Cognitive Behavioral Therapy (CBT) is a practical, no-nonsense form of psychotherapy built on a simple but powerful idea: the way you think directly shapes how you feel and what you do. It’s an evidence-based approach that doesn't just talk about problems; it gives you the skills to actively manage your mind and, in turn, your life.
Demystifying Cognitive Behavioral Therapy

Imagine your mind is like a garden. Over the years, without you really noticing, weeds can start to take over. These are your automatic negative thoughts—the knee-jerk reactions like "I'm going to fail" or "This will never work out." They pop up so fast they feel like facts, and they can easily choke out your confidence, leading to anxiety, frustration, or sadness.
CBT is essentially learning how to tend to this garden. Instead of spending years digging for the deep historical roots of every single weed, CBT hands you practical tools—like a trowel and a hoe—to deal with the ones strangling your garden right now. It operates on the principle that while you can't control every storm that passes through, you absolutely can learn to control how you interpret and respond to it.
The Foundational Triangle
The entire CBT framework rests on what’s often called the "cognitive triangle." This model shows how your thoughts, feelings, and behaviors are locked in a continuous, interconnected cycle. One always influences the others.
- Thoughts: What you tell yourself about a situation (e.g., "I'm terrible at interviews").
- Emotions: The feeling that thought sparks (e.g., anxiety, dread).
- Behaviors: The action you take because of that feeling (e.g., you cancel the interview or perform poorly because you're so nervous).
See how that works? The anxious feeling reinforces the avoidant behavior, which then seems to "prove" the original negative thought was right all along. It’s a self-fulfilling prophecy. CBT teaches you how to step in and break that cycle, most often by starting with the thought itself.
To give you a clearer picture, here’s a quick breakdown of the core components that make CBT so effective.
The Core Components of Cognitive Behavioral Therapy
A quick overview of the foundational elements that make CBT an effective therapeutic approach.
| Component | Description |
|---|---|
| Cognitive Restructuring | The process of identifying, challenging, and replacing distorted or unhelpful thought patterns with more balanced and realistic ones. |
| Behavioral Activation | A technique focused on increasing engagement in positive, rewarding activities to counteract avoidance, withdrawal, and depression. |
| Skills-Based Learning | CBT is educational. Clients learn concrete coping skills, problem-solving strategies, and relaxation techniques they can use independently. |
| Collaborative Approach | The therapist and client work together as a team to set goals, identify problems, and track progress in a structured way. |
| Present-Focused | While past experiences are acknowledged, the primary focus is on solving problems and building skills in the here and now. |
By mastering these elements, you essentially become your own therapist over time.
This isn't about ignoring reality or slapping on a fake "positive thinking" sticker. It’s about cultivating balanced and realistic thinking. You learn to question that initial negative thought, check the evidence for and against it, and find a more helpful perspective.
It’s a collaborative, skills-based journey that equips you with strategies to last a lifetime. To dig deeper into how these principles apply to various challenges, feel free to explore further articles on mental wellness. This active, empowering approach is precisely why CBT stands out as one of the most well-researched and effective therapies available today.
How Your Thoughts Shape Your Reality
Have you ever noticed how two people can go through the exact same event and have completely different reactions? Imagine two colleagues get laid off. One spirals into despair, seeing it as a personal failure. The other feels a rush of relief, viewing it as a long-overdue chance to find more meaningful work.
The layoff itself is just a fact—a neutral event. The difference in their emotional fallout comes down to one thing: their interpretation. This is the absolute core of what is cognitive behavioral therapy. It’s not the situation that dictates how we feel and act, but the story we tell ourselves about it.
This powerful link is mapped out by the cognitive model, a foundational concept in CBT. It’s a simple but profound chain reaction:
Event → Thought → Feeling → Behavior
Think of it like a series of dominoes. An event triggers a thought, that thought sparks an emotion, and the emotion drives an action. Getting a handle on this sequence is the first real step toward gaining control over knee-jerk emotional responses and starting to make more conscious choices.
The Power of Automatic Thoughts
The thoughts that kick off this whole cycle are often lightning-fast and fly completely under our conscious radar. In CBT, we call them automatic negative thoughts (ANTs), a name that perfectly captures their pesky, intrusive nature. These are the reflexive mental scripts that play on a loop in the back of your mind, shaped by years of past experiences and deeply held beliefs.
Because they’re automatic, we almost never stop to question them. We just accept them as the truth, and that’s where the trouble starts. A single unexamined thought can send us spiraling into a wave of painful emotions and self-defeating behaviors.
