In mental health, a relapse means symptoms have returned in a significant way after a period of feeling stable and well. It’s not a sign that you’ve failed—far from it. Think of it as a common and manageable part of the long-term recovery journey for conditions like depression, anxiety, or bipolar disorder.
What a Relapse Actually Is (in Human Terms)
Let's ditch the clinical jargon for a minute and talk about what a relapse feels like. Imagine your recovery journey is like hiking a beautiful but challenging trail. You’ve been making great progress, enjoying the view, and feeling stronger with every step. Then, suddenly, you slip on a loose rock or find yourself on a path that feels uncomfortably familiar—a detour that leads back toward where you started.
That detour is a relapse. It’s a noticeable return to the disruptive thoughts, feelings, or behaviors you worked so hard to move past. This is more than just a bad day; it’s a clear signal that your brain and body need some extra support again.
Relapse Is Not Failure
This is the most important thing to remember: a relapse does not erase your progress. The strength you built and the miles you covered on your journey still count. A setback is just a sign that your current strategies need a tune-up, not that you've failed completely. Many people go through this; it’s a recognized part of recovery for both mental health and substance use disorders. You can learn more about the deep connection between addiction and mental health treatment and see how integrated care is designed to handle these exact challenges.
A relapse isn’t a sign of weakness. It’s a sign that you might need extra care for your mental health, just like your body needs special attention when you catch a cold or pull a muscle.
What It Might Look Like
Relapse shows up differently for everyone. For someone managing depression, it could mean losing interest in hobbies again after months of enjoying them. For a person with an anxiety disorder, it might be the return of frequent panic attacks after a long period of calm.
Common signs often fall into a few key areas:
- Behavioral Changes: Pulling away from friends and family or ditching helpful routines like therapy appointments or your morning walk.
- Emotional Shifts: Feeling overwhelmed by the old hopelessness, anger, or sadness that had previously lifted.
- Cognitive Patterns: The return of harmful thought loops or that critical inner voice you had learned to quiet.
Recognizing these signs is the first step to getting back on track. It’s how you turn a detour into a powerful learning opportunity for lasting wellness.
The Three Stages of a Mental Health Relapse
When we think about what relapse means in mental health, it’s easy to picture it as a single, sudden event. But that’s rarely how it works. A relapse doesn't just appear out of nowhere; it’s a process that builds over time through predictable stages.
The good news is that this progression gives you a crucial window of opportunity. By learning to recognize the signs, you can intervene long before things reach a crisis point.
The journey often begins quietly, well before any of the old, obvious symptoms reappear. Let's break down the three distinct phases.
The infographic below maps out this progression, showing how relapse starts internally and works its way outward through your emotions, thoughts, and actions.
