Distress tolerance is the skill of getting through a painful moment without making it worse. It’s not about ignoring or eliminating tough emotions, but about learning how to sit with them—to ride the wave of an intense feeling until it passes on its own.
Think of it as your emotional anchor in a storm. It keeps you grounded when everything inside you wants to either fight, flee, or shut down.
Understanding Distress Tolerance: Your Anchor in Emotional Storms
Imagine you’re stuck in a massive traffic jam and already late for something important. Your heart pounds, frustration boils over, and you get a white-knuckle urge to lay on the horn, swerve between lanes, or just scream.
Distress tolerance is what allows you to feel all of that, take a deep breath, and accept the reality of the situation without acting on those impulses. It’s the critical space between feeling an intense emotion and reacting to it.
This skill is a cornerstone of Dialectical Behavior Therapy (DBT), a powerful treatment approach developed back in the late 1980s. Research has shown that DBT can reduce hospitalizations by roughly 73% and significantly cut treatment dropout rates for people struggling with intense emotional dysregulation. In the world of addiction recovery, for instance, patients with low distress tolerance are 2-3 times more likely to leave treatment before they’re ready. You can explore the history of DBT and its effectiveness to see just how impactful this approach is.
Reacting Versus Responding
A huge part of building distress tolerance is learning the difference between reacting and responding to a situation. They might sound similar, but they lead to vastly different outcomes.
- Reacting is impulsive and immediate. It’s driven by the rawest, most intense part of an emotion and often ends in regret. Think yelling, quitting, or using a substance to escape.
- Responding is thoughtful and intentional. It involves noticing the emotion, pausing, and then choosing a course of action that aligns with your long-term goals and values.
Developing this skill is about shifting from automatic, often destructive, reactions to mindful, constructive responses. It’s about accepting reality for what it is in the moment—not necessarily liking it, but acknowledging it so you can make a wise choice about what to do next.
Distress tolerance isn’t about being emotionless; it’s about preventing your emotions from hijacking your behavior. It’s the ability to sit with discomfort and still make choices that serve you.
To make this clearer, let’s look at how these two approaches show up in real life.
High vs Low Distress Tolerance At a Glance
The table below breaks down the typical thoughts, feelings, and actions associated with both low and high distress tolerance. It’s a quick way to see the difference between a reactive mindset and a responsive one.
| Characteristic | Low Distress Tolerance (Reactive) | High Distress Tolerance (Responsive) |
|---|---|---|
| Initial Thought | "I can't handle this!" "This feeling has to stop now." | "This is painful, but it's temporary." "What can I do to get through this?" |
| Emotional State | Overwhelmed, panicked, frantic, desperate, out of control. | Grounded, calm, observant, accepting, in control of actions. |
| Urge | To escape, numb out, lash out, or do anything to make the feeling go away immediately. | To use a coping skill, self-soothe, or wait for the emotional wave to pass. |
| Typical Action | Impulsive substance use, angry outbursts, self-harm, quitting, avoiding responsibilities. | Deep breathing, taking a walk, using distraction techniques, reaching out for support. |
| Outcome | The original problem gets worse, relationships are damaged, shame and guilt increase. | The crisis is survived without new problems, self-trust grows, resilience is built. |
Seeing the patterns side-by-side highlights how building this skill isn't just about feeling better in the moment—it's about protecting your future self from the fallout of impulsive decisions.
Why Distress Tolerance Is a Non-Negotiable Skill
Distress tolerance isn't just another psychology buzzword; it’s a bedrock skill for anyone serious about long-term mental health and sobriety. Think of it as your emotional immune system. Without it, even a small flare-up of pain can feel like a full-blown emergency, pushing you toward quick fixes that only dig a deeper hole.
This is the heart of what distress tolerance is—learning to sit with discomfort without making things worse.
When your distress tolerance is low, a familiar, damaging cycle kicks in. You get hit with a wave of intense emotion—shame, rage, bone-deep anxiety—and your first instinct is to hit the eject button. That desperation often fuels unhealthy escapes, like turning to a substance, lashing out at a loved one, or just shutting down completely.
Sure, those actions might offer a few minutes of relief, but they come with a heavy price. Every time you outsource your emotional management to a drink, a drug, or a distraction, you weaken your own ability to cope. Your emotional muscles get weaker, making the next wave of distress feel even more overwhelming. Before you know it, the "solution" has become the real problem.