Key Takeaway: Our immediate, unfiltered thoughts about a situation often have more power over us than the situation itself. Learning to spot these automatic thoughts is the first move toward changing the emotional outcome.
Let’s walk through a real-world example. Say you have a big presentation at work tomorrow. That’s the event. Now, watch how two different automatic thoughts can create two totally different realities.
- Thought: "I'm going to bomb this. Everyone will see I'm a fraud."
- Feeling: This thought immediately triggers a knot of anxiety, fear, and dread in your stomach.
- Behavior: You might put off preparing, stay up all night stewing in worry (which guarantees you’ll be tired), or even call in sick just to escape the perceived judgment.
Now, let's rewind and run a different mental script for the same event:
- Thought: "This is a chance to share what I've been working on. I'm prepared, and I’ll give it my best shot."
- Feeling: This perspective fosters a sense of grounded confidence and readiness.
- Behavior: You calmly review your notes, get a good night's sleep, and walk in ready to deliver the presentation with composure, no matter what happens.
Making the Invisible Visible
The whole point of cognitive behavioral therapy is to make these invisible thought patterns visible. It trains you to become a detective of your own mind, catching those ANTs in the act before they can hijack your emotional state and run the show.
This process isn't about blaming yourself for having negative thoughts—we all do. It’s about building the awareness to pause, identify the thought, and ask a simple question: "Is this thought actually true? Is it helpful?"
Once you can see these patterns clearly, you can start to challenge and reframe them. This is the heart of cognitive restructuring, a cornerstone technique in CBT. You learn to act like a fair-minded judge, examining the evidence for and against your negative thoughts, brainstorming alternative explanations, and swapping distorted thinking with more balanced and realistic interpretations.
The incredible effectiveness of this approach is recognized worldwide. Cognitive Behavioral Therapy is a proven treatment for a whole range of mental health issues, from depression and anxiety disorders to substance abuse. It’s often recommended as a first-line therapy because its benefits are measurable, practical, and lasting. Discover more insights about the growing CBT market on globenewswire.com.
Ultimately, understanding how your thoughts construct your reality gives you the power to start building a new one. You shift from being a passive reactor to life’s events to an active architect of your own mental and emotional well-being.
Practical CBT Techniques You Can Use
Knowing the link between your thoughts, feelings, and actions is one thing. Learning how to step into that cycle and change its direction is another thing entirely. Cognitive behavioral therapy isn't a passive process where you just talk about problems; it’s a skills-based approach that hands you a toolkit for managing your own mind.
These techniques are the practical, hands-on tools you learn to use, both in a therapist's office and in your daily life. They turn abstract ideas into concrete actions. Instead of just knowing your thoughts are unhelpful, you learn exactly what to do about them. Let’s break down some of the most powerful and widely used strategies in the CBT toolkit.
Challenge Your Thoughts With Cognitive Restructuring
Cognitive restructuring is the absolute cornerstone of CBT. Think of it as becoming a detective for your own mind. The goal is to catch, question, and reframe the automatic negative thoughts (ANTs) that pop up and trigger emotional distress. This isn't about forcing yourself to "just think positive." It's about learning to think realistically and flexibly.
It starts with catching the thought the moment it happens. Let's say you make a small mistake at work. The automatic thought might be, "I'm a complete failure." Instead of just accepting that as a fact, you put it on trial.
You challenge this thought by asking a few simple but incredibly powerful questions:
- What's the evidence for this thought? "I made one mistake on this report."
- What's the evidence against it? "I've successfully completed dozens of reports before. My boss gave me positive feedback last week. This one mistake doesn't erase all my past successes."
- What’s a more balanced way of looking at this? "I made a mistake, which is frustrating, but it's a normal part of being human. I can learn from it and fix it."
This process systematically takes apart distorted thinking. By looking at the actual evidence, you shift from a harsh, black-and-white judgment to a much more compassionate and accurate view of the situation.
Break the Cycle With Behavioral Activation
When people feel depressed or anxious, their first instinct is often to pull back. They stop doing the things they once enjoyed, which only digs the hole of hopelessness and lethargy deeper. Behavioral activation is a direct and powerful counter-attack designed to break this cycle of avoidance and isolation.
The core idea couldn't be simpler: action precedes motivation. Instead of waiting until you feel like doing something, you schedule and engage in meaningful activities first. The positive feelings follow the action.