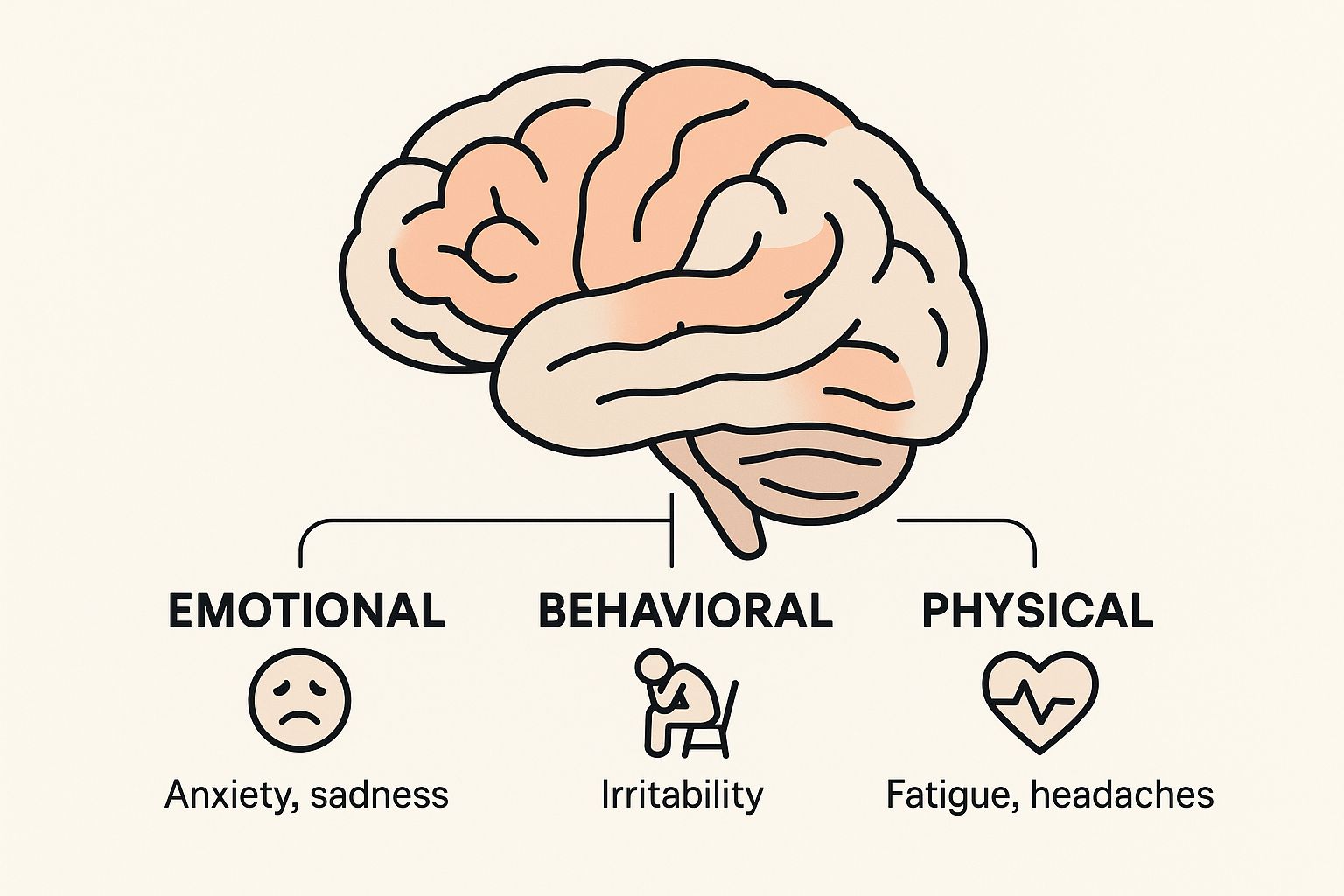
As you can see, the path usually starts with subtle emotional shifts, escalates into a mental tug-of-war, and only then results in noticeable behavioral changes.
Stage 1: Emotional Relapse
In this first stage, you aren't actively thinking about falling back into old behaviors. You may not even realize it's happening. But beneath the surface, your emotions and actions are starting to pave the way for a setback.
The warning signs are often subtle changes in routine:
- Isolating yourself: You might start pulling back from friends, skipping your support group, or avoiding family.
- Bottling up emotions: Instead of talking about what’s bothering you, you keep it all locked inside.
- Slipping self-care: You might neglect sleep, make poor food choices, or let your personal hygiene slide.
This stage is really about a quiet breakdown in self-care and coping skills. Building a stronger foundation with practical coping strategies for anxiety and depression can help you recognize and reverse this trend early.
Stage 2: Mental Relapse
If an emotional relapse goes unchecked, it often progresses to the next stage: a state of intense internal conflict. It’s like a war is being waged in your mind—part of you wants to stay on track, but another part is being pulled back toward old, unhealthy patterns.
A mental relapse is that internal debate. It's when you start bargaining with yourself, thinking, "Maybe just one missed therapy session won't hurt," or you find yourself romanticizing past negative behaviors.
This is where you might catch yourself lying, looking for excuses to skip healthy habits, or fantasizing about slipping back into old ways.
Stage 3: Physical Relapse
This is the final stage, and it’s what most people picture when they hear the word "relapse." Physical relapse is when you actively return to the behaviors and symptoms you’ve been working so hard to manage.
It's the tangible outcome of the two previous stages going unaddressed. Since studies show that up to half the world's population may experience a mental health disorder at some point, understanding this progression is vital knowledge for a massive number of people. Recognizing the emotional and mental precursors is the key to preventing this final stage from ever happening.
Understanding the Difference Between a Lapse and a Relapse
In the recovery journey, it’s easy to confuse a lapse with a relapse. People often use the terms interchangeably, but they represent two very different forks in the road. Getting them mixed up can trigger a wave of unnecessary shame and threaten to derail all your hard-earned progress.
Knowing the difference is one of the most powerful tools you can have. It helps you respond with self-compassion instead of self-criticism when you hit a bump, which is critical for building resilience.
What is a Lapse?
Think of a lapse as a brief, temporary slip. It’s a single misstep on your path, not a total departure from it. A lapse is an isolated incident.
Maybe you skipped a therapy appointment because you felt overwhelmed, or an old anxious thought pattern popped up before you re-centered yourself with a coping skill. It's a moment where your old symptoms reappear, but you quickly get back on track. A lapse doesn't erase your progress.
What is a Relapse?
