When you peel back the layers of addiction, you find two core components driving the cycle: physical dependence and psychological dependence. Think of them as two sides of the same coin—one rooted in the body, the other in the mind. They often feel tangled together, but understanding how they differ is the first step toward addressing both effectively.
Understanding the Core Differences in Dependence

Addiction is a complex beast, affecting both our physical wiring and our mental state. While physical and psychological dependence are distinct, they’re almost always intertwined, creating a tough cycle for anyone struggling with substance use.
Let’s use a simple, everyday example: coffee. That throbbing headache and wave of fatigue you feel after skipping your morning cup? That's physical dependence in action. Your body has literally adapted to the daily dose of caffeine and is protesting its absence with tangible, uncomfortable symptoms.
Now, think about the ritual itself—the smell of the beans, the warmth of the mug, the belief that you simply can't start your day without it. That’s psychological dependence. It's the emotional connection and the ingrained mental habit, not just a physical need.
A Clear Comparison
The distinction sharpens when you look at the mechanisms behind each one. Physical dependence is all about the body's physiological adaptation to a substance, which becomes obvious when withdrawal symptoms kick in after you stop. Psychological dependence, on the other hand, is an emotional and mental preoccupation with the substance.
This isn't a niche problem; substance use disorders impact millions across the globe. Back in 2008, estimates suggested that somewhere between 155–250 million people aged 15–64 had used illicit substances. You can discover more insights about the global impact of substance use on PMC.
Here’s a simple breakdown of how they differ:
| Aspect | Physical Dependence | Psychological Dependence |
|---|---|---|
| Origin | The body's physiological adaptation | The mind's emotional and cognitive reliance |
| Primary Driver | Avoiding physical withdrawal symptoms | Seeking pleasure or escaping emotional pain |
| Key Symptoms | Nausea, sweating, tremors, aches | Intense cravings, anxiety, irritability, restlessness |
| Common Example | The flu-like sickness of heroin withdrawal | The deeply ingrained ritual of a cigarette break |
At its core, physical dependence is about the body needing a substance to function normally, while psychological dependence is about the mind believing it cannot cope without it. Both are powerful forces in addiction.
Navigating this dual challenge is central to any successful recovery journey. Just going through detox to handle the physical side is rarely enough, because the psychological pull is often what triggers a relapse down the road. This is why effective treatment must tackle both components head-on—a foundational principle in understanding what is rehab and how it paves a real path to lasting sobriety.
How Physical Dependence Hijacks the Body
Physical dependence is what happens when your body’s internal chemistry literally changes to accommodate the regular presence of a substance. This isn’t about weak willpower or a moral lapse; it’s a biological adaptation. In an effort to keep things stable, your brain and body recalibrate their normal operations around the drug.
Think of it like a thermostat. Your body is great at regulating its own functions. But if you constantly have an external heater—the substance—running, the body’s internal furnace dials way down, expecting that outside source to do the work. The moment you unplug that heater, the internal system is caught completely off guard, triggering a state of chaos and distress.
This biological adjustment is what leads directly to tolerance and withdrawal. These are the twin pillars of physical dependence, the clearest signals that the body has been rewired.
The Science of Tolerance
Tolerance is usually the first sign that your body is adapting. It’s when you find yourself needing more of a substance to get the same effects you once felt with a much smaller amount. The dose that used to bring relief or euphoria barely registers anymore, because your body has gotten better at breaking it down or your brain’s receptors have become less sensitive.
For example, someone might start with a single painkiller to manage discomfort. A few months later, that one pill barely takes the edge off, and they need two or three just to feel the same relief. This isn't a sign of weakness; it's a physiological response showing that the body has built up a defense against the drug's effects.
This constant need to up the dose is a dangerous part of the addiction cycle. As tolerance builds, the risk of overdose skyrockets because a person has to consume progressively higher—and more toxic—amounts to chase that original feeling.
The Reality of Withdrawal
Withdrawal is the body's powerful, and often agonizing, reaction when a substance is cut back or stopped. Because the body has learned to function with the drug, its sudden absence throws everything into disarray. The symptoms that follow are the body’s desperate attempt to regain balance, and they can range from merely uncomfortable to life-threatening.