Here’s how it works in practice:
- Identify Activities: You and a therapist will brainstorm a list of activities that are either enjoyable, rewarding, or simply align with your values—even if you have zero desire to do them right now. This could be anything from a 10-minute walk to calling a friend or spending a bit of time on a hobby.
- Schedule Them: Just like a doctor's appointment, you put these activities into your weekly calendar. The key is to start small. The goal is to build momentum, not to overwhelm yourself.
- Monitor Your Mood: After you do the activity, you rate your mood or sense of accomplishment. This creates a powerful feedback loop, showing you in real-time that your actions have a direct, positive impact on how you feel.
Behavioral activation is especially effective for depression because it directly targets the withdrawal and inactivity that keep the illness going. It helps you rebuild a life filled with purpose and positive reinforcement, one small step at a time. For many, mastering these practical skills is key to developing effective coping strategies for anxiety and depression that truly last.
This visual shows the powerful difference between a negative cycle of withdrawal and a positive one driven by behavioral activation.
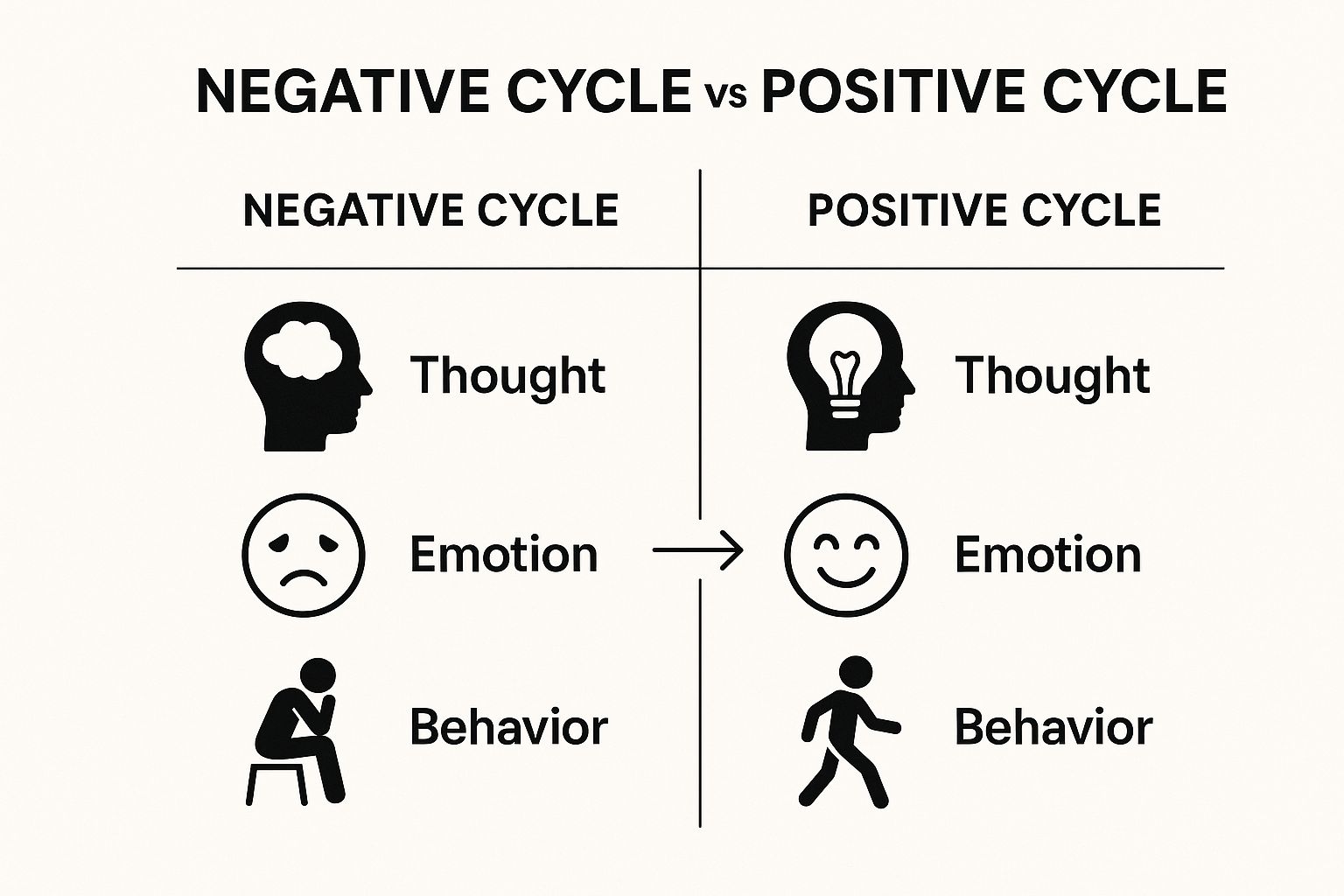
As the infographic makes clear, a single shift in behavior—from avoidance to engagement—can completely reverse the emotional downward spiral.
