integrated Treatment?
This is a big one. If you find yourself reaching for a substance mainly to quiet feelings of anxiety, numb depression, or push away memories of past trauma, then integrated treatment is almost certainly the right fit. It’s built for people whose substance use and mental health are tangled together.
Another huge tell is if you’ve tried to quit before on your own, only to have a flood of overwhelming emotions send you right back to using.
If you even suspect a link between how you feel and why you use, the best next step is a professional dual diagnosis assessment. Think of it as creating a personalized map for your recovery, making sure no part of your struggle gets left behind.
What’s the Difference Between Outpatient and Inpatient Treatment?
The simplest answer comes down to where you sleep at night. Inpatient treatment is a 24/7 residential program. You live right at the facility, which creates a highly structured, immersive environment where you can focus solely on healing.
Outpatient treatment, on the other hand, lets you live at home. You can keep up with work, school, or family life while attending scheduled therapy and support sessions at the center. It’s the perfect option for people who need intensive help but have a stable home environment and don’t require around-the-clock medical supervision.
Is My Treatment Actually Confidential?
Yes. 100%. All addiction and mental health treatment is shielded by strict federal privacy laws, especially the Health Insurance Portability and Accountability Act (HIPAA). These rules aren't just suggestions; they legally ensure your personal health information is kept completely private.
From your very first phone call to us until your last therapy session, every single detail is secure. We take this responsibility seriously because creating a safe, trusting space is essential. It allows you to focus on your recovery without ever worrying about judgment or your privacy.
How Does Involving My Family Help?
Addiction rarely affects just one person—it sends shockwaves through the entire family. That’s exactly why healing together can be so incredibly powerful. Bringing family into the process is a core part of building a support network that will actually last.
Family therapy and educational workshops do a few key things:
- Heal Broken Trust: It creates a safe, guided space to mend relationships and learn how to communicate again.
- Educate Loved Ones: It helps your family understand the science behind addiction and mental health, replacing confusion and frustration with empathy.
- Build a Real Support System: It teaches your loved ones how to offer healthy, effective support instead of accidentally enabling old patterns.
When your family is part of the solution, the foundation for your recovery becomes much stronger and more resilient for the long haul.
At Altura Recovery, we believe clear answers lead to confident action. If you have more questions or you’re ready to see what our outpatient addiction and mental health programs look like, our team is here to help. You can learn more about our personalized approach at https://www.alturarecovery.com.








