An Intensive Outpatient Program (IOP) offers a powerful middle ground in mental health and substance use treatment. It provides far more structure and support than traditional weekly therapy but gives you the freedom to live at home, go to work, and stay connected to your family. Think of it as a way to get immersive, high-level care without having to press pause on your entire life.
It’s designed for those moments when once-a-week appointments just aren’t cutting it, but 24/7 residential care feels like too much of a leap.
A Bridge Between Inpatient Care and Weekly Therapy

Imagine the different levels of care as a spectrum. On one end, you have 24/7 inpatient or residential treatment, where you’re fully immersed in a therapeutic environment. On the other, you have standard outpatient therapy—maybe one hour a week to check in. An IOP is the sturdy, well-supported bridge that connects the two.
This model allows you to build a foundation for lasting recovery while still navigating the real world. Instead of being removed from your daily triggers and responsibilities, an IOP helps you learn to manage them head-on with a powerful new set of skills and a team of people in your corner.
For a quick overview of what makes an IOP tick, take a look at the key features below.
IOP Therapy at a Glance Key Features
| Feature | Description |
|---|---|
| Time Commitment | Typically 9-15 hours per week, spread across 3-5 days. |
| Living Situation | Clients live at home or in a sober living environment. |
| Treatment Modalities | Combines group therapy, individual counseling, and family sessions. |
| Core Focus | Skill-building, relapse prevention, and emotional regulation. |
| Ideal Candidate | Medically stable but needs more support than weekly therapy. |
| Flexibility | Programs often offer day or evening sessions to fit work/school schedules. |
This structure is what makes IOPs so effective—they deliver a high dose of therapy while keeping you grounded in your daily life.
The Balance of Structure and Freedom
The whole idea behind what is IOP therapy is finding that sweet spot between therapeutic intensity and personal autonomy. You get a serious level of clinical care without the round-the-clock restrictions of a residential facility. This approach works because it’s built on a few core principles:
- Real-World Application: You don't just learn coping skills in a vacuum. You practice them at home, at work, and with your family the very same day, getting immediate feedback on what works.
- Community Connection: Healing happens in community. In an IOP, you’re surrounded by peers who get what you’re going through, which instantly cuts through the feelings of isolation that often come with mental health or substance use struggles.
- Maintaining Responsibilities: With schedules often available in the mornings or evenings, you don’t have to choose between getting help and keeping your job or caring for your kids. Recovery becomes part of your life, not a replacement for it.
An IOP is designed for individuals who need a robust support system but have a stable and safe home environment. It's an empowering step down from residential care or a vital step up for those who find weekly therapy isn't enough to manage their symptoms.
Proven Effectiveness in Treatment
While the flexible model feels modern, IOPs have a long and successful track record. They really gained traction between the mid-1990s and early 2010s as a cost-effective and powerful alternative to inpatient care.
Don’t just take our word for it—the research is solid. One major review of studies found that for many people with substance use disorders, IOPs deliver outcomes that are just as good as inpatient treatment. If you want to dive into the data yourself, you can read the full research on their outcomes. This makes IOP a trusted and evidence-based option for building a sustainable path forward.
How a Typical IOP Week Is Structured
If you're wondering how an Intensive Outpatient Program fits into an already busy life, you’re asking the right question. Think of an IOP less like a full-time job and more like a deeply focused part-time course in well-being. It’s structured, consistent, and designed to build real-world recovery skills without demanding you press pause on everything else.
The magic of an IOP is in its balance of intensity and real-life application. You get a substantial amount of therapeutic contact each week—far more than standard therapy—which is what drives meaningful progress. But you still go home every night, ready to practice what you’ve learned.
This setup creates a predictable and grounding routine. By showing up for a few hours a day, a few days a week, you build a steady rhythm that anchors your recovery in the middle of your everyday life.
A Look at the Weekly Time Commitment
The defining feature of an IOP is its time requirement. This isn't just about logging hours; it's about creating an immersive therapeutic environment that you can still integrate with work, school, or family responsibilities.
Most IOPs require between 9 and 20 hours of treatment per week, typically spread over three to five days. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), the standard for adults is a minimum of 9 hours of scheduled therapeutic services.
This isn't just passive listening. Those hours are packed with a mix of counseling, skill-building workshops, and support designed to give you the tools to manage your condition effectively.
The Building Blocks of Your IOP Schedule
So, what exactly fills those 9 to 20 hours? An IOP week is a carefully layered mix of different therapeutic activities, with each one playing a specific role in your recovery. While every program has its own flavor, you can expect to see a few core components on your schedule.