Confront Your Fears With Exposure Therapy
For anxiety disorders, phobias, and PTSD, avoidance is the fuel that keeps fear alive. The more you avoid something, the bigger and scarier it becomes in your mind. Exposure therapy is a structured, evidence-based technique for gently and safely confronting those fears head-on.
The whole process is gradual and controlled, making sure you are never overwhelmed. It works on the principle of habituation—the more you're exposed to something you fear without anything bad happening, the less your brain and body will react with panic.
Expert Insight: The goal of exposure therapy isn't to get rid of anxiety completely. It's to build your confidence in your ability to manage it. You learn through direct experience that you are far more capable than your fear tells you.
Imagine someone with a severe fear of dogs. A therapist wouldn't start by putting them in a room with a Great Dane. Instead, they would build an "exposure hierarchy," which is just a list of feared situations ranked from least to most scary.
It might look something like this:
- Step 1: Look at a picture of a small dog.
- Step 2: Watch a short video of a dog playing.
- Step 3: Stand across the street from a calm dog on a leash.
- Step 4: Stand on the same sidewalk as the leashed dog.
- Step 5: Briefly pet the dog with the owner's help.
You only move to the next step once the anxiety at the current step has come way down. This gradual process rewires the brain's fear response, teaching it that the feared situation is actually safe. Through these repeated exposures, the fear shrinks, and your world, once limited by avoidance, starts to open back up again.
CBT offers a diverse range of tools because no two people are the same. While one person may need to focus on restructuring their thoughts, another might get the most benefit from changing their behaviors first. The table below highlights some common techniques and where they are most often applied.
Common CBT Techniques and Their Applications
| Technique | Primary Goal | Commonly Used For |
|---|---|---|
| Cognitive Restructuring | To identify and challenge irrational or negative thought patterns. | Depression, Generalized Anxiety, Panic Disorder |
| Behavioral Activation | To increase engagement in positive and meaningful activities. | Depression, Social Withdrawal |
| Exposure Therapy | To gradually confront feared objects or situations in a safe way. | Phobias, PTSD, OCD, Social Anxiety |
| Journaling & Thought Records | To track thoughts, feelings, and behaviors to identify patterns. | Most anxiety and mood disorders |
| Relaxation & Mindfulness | To reduce physical symptoms of anxiety and increase present-moment awareness. | Panic Disorder, Stress, Anxiety |
Ultimately, a good therapist helps you select and master the right combination of these strategies. The real power of CBT lies in its practicality—it equips you with real skills you can use for the rest of your life.
Mental Health Conditions CBT Can Improve
Cognitive behavioral therapy isn't a single, rigid prescription. It’s more like a flexible framework that can be adapted to an incredibly wide range of mental health challenges. The real power of CBT lies in this versatility—its core principles of identifying and changing unhelpful thought and behavior patterns can be tailored to get to the root of what's causing the problem.
Rather than just listing off conditions, it's more useful to see how CBT actually works for specific issues. It provides targeted, practical tools that address the underlying mechanics of a disorder, creating a clear path toward relief and lasting recovery.
Anxiety Disorders and Panic Attacks
Anxiety is often fueled by a one-two punch: the mental habit of "catastrophizing"—where your mind immediately jumps to the worst-case scenario—and the behavioral habit of avoiding situations that trigger fear. CBT goes after both of these head-on.
For someone experiencing panic attacks, the therapy focuses on changing how they interpret the terrifying physical sensations. For example, a racing heart isn’t treated as a sign of a heart attack but is reframed as what it is: a normal, harmless adrenaline response. Through gradual exposure, a person learns they can handle these feelings without needing to flee, which slowly dismantles the fear itself.
With generalized anxiety, CBT helps people catch their core worries and honestly assess how likely they are to come true. By challenging the distorted thoughts that fuel constant dread, they learn to separate productive problem-solving from the exhausting spin cycle of rumination.
Depression and Mood Disorders
Depression often traps people in a heavy trio of negative beliefs: a negative view of themselves, the world, and the future. These thoughts feel overwhelmingly true, leading to withdrawal, low energy, and a loss of interest in everything. CBT uses a two-pronged approach to break this cycle.