The specific symptoms of withdrawal vary dramatically depending on the substance, creating very different physical experiences for each.
- Alcohol Withdrawal: This can be one of the most dangerous. Symptoms often start with tremors (the "shakes"), anxiety, and heavy sweating. In severe cases, it can progress to seizures or a condition called delirium tremens (DTs), which can be fatal without medical supervision.
- Opioid Withdrawal: Often described as the worst flu imaginable, opioid withdrawal is intensely miserable. It typically involves deep muscle and bone aches, diarrhea, vomiting, chills, and uncontrollable sweating. While it's rarely deadly, the sheer physical discomfort is a major driver of relapse.
- Stimulant Withdrawal: When someone stops using stimulants like cocaine or methamphetamine, the withdrawal is famous for its "crash." This includes profound fatigue, a ravenous appetite, and severe depression, which brings a significant risk of self-harm.
It's crucial to understand that physical dependence can develop even when someone is taking a prescribed medication exactly as their doctor directed. It is a natural biological process, not an immediate sign of abuse, but it highlights the powerful way these substances can hijack the body's normal functions.
This is a critical distinction in the physical vs psychological dependence discussion. The physical symptoms of withdrawal are temporary, but they are often so brutal that the fear of experiencing them becomes a primary reason to keep using. This physical trap powerfully reinforces the psychological craving, creating an interconnected cycle that’s incredibly hard to break without professional help. That’s why addressing the body’s needs through a safe, medically supervised detox is the essential first step before the deeper psychological work of recovery can even begin.
The Mind's Compulsion: Unpacking Psychological Dependence
If physical dependence chains the body, then psychological dependence hijacks the mind. It’s that relentless mental and emotional compulsion to use a substance, driven not by the need to dodge physical sickness but by a deep-seated, perceived need to feel good, manage stress, or just get through the day.
This is the part of addiction people often just call "the habit." It's the powerful, ingrained belief that you simply cannot function, relax, or have fun without your substance of choice. This mental territory is where intense cravings and obsessive thoughts about using take root, creating a powerful loop that's incredibly hard to break.
The Mental And Emotional Drivers
At its core, psychological dependence is about learned associations. It systematically rewires the brain's reward system, forging a strong link between a substance and feelings of pleasure or relief from pain. Over time, these connections become so strong they feel like reflexes.
For example, someone might develop a psychological dependence on marijuana not because their body will revolt without it, but because they’ve come to believe they can’t be creative, unwind after work, or fall asleep without getting high. The drug becomes a crutch they use to regulate their emotional state.
Other common behavioral links include:
- Situational Triggers: The overwhelming urge to light a cigarette that hits the second you pour a cup of coffee.
- Emotional Triggers: Automatically reaching for a drink after a stressful argument to numb difficult feelings.
- Social Triggers: The genuine belief that you can't socialize or enjoy yourself at a party without using a specific substance.
These aren't physical necessities. They are learned behaviors and mental shortcuts that can become just as powerful as any physical withdrawal symptom.
The core of psychological dependence is the powerful, often paralyzing, belief that life is unmanageable without the substance. It turns the drug into a solution for every problem, creating an emotional and mental prison.
It's important to see how all the pieces fit together. Addiction as a broader concept includes physical dependence, psychological dependence, and tolerance, with each element shaping the experience differently. Research shows that addiction impacts over 15% of the adult American population, and alcohol dependence alone accounts for roughly two-thirds of all cases. You can dig into the full research on addiction's components from the National Library of Medicine.
Behavioral Addictions: The Clearest Example
The most compelling proof of psychological dependence can be found in behavioral addictions. Things like gambling, shopping, or compulsive internet use involve no physically addictive substance, yet they can be just as destructive as any drug addiction.
A person with a gambling addiction doesn't experience physical withdrawal. Instead, when they try to stop, they feel intense restlessness, irritability, and anxiety—all hallmarks of psychological dependence. Their mind becomes consumed with thoughts of the next bet, driven by the desire to either recreate a thrill or chase their losses.
This shows that the mental compulsion alone is strong enough to completely hijack a person's life, even without a chemical hook. It is this psychological force that often proves to be the most stubborn challenge in long-term recovery.