From Everyday Annoyances to Full-Blown Crises
This cycle isn’t reserved for major tragedies; it plays out in the small moments of daily life. A tense text from your partner, an unexpected critique from your boss, or even a quiet evening feeling lonely can trigger this downward spiral if your tolerance is low.
What one person brushes off as a minor annoyance can feel like a five-alarm fire to another. The urge to escape the feeling—any bad feeling—becomes so intense it short-circuits rational thought. This is exactly why distress tolerance is a non-negotiable skill in addiction recovery. It builds a crucial firewall between a trigger and a relapse.
For people managing co-occurring disorders, like anxiety or depression alongside a substance use disorder, distress tolerance is the bridge connecting both sides of their recovery. It gives them a way to handle the symptoms of one condition without setting off the other.
With this skill, you can sit with the discomfort of a craving or the ache of a painful memory and know that, while it’s not pleasant, it is survivable. It breaks that automatic, deeply grooved connection between, "I feel bad," and, "I need to use."
Building a Foundation for Real Freedom
Ultimately, developing distress tolerance is about taking your power back. It’s making the choice to stop running from discomfort and start learning how to move through it.
By building this skill, you're not just learning to get through a crisis. You’re laying the foundation for a life where you are in control of your actions, not your emotions. It’s an essential piece of the puzzle for anyone chasing genuine, lasting freedom.
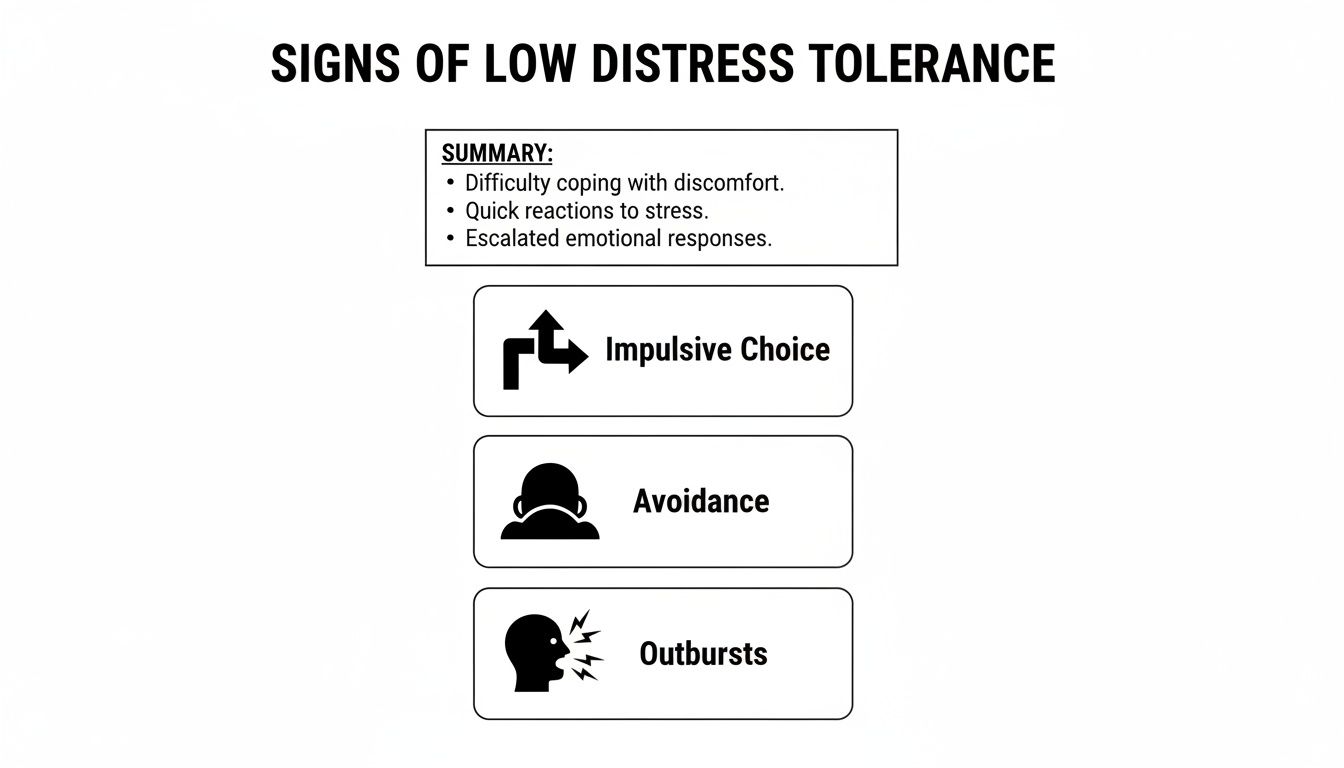
Common Signs of Low Distress Tolerance
Recognizing the signs of low distress tolerance is the first step toward building real emotional resilience. This isn't about slapping on a label. It's about spotting specific patterns that might be keeping you stuck. These signs usually show up as impulsive actions, chronic avoidance, or emotional reactions that feel way out of proportion to the trigger.