A typical week will almost always include:
- Group Therapy Sessions: This is the heart of most IOPs. You’ll spend several hours per session in a small, therapist-led group of peers who get what you’re going through.
- Individual Counseling: Your one-on-one sessions are a private space to dig into personal challenges, process what comes up in group, and fine-tune your treatment goals with your primary therapist.
- Educational Workshops: Think of these as practical classes for your recovery. You’ll learn tangible skills covering topics like relapse prevention, stress management, healthy communication, and the science behind addiction or mental health.
- Family Therapy (When appropriate): Many programs offer sessions with loved ones to help repair relationships, improve communication, and build a stronger support system right where you live.
The combination of group and individual therapy is a game-changer. Groups remind you that you aren’t alone and give you a safe place to practice new skills. Individual sessions let you go deeper into your personal story and goals.
This multi-faceted structure ensures you’re supported from every angle. Group sessions build community and shared experience, while individual therapy provides personalized guidance. You can learn more about how these two formats work together by reading our comparison of individual therapy vs group therapy.
The Core Therapies Inside an IOP
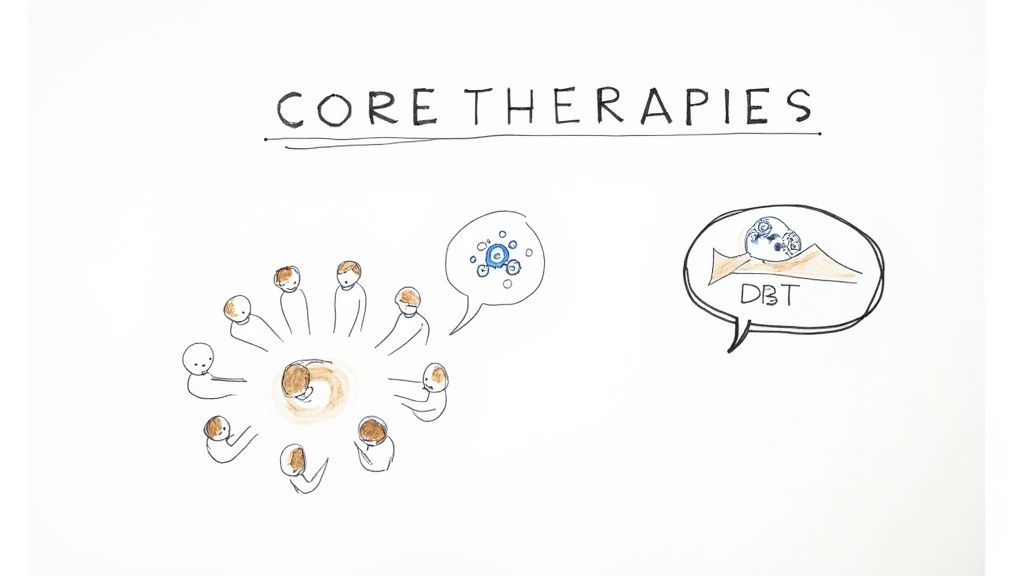
An Intensive Outpatient Program is much more than just a schedule of appointments. It's a thoughtfully designed therapeutic environment built around proven, evidence-based methods. The aim isn't just to talk about your challenges but to actively build the skills you need to manage them for the long haul. This is done through a powerful one-two punch of group sessions and personalized, one-on-one counseling.
At the heart of almost every IOP is group therapy. Think of it as a real-time laboratory for your recovery. In these sessions, you aren’t just learning from a therapist; you're connecting with peers who get what you’re going through on a deeply personal level. This shared experience is incredibly effective at breaking down the walls of isolation that so often come with mental health and substance use struggles.
Guided by a professional, you get a safe, structured space to practice new communication skills, give and receive honest feedback, and feel the power of mutual support. It’s where the concepts you learn about become real-world skills you can actually use.
Personalized Strategies in Individual Therapy
While group sessions foster a sense of community, individual therapy gives you the focused, personal attention needed to unpack your unique history and specific hurdles. This is your dedicated time to work one-on-one with a licensed clinician, digging into the issues that matter most to your recovery.
These sessions are anything but generic. You might spend the time processing past trauma, mapping out a concrete relapse prevention plan, or working through co-occurring conditions like anxiety or depression. This personalized approach ensures your treatment plan is a strategy built just for you, not a one-size-fits-all solution.
The real magic of an IOP is how group and individual therapy work together. Group therapy reminds you that you're not alone, while individual therapy ensures your personal journey is honored and expertly guided.