Treating this side of addiction requires much more than just stopping the substance; it means unlearning these deeply ingrained behaviors and thought patterns. Therapies like Cognitive Behavioral Therapy (CBT) are designed specifically to identify these triggers and build new, healthier coping mechanisms. Comparing different therapeutic approaches, such as in our guide on individual therapy vs group therapy, can help you find the best path forward for rewiring these mental habits and finally achieving freedom from the psychological grip of addiction.
Comparing Symptoms of Physical and Psychological Dependence
While physical and psychological dependence often feel tangled together, their symptoms show up in starkly different ways. Getting clear on the differences is crucial for creating a recovery plan that actually works—one that addresses both the body and the mind. Think of it this way: one is a visceral, bodily rebellion; the other is a persistent, mental obsession.
This chart breaks down the key risks, showing how withdrawal, intense cravings, and relapse rates differ between the two.
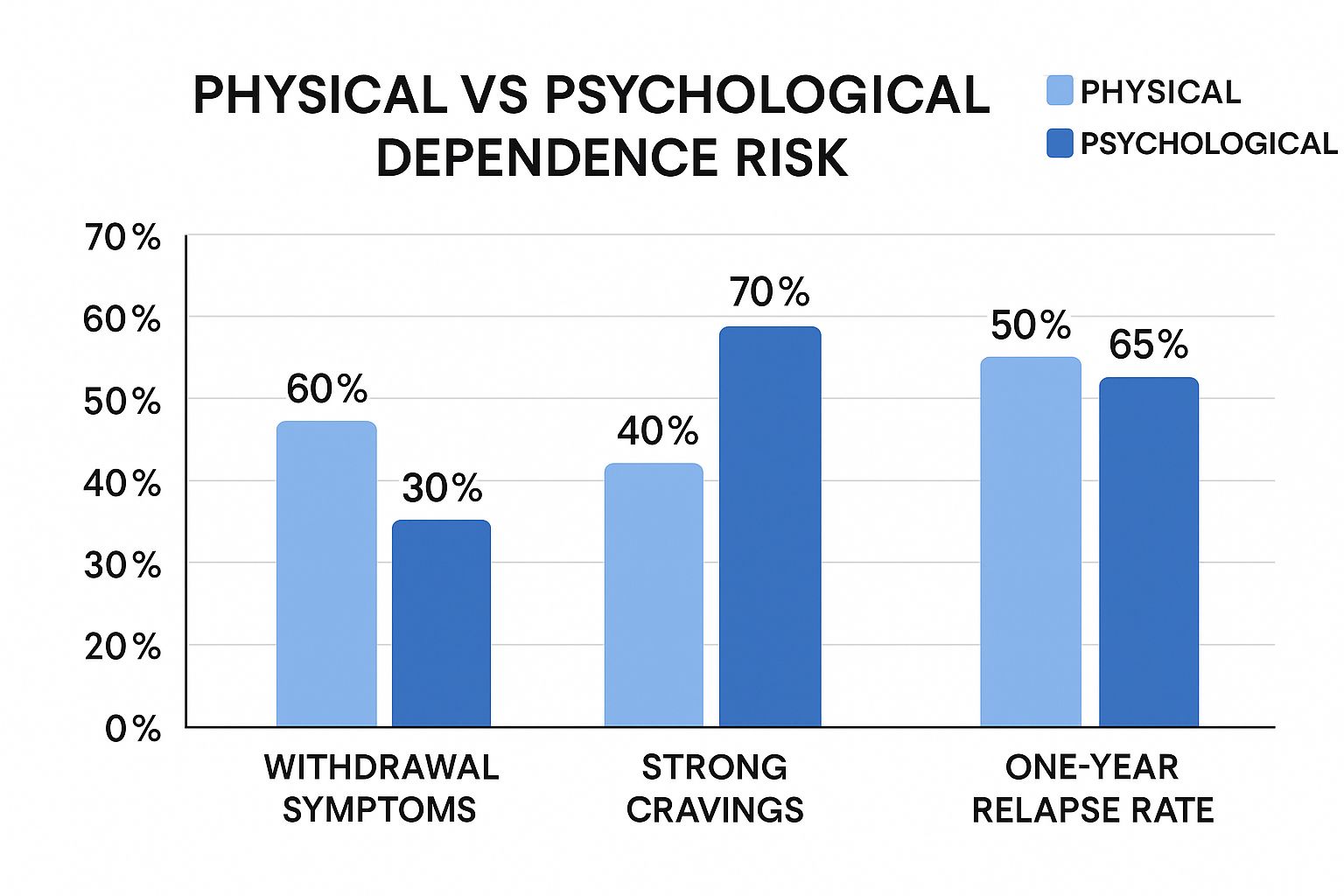
The data tells a clear story. Physical dependence brings a higher rate of acute withdrawal, but psychological dependence is what really fuels the stronger cravings and the alarmingly high one-year relapse rate.