A relapse, on the other hand, is a more significant and sustained return to unmanageable symptoms. It’s not just one misstep but a full-blown return to old, harmful patterns of thinking and behaving that takes you completely off your recovery path.
Where a lapse is momentary, a relapse is a prolonged state. It's when you stop using your coping skills altogether and slide back into the state you were in before you started getting help.
Reframing the Slip
The real difference between a lapse and a relapse often comes down to your response. When you treat a lapse as a learning opportunity—a chance to figure out what triggered it and adjust your recovery plan—it actually makes you stronger. It’s a signal to fine-tune your strategy, not abandon it.
A lapse is like stumbling on a hiking trail. You might skin your knee, but you get up, dust yourself off, and keep moving forward. A relapse is choosing to turn around and walk all the way back to the start.
Seeing a slip through this lens empowers you to handle minor setbacks with grace and get right back to the work of healing.
To make it even clearer, let's break down the key distinctions between a lapse and a relapse side-by-side.
Lapse vs Relapse Key Distinctions
This table helps illustrate the practical differences between a brief slip and a more serious return to old patterns.
| Characteristic | Lapse (A Slip) | Relapse (A Return) |
|---|---|---|
| Duration | Short-lived; a single event or a very brief period (hours or a day). | Sustained; a prolonged return to old behaviors and symptoms (days, weeks, or longer). |
| Control | You typically regain control quickly and get back to your recovery plan. | Involves a significant loss of control over a longer period. |
| Impact | A minor setback that doesn't undo overall progress. | A major setback that significantly disrupts recovery and daily functioning. |
| Mindset | Often seen as a mistake to learn from; a "wake-up call." | Can feel like a total failure or a full return to a previous state of illness. |
Understanding these differences helps you assess a situation accurately. Recognizing a slip as a lapse allows you to correct your course quickly, without the guilt that can turn a small stumble into a major fall.
Identifying Common Relapse Warning Signs and Triggers
Recognizing the early signs of a potential relapse is one of the most powerful skills you can build on your mental wellness journey. Think of these warning signs like yellow traffic lights—they don’t mean you have to stop, but they’re a clear signal to slow down, pay attention, and proceed with extreme caution.
These signs are usually subtle shifts in your thoughts and routines. They’re the small changes that sneak in long before a major return of symptoms. When you learn to spot your personal red flags, you can act proactively and turn what could have been a setback into a real opportunity for growth.
Triggers: The External and Internal Cues
A trigger is anything—a person, place, feeling, or event—that bumps up your risk of relapse. These are highly personal, but they generally fall into two buckets:
- External Triggers: These are things happening in your environment. It could be a high-stress project at work, a heated argument with a loved one, or even just driving past a place tied to past trauma.
- Internal Triggers: These come from within you. We’re talking about intense emotions like loneliness or anger, physical states like pure exhaustion, or old, harmful thought patterns making a comeback.
Common Warning Signs to Watch For
While everyone’s red flags are unique, there are definitely some common warning signs that show up across different mental health conditions. Learning to tune into these patterns is absolutely key.
You might notice changes in your daily life, like letting your self-care slide or starting to isolate yourself from friends and family. This kind of withdrawal is often one of the very first signs that you’re struggling. It feels hard, but connecting with others during these times is crucial. Engaging in structured activities like exploring different group topics for addiction recovery can provide that essential connection when you feel most vulnerable.
A relapse rarely begins with one big, bad decision. It starts with the small compromises—skipping a therapy session, forgetting your medication, or telling yourself, "I'll deal with it tomorrow." Recognizing these minor slips is the key to preventing a major slide.
The risk of symptoms returning is a serious part of managing any long-term condition. Relapse in bipolar disorder, for example, is a significant concern. A UK study found that over five years, about 7.2% of participants relapsed, and of those people, 60.9% only had one episode. But other research shows relapse rates as high as 54.3% over just two years, which really underscores how vital it is to spot those early warning signs. You can dig into the specifics of these findings on relapse rates in bipolar disorder to get a clearer picture of the data.
How to Build a Proactive Relapse Prevention Plan

Understanding what relapse means is one thing; actively working to prevent it is another game entirely. This is where a Relapse Prevention Plan (RPP) comes in. It's your personal roadmap for navigating the inevitable challenges of recovery. This isn't just a document—it's a proactive strategy that puts you back in the driver's seat when you feel most vulnerable.
Think of an RPP as a fire escape plan for your mind. You hope you never need it, but you map it out in advance so that if a fire starts, you know exactly which exits to take without a second thought. This plan is a living, breathing guide, something best developed with a therapist or a trusted loved one to build a strong safety net.