The Power of CBT and DBT
Two of the most common and effective therapeutic models you’ll find in an IOP are Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT). These aren't just clinical acronyms; they are practical, hands-on approaches for changing your life from the inside out.
- Cognitive Behavioral Therapy (CBT) helps you learn to spot and challenge the negative thought patterns that drive self-destructive actions. It’s like becoming a detective of your own mind, learning to catch unhelpful thoughts before they can spiral out of control. To see how this works in practice, you can learn more about the fundamentals of what Cognitive Behavioral Therapy is and its applications.
- Dialectical Behavior Therapy (DBT) is especially powerful for managing intense emotions and improving relationships. It teaches crucial skills in four key areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
These therapies don’t just offer insight—they give you tangible tools to handle triggers, regulate your emotions, and build a more resilient mindset. They form the bedrock of a lasting recovery.
Is IOP the Right Level of Care for You?
Choosing the right level of care can feel like a high-stakes decision, but it really comes down to finding the sweet spot between intensive support and real-world independence. An Intensive Outpatient Program (IOP) isn't the answer for everyone, but for the right person, it’s the perfect blend of structure and freedom.
IOPs are designed for people who are medically stable and don’t need 24/7 supervision, yet require something much more substantial than a single weekly therapy appointment. Think of it this way: if weekly therapy is a check-in, an IOP is a focused, part-time course on rebuilding your life. It’s a major step up in clinical horsepower, giving you the momentum needed to make real, lasting changes.
Who Is an Ideal Candidate for an IOP?
An IOP is often a perfect fit for a few key situations. Seeing if your circumstances line up with these can bring a lot of clarity.
A strong candidate for an IOP is someone who:
- Is Transitioning from a Higher Level of Care: If you’ve just completed an inpatient or residential program, an IOP is a vital step-down. It helps you take the skills you learned in a highly controlled setting and apply them to the chaos of daily life—but with a strong safety net still firmly in place.
- Has a Stable and Supportive Home Environment: Because you live at home during an IOP, having a safe and encouraging place to return to each day is non-negotiable. Your living situation should be a source of strength, not a trigger for relapse.
- Needs to Maintain Daily Responsibilities: If you're a student, a working professional, or a parent, you can't just press pause on your life. An IOP’s flexible scheduling, often with day or evening options, allows you to get the intensive treatment you need without having to step away from your commitments completely.
- Is Experiencing Worsening Symptoms: For someone whose mental health or substance use has started to spiral but doesn't yet require hospitalization, an IOP provides a powerful intervention to get things back on track before they reach a crisis point.
An IOP is fundamentally about empowerment. It’s for those who are ready to do the hard work of recovery while staying connected to their lives, families, and communities.
Sometimes, an IOP will also incorporate medication management into the treatment plan. If you're weighing your options, it can be helpful to learn more about what medication-assisted treatment is and see how it complements therapy.
Ultimately, the best way to know for sure is through a professional clinical assessment. That’s how we can determine if an IOP provides the right structure and support for your long-term success.
Comparing IOP to Other Treatment Options
Trying to understand the landscape of addiction and mental health treatment can feel like learning a new language, with acronyms like IOP, PHP, and outpatient creating a lot of confusion. The key is to see these not as competing choices, but as different points along a continuum of care, each designed for a specific level of need.
An Intensive Outpatient Program (IOP) carves out a vital space on this spectrum. Think of it like physical therapy after a major surgery. You no longer need to be in the hospital 24/7 (that’s inpatient care), but a single weekly visit (standard outpatient) isn’t nearly enough to rebuild your strength. An IOP is the middle ground—it’s like attending therapy several times a week to intensively practice the skills you need for a strong, lasting recovery.
Where IOP Fits in the Spectrum of Care
To truly grasp what an IOP is, it helps to see it lined up next to other common levels of care. It provides a significant step-up in support from traditional therapy without requiring the full-time commitment of living at a facility.
Here's a quick rundown of the main levels:
Residential/Inpatient Treatment: This is the most intensive option, offering 24/7 medical supervision and a highly structured environment. It’s the right choice for people who are medically unstable or need to get out of a triggering home situation to build a foundation for sobriety.
Partial Hospitalization Program (PHP): A step down from inpatient, a PHP involves treatment for 5-8 hours a day, five days a week. Clients still live at home but spend their days at the treatment center, like a full-time job focused on recovery.
Intensive Outpatient Program (IOP): This is the crucial middle ground we're focused on. IOPs provide more structure than weekly therapy but offer the flexibility to maintain work, school, and family responsibilities.