Withdrawal: The Body Versus the Mind
The sharpest contrast between physical and psychological dependence surfaces during withdrawal. The symptoms don't just feel different; they come from entirely separate systems of distress.
Physical withdrawal is the body’s raw, physiological protest when a substance it has adapted to is suddenly gone. These symptoms are tangible, measurable, and often brutal. Someone withdrawing from alcohol might experience uncontrollable tremors, drenching sweats, and a racing heart. Opioid withdrawal is notorious for its intense flu-like misery: deep muscle aches, nausea, and unrelenting chills. These aren't just feelings; they're biological crises.
On the other hand, psychological withdrawal is a storm raging inside the mind. It shows up as overwhelming anxiety, crushing depression, irritability, and a profound inability to feel any pleasure at all. Someone with a psychological dependence on cannabis might not be physically shaking, but they can feel an unbearable restlessness and an obsessive conviction that they cannot handle life’s challenges without it.
Physical withdrawal symptoms are the body screaming for a substance to restore its chemical balance. Psychological withdrawal symptoms are the mind desperately clinging to a learned coping mechanism it believes is essential for survival.
The Nature of Cravings
Cravings are a universal feature of addiction, but where they come from and how they feel can vary dramatically. Understanding the physical vs psychological dependence dynamic helps explain why.
Physical cravings are often directly wired to the agony of withdrawal. The urge to use is a primal, desperate push to stop the physical pain. It’s the body’s attempt to end the sickness, and it peaks during the acute detox phase.
In contrast, psychological cravings can linger for months or even years after the last physical symptom has faded. These cravings are sparked by emotional states and environmental cues. For example:
- Situational Triggers: Driving past a familiar bar can trigger a sudden, intense urge for a drink.
- Emotional Triggers: Feeling overwhelmed after a tough day at work can create a powerful craving for the substance once used to unwind.
- Social Triggers: Being at a party where others are using can ignite the powerful feeling that you need the substance to fit in or have fun.
Impact on Daily Life and Behavior
Both types of dependence throw daily life into chaos, but in different ways. Physical dependence tends to create an immediate, crisis-driven disruption. A person might miss work because they are too sick from withdrawal or spend all their energy just trying to find more of the substance to keep the sickness at bay.
Psychological dependence creates a more subtle but equally destructive disruption. It quietly rewires a person's priorities, thoughts, and routines. Hobbies get dropped, relationships are neglected, and responsibilities are ignored—not because of physical illness, but because every ounce of mental energy is hijacked by the obsession with the substance.
Physical vs Psychological Dependence At a Glance
The table below offers a straightforward, side-by-side comparison of these two forces, highlighting their core differences in a way that's easy to grasp.
| Characteristic | Physical Dependence | Psychological Dependence |
|---|---|---|
| Primary Driver | Driven by the need to avoid the pain of physical withdrawal. | Driven by the desire to seek pleasure, relieve emotional distress, or cope with life. |
| Symptom Type | Tangible, bodily symptoms like tremors, nausea, and sweating. | Mental and emotional symptoms like anxiety, intense cravings, and depression. |
| Duration | Acute symptoms typically last for days to a few weeks. | Can persist for months or even years, demanding long-term management strategies. |
| Treatment Focus | Medically supervised detox to manage physical symptoms safely and comfortably. | Therapy (like CBT and DBT), support groups, and the development of healthy coping skills. |
Getting through the intense symptoms of physical withdrawal is often the critical first step. Many people find that this stage is made much more manageable with the right medical support. If you want to dive deeper, our guide on what is medication-assisted treatment explains how this approach can stabilize the body. But it's crucial to remember that true, lasting recovery is only possible when the powerful psychological drivers of addiction are addressed with the same level of focus and care.