Core Components of Your Plan
A solid RPP is built on two things: honest self-awareness and practical tools. It has to be tailored specifically to your experiences, acknowledging your unique patterns and needs. A great way to build a proactive relapse prevention plan is by incorporating various therapeutic activities to boost well-being that strengthen your mental resilience.
Your plan should absolutely include these essential elements:
- Your Personal Triggers and Warning Signs: Get brutally honest. Make a detailed list of the specific situations, feelings, or thoughts that have historically sent you backward.
- Healthy Coping Strategies: What will you actually do when a trigger appears? List concrete actions—call a specific friend, go for a walk around the block, use a 5-minute breathing technique.
- A Support Network Contact List: This is your emergency call sheet. Compile the names and numbers of people you can call in a crisis—your therapist, family members, a sponsor, or friends who truly get it.
This structured approach isn't just a nice idea; it's backed by extensive research. Psychological interventions are proven to significantly reduce the risk of relapse. One major analysis found these plans lowered the hazard ratio to 0.60, which means they substantially delay the time to relapse compared to standard treatment.
A Relapse Prevention Plan turns vague intentions into concrete actions. It transforms "I should probably call someone" into "When I feel X, I will call Y and Z."
Making the Plan Actionable
The best plan in the world is useless if you don't use it. Keep it accessible. That could mean a dedicated notebook, a note pinned on your phone, or a document shared with your support system.
A robust RPP becomes even more critical when conditions overlap, like in co-occurring disorders. In fact, an integrated dual diagnosis treatment approach almost always incorporates this type of planning to tackle both mental health and substance use challenges at the same time.
Finally, review and update your plan regularly. As you grow in your recovery, your triggers will shift and your coping skills will get stronger. Your RPP should evolve right along with you, remaining a relevant and powerful tool for maintaining your long-term stability.
Your Top Questions About Mental Health Relapse, Answered
When you're on a recovery journey, it's completely normal for questions and fears about setbacks to pop up. The idea of relapse can be intimidating, but getting clear, straightforward answers helps strip away the anxiety and empowers you to move forward with confidence.
Let’s tackle some of the most common questions head-on.
Does a Relapse Mean My Treatment Failed?
Absolutely not. A relapse isn't a sign that your treatment failed, and it's definitely not a reflection of your worth or effort. It’s better to think of it as a signal—a check-engine light for your recovery plan.
Recovery is almost never a straight line from point A to point B. A relapse simply means it's time to reassess what’s working and what isn’t. It’s an opportunity to learn more about your triggers, fine-tune your coping strategies, and work with your support team to make adjustments. It highlights areas for growth; it doesn't erase all the hard-won progress you’ve already made.
How Can I Support a Loved One Experiencing a Relapse?
Supporting someone you care about through a relapse is a delicate dance between empathy and healthy boundaries. The best first step is to approach them calmly, without judgment, and simply express your concern. Offering a listening ear can make a world of difference.
Gently encourage them to reconnect with their therapist, psychiatrist, or support group. You can also offer practical help, like a ride to an appointment or help with an errand that feels overwhelming.
Remember, you can be a vital part of their support system, but you can’t be their therapist. It's crucial that you also protect your own well-being during this time. Don't be afraid to lean on your own support network.
Is It Possible to Prevent Relapse Completely?
While guaranteeing you'll never have another setback isn't realistic, you can absolutely reduce the likelihood and severity of a relapse. Being proactive is your best defense. This is where your Relapse Prevention Plan becomes your most powerful tool.
Consistently using the strategies you've learned builds incredible resilience. This isn't about perfection; it's about practice. It means actively engaging in key habits like:
- Managing stress effectively: Using healthy coping skills before stress hits a boiling point.
- Practicing consistent self-care: Making sleep, good nutrition, and restorative activities non-negotiable.
- Staying connected: Leaning on your support system regularly, not just when you're in crisis.
- Recognizing early warning signs: Paying close attention to those subtle shifts in your mood, thoughts, and behaviors.
These actions give you the best shot at maintaining long-term stability and wellness.
How Long Does a Mental Health Relapse Usually Last?
There’s no set timeline for a relapse. The duration is different for everyone and depends on the specific condition, individual circumstances, and—most importantly—how quickly support is put in place. The single most critical factor in shortening a relapse is early intervention.
The moment you recognize those warning signs and reach for your support plan, you're already shortening the timeline. Acting swiftly can turn what might have become a prolonged, difficult episode into a brief, manageable setback.
At Altura Recovery, we understand that real healing involves navigating setbacks with compassionate, expert guidance. If you or a loved one needs support, our outpatient programs are designed to help you build the skills for long-term recovery while maintaining your daily life. Learn more about our approach at https://www.alturarecovery.com.