Standard Outpatient Therapy: This is the least intensive option, usually involving just one or two therapy sessions per week. It’s best for individuals who already have strong coping skills and a solid support system but need ongoing guidance to maintain their progress.
This infographic helps visualize who is best suited for the IOP level of support.
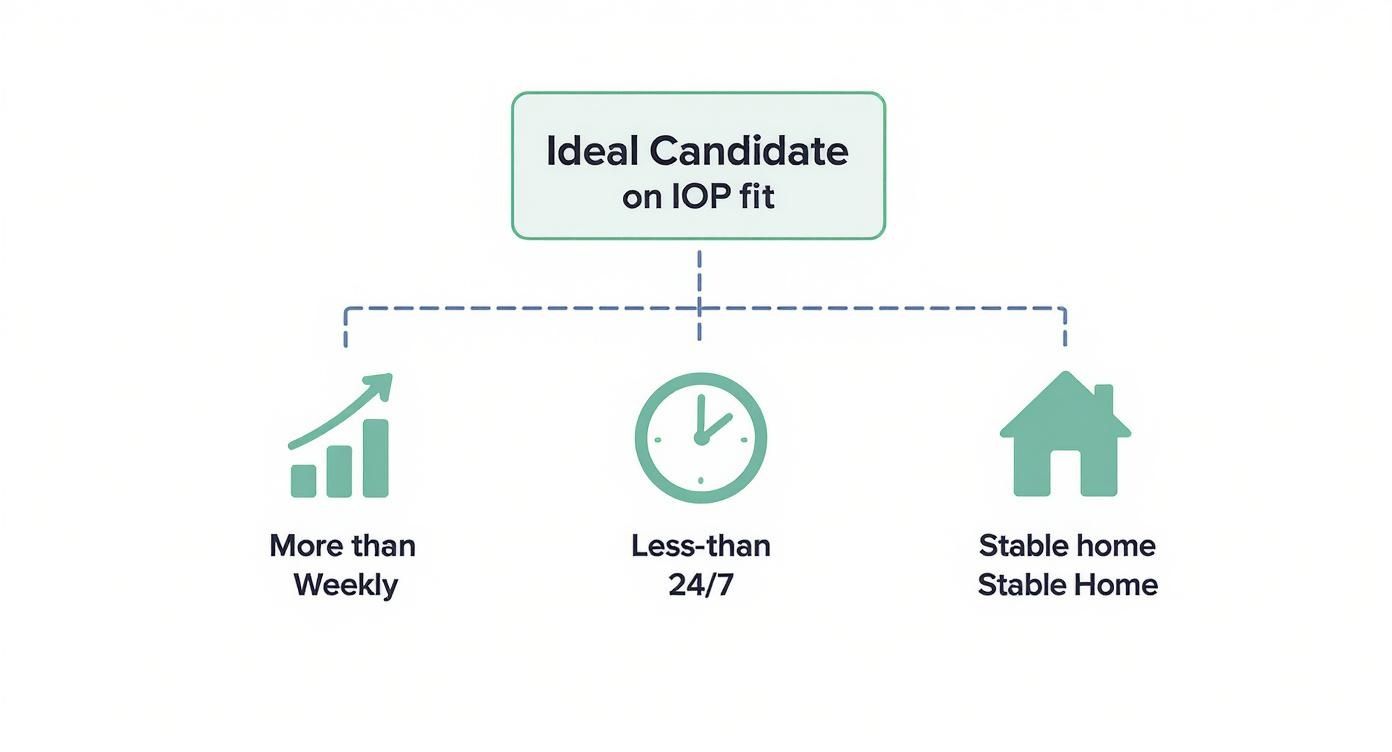
As you can see, the ideal IOP candidate is someone who needs more than weekly therapy but less than round-the-clock care, all while having a stable home to return to each day.
To make the differences even clearer, here’s a simple table comparing the main outpatient options.
IOP vs Other Treatment Levels
| Level of Care | Weekly Hours | Living Arrangement | Best For |
|---|---|---|---|
| PHP | 20-30 hours | Live at home or sober living | Stepping down from inpatient; needing daily structure |
| IOP | 9-15 hours | Live at home or sober living | Balancing recovery with work/school; needing robust support |
| Standard Outpatient | 1-3 hours | Live at home | Maintaining long-term recovery; stable with strong coping skills |
This table shows how IOP perfectly bridges the gap, offering substantial support without completely disrupting daily life.
Time Commitment and Intensity
The primary difference between these levels really comes down to the number of hours dedicated to treatment each week. An IOP typically requires about 9 to 15 hours per week, usually spread across three or four days, for a period of about 90 days.