The Interplay Between Body and Mind in Addiction
It’s tempting to draw a hard line between physical and psychological dependence, treating them as two different problems. But in reality, they’re deeply connected, fueling each other in a relentless cycle that makes addiction so tough to beat.
Neither one exists in a vacuum. Think of them as two forces constantly interacting, where a struggle with one almost always cranks up the volume on the other.
This dynamic creates a vicious feedback loop. The intense physical agony of opioid withdrawal—the muscle aches, nausea, and tremors—is a purely biological event. Yet, the desperation and sheer panic triggered by those symptoms are psychological, creating an overwhelming mental craving for the drug just to make the pain stop.
The connection works the other way, too. Someone who has been physically sober for months can get sideswiped by a powerful psychological trigger. Seeing an old friend they used to use with or driving past a familiar corner can ignite a mental craving so intense it feels physical. That craving can manifest as a knot in the stomach or a racing heart, creating a perceived physical need for the substance where none existed just moments before.
The Impact of Co-Occurring Disorders
This link between body and mind gets even stronger when mental health conditions are in the mix. These situations, known as co-occurring disorders or a dual diagnosis, are incredibly common and create a much more complex challenge for recovery.
Often, issues like depression, anxiety, or PTSD predate any substance use, creating fertile ground for psychological dependence to take root.
Someone wrestling with untreated depression might turn to alcohol to numb their emotional pain, quickly developing a psychological reliance on it as a coping tool. Over time, that consistent use leads to physical dependence. Now, when they try to quit, they're not just facing the brutal physical withdrawal from alcohol. They’re also hit with the return of their original, untreated depression, which often feels even more intense than before.
This cycle can make recovery feel impossible without integrated treatment. The psychological pain drives the substance use, and the substance use makes the psychological pain worse.
The relationship between a substance use disorder and a mental health condition isn't just an overlap; it’s a powerful, self-reinforcing cycle. One condition actively feeds the other, which is why treating both at the same time isn’t just a good idea—it’s essential for lasting recovery.
Why Treating Both Is Non-Negotiable
The data on this connection is crystal clear. In the United States, the link between physical and psychological dependence is starkly evident in the mental health burden tied to substance use. About 32.8% of adults over 18 have either a substance use disorder or a mental illness.
What’s more, adolescents who experience major depressive episodes are twice as likely to use illicit drugs, a direct reflection of psychological dependence driving physical risk. You can dig deeper into these overlapping challenges in a detailed report from the Commonwealth Fund.
This powerful connection explains why a one-dimensional treatment approach is pretty much doomed to fail. A program that only focuses on medical detox might get someone through the physical withdrawal symptoms, but it leaves them completely defenseless against the psychological triggers that will inevitably pop up again.
On the flip side, therapy alone might not be enough for someone whose physical dependence is so severe that they can’t even think clearly enough to engage in counseling.
True, sustainable recovery demands a unified approach. It has to address the body’s needs with medical support while healing the mind with proven therapeutic strategies. By treating both physical and psychological dependence with equal importance, we break the cycle and build a solid foundation for real, lasting freedom.
Effective Treatment for Both Physical and Psychological Needs

To overcome addiction for good, you need a plan that tackles both the body’s cravings and the mind’s compulsions. If you only treat one side of the physical vs psychological dependence coin, you're leaving the door wide open for relapse. A modern, integrated care plan weaves together medical support with proven therapies, creating a much stronger foundation for recovery.
For anyone facing severe physical dependence, the process almost always starts with medically supervised detoxification. This isn't just about comfort; it's about safety. It allows the body to stabilize and manage the acute, often agonizing, withdrawal symptoms under the watchful eye of medical professionals. Once the physical crisis has passed, the real psychological work can begin.
Medical Support for Physical Dependence
When it comes to substances like opioids and alcohol that create an intense physical grip, medical interventions are game-changers. These treatments are designed to ease physical suffering and quiet the relentless cravings, making the early days of recovery far more manageable.