When sitting with discomfort feels impossible, life can turn into a series of emergencies you’re constantly trying to put out. This isn't a character flaw; it’s a sign that your coping skills are maxed out. Research shows that distress tolerance levels often get set in childhood and stay fairly stable into the teen years. That stability explains why adults in recovery need to intentionally build new skills—without them, the old cycle just keeps running. In fact, low distress tolerance in youth is a major red flag, often linked to future substance use and mental health struggles like anxiety. It can effectively double the risk for early-onset addiction. You can read the full research on developmental patterns of distress tolerance to see just how deep these roots go.
Behavioral and Emotional Indicators
Low distress tolerance can show up in a few key ways. Spotting them in your own life is the beginning of creating change.
Impulsive Decisions to Escape Pain: This is the big one. It looks like making a snap decision—quitting a job after one bad day, ending a relationship in the middle of a fight, or blowing your budget on something you don't need—all to get instant relief from a painful feeling.
Chronic Procrastination and Avoidance: If you find yourself constantly putting off tasks that feel hard or dodging difficult conversations, it might be a sign of low distress tolerance. The thought of the discomfort is so overwhelming that avoidance becomes your go-to move.
Emotional Outbursts: When a small frustration triggers a massive reaction, like explosive anger or uncontrollable tears, it points to a struggle with managing emotional waves. The feeling isn’t just there; it’s a total takeover.
The core issue isn't the presence of pain, but the belief that you cannot survive it. Low distress tolerance creates a frantic urgency to make the feeling stop, no matter the long-term cost of your actions.
Unhealthy Coping Habits
Beyond those knee-jerk reactions, low distress tolerance often pushes people to rely on external "fixes" to numb what's going on inside.
These habits offer a temporary escape hatch but ultimately keep you from developing healthier, more lasting ways to cope. They might look like:
- Relying on substances to deal with stress, anxiety, or sadness.
- Compulsive behaviors like excessive shopping, gambling, or binge-eating.
- Constant distraction through social media, TV, or overworking to avoid being alone with your thoughts.
- Catastrophizing minor setbacks, turning a small mistake into a sign of complete and utter failure.
It’s crucial to notice these behaviors without judgment. They aren't failures; they are simply signals that it’s time to start building a new toolkit for navigating life’s storms.
Four Powerful DBT Skills to Build Distress Tolerance
Knowing you need to build distress tolerance is one thing; having a practical, in-the-moment toolkit is something else entirely. For that, we turn to Dialectical Behavior Therapy (DBT), which offers a powerhouse of evidence-based skills designed for exactly these moments.
Think of them as your emotional first-aid kit. They aren’t meant to magically erase the pain. Instead, they’re designed to help you survive a crisis without doing something that makes the situation worse. By using them, you create a critical pause between an intense feeling and a knee-jerk reaction, giving your wiser, calmer mind a chance to catch up.
The skills below are built to counteract the exact signs of low distress tolerance shown here—like impulsive choices and emotional outbursts.
As you can see, low distress tolerance often shows up as a desperate scramble to escape discomfort, leading to choices that derail your long-term goals. DBT skills give you a better way forward.
TIPP Skills for When You’re in Crisis Mode
When your nervous system is screaming and you feel like you’re about to fly out of your skin, you can’t think your way calm. You have to do something. The TIPP skills are all about changing your body chemistry, fast, to dial down the emotional intensity.
- Temperature: Splash your face with cold water or hold an ice pack against your cheeks and forehead. This triggers the mammalian "dive reflex," a physiological response that instantly slows your heart rate.
- Intense Exercise: Go all out for just a minute or two. Think jumping jacks, sprinting in place, or burpees. It burns off that raw, anxious energy and gives your nervous system a much-needed reset.
- Paced Breathing: Deliberately slow your breathing way, way down. Inhale for a count of four, then exhale slowly for a count of six. This activates the parasympathetic nervous system—your body’s natural relaxation response.