This structure provides a strong safety net as you start navigating daily life and its inevitable triggers. If you want a more detailed look at the entire recovery journey, you can explore our guide on how does rehab work.
An IOP is the bridge that connects the highly structured world of inpatient care with the independence of traditional outpatient therapy. It allows you to test your recovery skills in the real world while still having a team of professionals to guide you.
The Real-World Benefits of Choosing an IOP
Deciding on an Intensive Outpatient Program isn't just a clinical choice; it comes with practical advantages that can make all the difference in building a lasting recovery. One of the biggest is the ability to put what you learn into practice immediately. There’s no waiting period.
You can show up for a session, learn a new way to handle a tough conversation, and use that skill with your family that very same night. This instant feedback loop is incredibly powerful. It takes coping strategies out of the realm of theory and plants them firmly in your real, lived experience, building genuine confidence in your ability to navigate life's curveballs.
A huge part of IOP is stocking your toolbox with healthy coping mechanisms for stress, which are the bedrock of long-term well-being. This focus on practical, day-to-day skill-building is what makes the model work.
Fostering Community and Connection
Another massive benefit is the built-in support network you gain. The group therapy sessions that form the core of an IOP create a powerful sense of community, pushing back against the deep isolation that so often comes with mental health and substance use struggles.
In an IOP, you’re suddenly surrounded by people who just get it. This shared experience validates your feelings, chips away at shame, and gives you a safe space to be vulnerable while trying out new ways of connecting with others.
This bond with your peers offers a unique blend of encouragement and accountability that’s tough to replicate anywhere else.
Cost-Effective and Less Disruptive
Finally, an IOP manages to deliver intensive, high-quality treatment in a way that’s both more affordable and far less disruptive than residential care. Because you live at home and commute to treatment, the costs are significantly lower, and you can keep up with your responsibilities at work and with your family.
Here’s a quick look at the financial and lifestyle advantages:
- Lower Costs: IOPs are a fraction of the cost of inpatient programs, which opens the door to top-tier care for more people.
- Maintained Responsibilities: The flexible schedules are designed to fit around your life, allowing you to keep your job, stay in school, and be there for your family.
- Real-World Integration: Instead of hitting pause on your life, treatment becomes a part of it. This promotes a much smoother, more natural transition into long-term recovery.
This structure provides a powerful, evidence-based path to healing that respects and works with your daily life, making it a truly sustainable choice.
Got Questions About IOP? We’ve Got Answers.
When you’re thinking about starting treatment, the practical details matter. How long will it take? Can I afford it? What happens when I’m done? Getting straight answers to these questions helps reduce anxiety and lets you focus on what’s important: getting better.
Here’s a clear rundown of the most common questions we hear about Intensive Outpatient Programs.
How Long Does an IOP Program Typically Last?
There's no magic number for recovery, so the length of an IOP is always based on your personal progress and clinical needs. That said, a typical timeframe for many intensive outpatient programs is around 12 weeks, or about 90 days.
During these three months, your clinical team is constantly checking in on your progress. This ensures you have enough time to really build a solid foundation of coping skills and emotional resilience before you transition to a less intensive level of support.
Will My Insurance Cover IOP Therapy?
Yes, in most cases. The vast majority of major health insurance plans cover IOP services as a standard level of care for mental health and substance use treatment. As of January 1, 2024, Medicare also began covering IOP, which has opened the door for many more people to get help.
Because IOP is a well-established, evidence-based treatment, it is almost always covered under behavioral health benefits. The best first step is to call your insurance provider directly or let the treatment center verify your benefits. This will give you a clear picture of your specific coverage, including any co-pays or pre-authorization you might need.
What Happens After I Finish an IOP?
Completing an IOP is a huge milestone, but it’s a stepping stone, not the final destination. A quality program will never just send you on your way without a map for what comes next. Before you graduate, you’ll work side-by-side with your therapist to create a detailed and personalized aftercare plan.
Think of this plan as your roadmap for maintaining momentum. It often includes things like:
- Stepping down to a lower level of care, like a supportive outpatient program (SOP) or weekly individual therapy sessions.
- Getting connected with community support groups like AA, NA, or SMART Recovery to keep that sense of peer connection strong.
- Continuing with medication management if that’s been part of your treatment.
The whole point is to make sure you have a continuous network of support to help you thrive long after you’ve left the program.
At Altura Recovery, we believe clear answers build confidence. Our team is here to help you navigate insurance, understand our programs, and create a solid plan for long-term healing. Learn more about our approach at https://www.alturarecovery.com.