Key medical treatments include:
- Medication-Assisted Treatment (MAT): This isn't just swapping one drug for another. MAT is an evidence-based approach that uses specific, FDA-approved medications to normalize brain chemistry, block the euphoric effects of substances, and dial down physiological cravings. It is a proven tool for slashing relapse rates for opioid and alcohol use disorders.
- Medical Supervision: For substances with dangerous withdrawal symptoms, like alcohol or benzodiazepines, 24/7 medical monitoring is non-negotiable. It’s what prevents potentially life-threatening complications like seizures.
An effective treatment plan recognizes that healing the body is the essential first step. It's nearly impossible for someone to engage meaningfully with the psychological side of recovery when they're still fighting a physical war.
Once the body is on stable ground, the focus has to shift to healing the mind. This is where outpatient therapies become essential for building long-term resilience and shutting down relapse pathways.
Therapeutic Strategies for Psychological Dependence
Psychological dependence is all about learned behaviors, emotional triggers, and deeply grooved thought patterns. Effective treatment involves rewiring these mental habits and building a toolbox of healthier coping skills. An outpatient setting is perfect for this, as it allows people to practice these new skills in their actual, real-world environment.
Proven therapeutic approaches include:
- Cognitive Behavioral Therapy (CBT): This is a practical, hands-on therapy that helps you identify the destructive thought patterns that lead to using. More importantly, it teaches you how to replace them with more constructive ones, giving you real tools to manage cravings and navigate high-risk situations.
- Support Groups: Programs like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) provide an incredible sense of community and peer support. Sharing your story with people who truly get it dissolves feelings of isolation and helps build a new, sober identity.
An integrated approach is especially critical for anyone dealing with co-occurring mental health conditions. Understanding how to manage both is key to lasting wellness. You can learn more in our guide to integrated dual diagnosis treatment. By combining medical care for the body with therapeutic support for the mind, a truly personalized recovery plan provides the tools needed for sustainable freedom.
Getting Clear on Common Questions About Dependence
When you're trying to understand the difference between physical and psychological dependence, a lot of questions come up. Getting straight answers is the first step toward figuring out the right path for yourself or someone you care about.
Can You Have Psychological Dependence Without Physical Dependence?
Yes, absolutely. This is actually quite common, especially with substances that don't trigger severe physical withdrawal symptoms, like cannabis or hallucinogens. Someone might not get physically sick when they stop, but they'll still fight intense cravings, anxiety, and a powerful mental pull to use again.
Behavioral addictions are perfect examples of this. Things like gambling or internet addiction are driven entirely by psychological dependence, with no physical component at all. The entire battle is rooted in mental and emotional compulsion.
Is One Type of Dependence More Serious Than the Other?
It's a common question, but neither one is inherently "more serious"—both are critical parts of what makes addiction so complex. The immediate danger of physical dependence can be incredibly high. Withdrawal from alcohol or benzodiazepines, for instance, can be fatal without medical supervision, making it a life-threatening emergency.
However, it's the psychological dependence that often keeps people trapped in a cycle of relapse for the long haul. It can be just as difficult to overcome, if not more so. Real, lasting recovery means giving both aspects equal attention and care.
The greatest danger of physical dependence is the acute withdrawal phase. The greatest danger of psychological dependence is its persistence, which fuels relapse long after the body has healed.
How Long Does Each Type of Dependence Last?
The timelines are completely different. Physical dependence usually clears up once the withdrawal process is over. This can take anywhere from a few days to several weeks, depending on the substance. After that, the body's chemistry starts to rebalance, and the acute physical symptoms fade.
Psychological dependence, on the other hand, can stick around for months or even years. The cravings, emotional triggers, and ingrained habits require ongoing work to manage. It's a long-term process of relearning how to navigate life—its stresses and its joys—without turning back to the substance. This is where therapy, solid support systems, and healthy coping skills become non-negotiable.
At Altura Recovery, we know that true healing has to address both the body and the mind. Our outpatient programs in Houston are designed to provide the integrated care needed to break the cycle of addiction and build a real foundation for freedom. You can explore our approach at https://www.alturarecovery.com.