- Paired Muscle Relaxation: Tense a group of muscles as you breathe in, then let them go completely limp as you breathe out. Work your way through your whole body, from your toes to your face, releasing physical tension as you go.
These are your go-to physical interventions for moments when you feel completely overwhelmed and on the verge of an impulsive, destructive act.
ACCEPTS Skills for When You Need a Healthy Escape
Sometimes, the best thing you can do is get your mind off the problem for a while so it doesn't consume you. The ACCEPTS acronym is your menu of seven healthy distractions to pull you out of an emotional spiral.
- Activities: Get busy with something that demands your full attention. Do a puzzle, organize a closet, or dive into a craft project.
- Contributing: Shift the focus off yourself by helping someone else. Volunteer for an hour, do a chore for a family member, or make something for a friend.
- Comparisons: Gently put your situation in perspective. Think of a time you successfully handled an even tougher situation, or consider how others are coping with their own immense difficulties.
- Emotions: Generate a different feeling on purpose. Watch a hilarious movie, listen to an uplifting playlist, or read an inspiring story.
- Pushing Away: Give yourself permission to temporarily shelve the problem. Imagine putting it in a box and placing it on a high shelf to deal with when you're calmer.
- Thoughts: Force your mind to do something else. Count backward from 100 by sevens, recite song lyrics, or do a crossword puzzle.
- Sensations: Overload one of your five senses. Take a hot shower, listen to loud music, smell a strong essential oil, or bite into a lemon.
IMPROVE and Radical Acceptance for Finding Peace in the Pain
Where TIPP and ACCEPTS are about immediate crisis survival, the next two skills are about enduring ongoing pain without making it worse.
The IMPROVE skills are about making the present moment just a little more bearable. This includes using Imagery to visualize a safe, calming place; finding Meaning in the suffering; turning to Prayer or a spiritual practice; Relaxing your body; focusing on One thing in the moment; taking a brief mental Vacation; and offering yourself genuine Encouragement.
Radical Acceptance, however, is arguably the most powerful—and challenging—distress tolerance skill of all. It’s about looking reality square in the face and accepting it completely, without judgment or resistance. This doesn't mean you like or approve of the situation. It just means you stop fighting what you cannot change.
"Radical acceptance is the willingness to experience ourselves and our life as it is. A moment of radical acceptance is a moment of genuine freedom." – Tara Brach
This single act of letting go frees up an incredible amount of mental and emotional energy, which you can then redirect toward what you can control: your response.
To make these powerful tools easier to remember, here's a quick cheat sheet summarizing the core DBT distress tolerance skills.
Your DBT Distress Tolerance Skill Cheat Sheet
| DBT Skill Set | Core Purpose | Best Used When… |
|---|---|---|
| TIPP | Rapidly calm your body's crisis response | You're feeling emotionally flooded, panicked, or on the verge of acting on an urge. |
| ACCEPTS | Distract your mind from overwhelming emotions | You're stuck in a negative thought loop and need to create mental space. |
| IMPROVE | Make the current painful moment more tolerable | The crisis isn't acute, but the emotional pain is high and you need to endure it. |
| Radical Acceptance | Stop fighting reality to reduce suffering | You're railing against a painful truth you cannot change in this moment. |
Keep this table handy. Just knowing you have options can make an unbearable moment feel more manageable.
The power of these DBT-based approaches is well-documented. Research shows that distress tolerance is a strong predictor of how well someone can cope with negative emotions. Therapies like DBT can boost a person's tolerance by 30-50% after treatment.
At Altura Recovery, our programs are built around these proven principles. In fact, 85% of our clients report having significantly improved coping skills after just 12 weeks of integrated care. You can discover more insights about the effectiveness of distress tolerance skills and their impact in clinical settings.
How Professional Guidance Can Build Your Resilience

Knowing what distress tolerance skills are is one thing. Actually using them when a real-life crisis hits is another challenge entirely. While self-help is a fantastic start, turning that knowledge into a reliable, real-world practice is much easier with the right support. You don't have to build this kind of resilience alone.
A structured environment, like the outpatient programs at Altura Recovery, can accelerate this journey. It's not just about learning skills in a vacuum; it’s about applying them in a safe space with experts who can guide you through setbacks and celebrate your wins.
A Multi-Layered Approach to Healing
Building lasting emotional resilience requires more than a single type of therapy. At Altura Recovery, we pull from a combination of powerful, evidence-based methods to help you build a robust toolkit for managing distress. Our outpatient programs—including our Intensive Outpatient Program (IOP) and Partial Hospitalization Program (PHP)—are designed to fit into your life while providing the intensive support you need.
We focus on therapies proven to boost what is distress tolerance:
- Dialectical Behavior Therapy (DBT): This is the gold standard for learning concrete distress tolerance and emotion regulation skills.
- Cognitive Behavioral Therapy (CBT): CBT helps you spot and reframe the negative thought patterns that pour fuel on emotional fires.
- Eye Movement Desensitization and Reprocessing (EMDR): For many, low distress tolerance is rooted in past trauma. EMDR is a specialized therapy that helps process those underlying wounds.
The Power of Personalized and Group Support
This therapeutic blend is delivered through both one-on-one and community-oriented models, making sure every angle of your recovery is supported.
Professional treatment provides a safe container for practice. It’s a place to try out new coping skills, make mistakes without judgment, and receive expert feedback to refine your approach for real-world challenges.
Individual therapy sessions allow clinicians to tailor these skills directly to your unique triggers and life circumstances. At the same time, group therapy offers a powerful space to practice new behaviors with peers who truly understand what you're going through.
This combination of personalized attention and community support creates a strong foundation for lasting change, empowering you to build a life defined by resilience, not by reaction.
Frequently Asked Questions About Distress Tolerance
Diving into distress tolerance can bring up a lot of questions. The whole idea can feel backward at first, especially when every nerve in your body is screaming at you to run from emotional pain. To help clear things up, we’ve put together answers to some of the most common questions people ask when they’re starting out.
Think of this as your quick-reference guide for making these powerful skills feel more intuitive and useful in your own life.
Is Distress Tolerance the Same as Ignoring My Feelings?
Not at all—in fact, it's the exact opposite. Trying to ignore or suppress your feelings is like trying to hold a beach ball underwater. Sooner or later, it’s going to pop back up, and usually with a lot more force.
Distress tolerance is about acknowledging your feelings without letting them take over the driver's seat. It's the skill of noticing you feel angry, sad, or anxious, and then choosing a thoughtful response instead of getting swept away by a knee-jerk reaction. The entire practice is built on mindful awareness, not emotional avoidance.
True distress tolerance isn’t about becoming numb. It’s about learning to feel everything and still stay in control of your actions, empowering you to experience your emotions without becoming a victim to them.
This difference is everything. Validating what you feel is always the first step toward managing it effectively.
How Long Does It Take to Improve Distress Tolerance?
Building distress tolerance is a lot like building muscle at the gym. It takes consistent practice, patience, and time. There's no set timeline because everyone’s starting point, challenges, and pace are different.
Some DBT skills, like splashing your face with cold water from the TIPP skill set, can give you immediate relief in a crisis. But achieving real, lasting mastery is a gradual process. The key is consistent effort and, just as important, giving yourself grace when you have a setback.
Working with a therapist can really speed things up. They provide structured lessons, personalized feedback on what’s working, and steady support when the process feels tough.
Can I Practice These Skills on My Own?
You can absolutely start practicing some of the foundational skills by yourself. Simple techniques like paced breathing, using healthy distractions from the ACCEPTS list, or even just practicing a half-smile to shift your mood are great places to begin.
However, for anyone wrestling with addiction, significant trauma, or a co-occurring mental health condition, getting professional guidance is highly recommended. A trained therapist can teach you the skills correctly, help you pinpoint your specific triggers, and provide crucial support when things get overwhelming. That expert guidance is what makes the tools safe and effective enough for lasting success.
What Is the Difference Between Distress Tolerance and Emotion Regulation?
This is a fantastic question, since the two concepts sound similar but do very different jobs. Here’s a simple analogy to clear it up:
- Distress Tolerance: This is your emergency first-aid kit. You use these skills to survive an intense crisis right now without making things worse. They are short-term survival tools designed to get you through the storm.
- Emotion Regulation: This is your long-term wellness plan. These skills are about understanding your emotions, lowering your daily vulnerability to emotional pain, and building a life with more positive experiences.
You truly need both. Distress tolerance skills get you through the immediate storm, while emotion regulation skills help you build a stronger boat so that future storms feel a lot less threatening.
At Altura Recovery, we specialize in helping you build both of these essential toolkits. Our outpatient programs integrate evidence-based therapies like DBT to provide the structured support and expert guidance you need to master these skills and achieve lasting freedom from addiction. If you’re ready to stop reacting and start responding to life’s challenges, learn more about our approach.