- Cognitive Restructuring: This technique helps you challenge the persistent thoughts of hopelessness and worthlessness that are hallmarks of depression. A therapist guides you to find evidence that contradicts these toxic beliefs, slowly helping you shift from a mindset of harsh self-criticism to one of balanced self-assessment.
- Behavioral Activation: This is a powerful tool that directly fights the lethargy and isolation of depression. It involves scheduling small, meaningful activities back into your life, based on the principle that action precedes motivation. Even something as simple as a short walk or a quick call to a friend can provide a small lift that starts to reverse the downward spiral.
By actively changing behaviors, you create new, positive experiences that serve as direct evidence against the belief that nothing will ever get better. It’s tangible proof that your actions can directly influence your mood.
Post-Traumatic Stress Disorder (PTSD)
Trauma can shatter a person's sense of safety, leaving them with intrusive memories, hypervigilance, and a powerful urge to avoid anything that reminds them of the event. Trauma-focused CBT (TF-CBT) is a specialized approach designed to help people process these experiences in a safe, structured way. For a deeper look at this, exploring the principles of https://alturarecovery.com/blog/what-is-trauma-informed-therapy can provide valuable context on creating a safe therapeutic space.
TF-CBT helps individuals confront and re-process traumatic memories, which reduces their emotional intensity over time. It also focuses on correcting the distorted beliefs that often take root after trauma, such as blaming oneself or seeing the entire world as dangerous.
Other Conditions Where CBT Shines
The applications of CBT extend far beyond these examples. Its structured, skills-based approach makes it highly effective for a variety of other challenges:
- Obsessive-Compulsive Disorder (OCD): A specific type of CBT called Exposure and Response Prevention (ERP) is considered the gold-standard treatment for OCD.
- Eating Disorders: CBT helps individuals challenge distorted thoughts about body image, food, and self-worth while working to modify unhealthy eating behaviors.
- Substance Use Disorders: As a cornerstone of addiction treatment, CBT helps people identify their triggers, manage cravings, and build healthier coping skills to prevent relapse.
- Attention-Deficit/Hyperactivity Disorder (ADHD): While it's not a cure, CBT can equip adults with ADHD with practical skills for organization, time management, and regulating their emotions. For more on this, understanding ADHD, its symptoms, and treatments offers additional context.
This remarkable adaptability is why CBT is one of the most widely practiced and well-researched psychotherapies available today. It offers both hope and practical tools to people facing a broad spectrum of mental health concerns.
How CBT Is Becoming More Accessible Than Ever
The world of mental healthcare is changing, and Cognitive Behavioral Therapy is right at the heart of the shift. For decades, CBT was something you could only get in a traditional, face-to-face session. While that model works, it came with plenty of hurdles—cost, scheduling headaches, and the stigma that often kept people from walking into a therapist’s office in the first place.
Thankfully, those barriers are coming down. Today, evidence-based mental health support is easier to reach than it has ever been, thanks in large part to technology. The rise of telehealth and specialized mental health apps has put powerful CBT tools directly into the hands of millions. What once required a weekly trip across town can now happen from the comfort of your home, on a schedule that actually works for you.
The Digital Revolution in Mental Healthcare
Digital platforms have completely changed the game. From video sessions with licensed therapists to guided self-help programs, technology has made expert care far more convenient and discreet.
This has been a massive breakthrough for people who might otherwise have gone without support. If you live in a rural area, have mobility issues, or are a busy professional juggling a dozen responsibilities, connecting with a qualified CBT practitioner is no longer a logistical nightmare. This explosion in accessibility means more people can get the right help, right when they need it.
For instance, many modern treatment centers now offer flexible programs that blend in-person and virtual care. Someone might join an intensive outpatient program that mixes group therapy with individual CBT exercises completed through a secure online portal. It’s a hybrid approach that delivers both structure and real-world convenience.
The Economic and Systemic Embrace of CBT
It isn’t just about new tech. CBT’s accessibility has also been turbocharged by its proven track record and economic efficiency. Because it’s structured, goal-oriented, and backed by a mountain of evidence, healthcare systems and insurance providers have increasingly thrown their weight behind it.
The economic impact of Cognitive Behavioral Therapy reflects its growing importance in global healthcare. In North America, which holds the largest market share at around 40%, the therapy generated approximately USD 3 billion in revenue by the mid-2020s, with annual growth near 10%.
In Europe, CBT services make up about 28% of the behavioral therapy market. There's a growing push for insurance coverage and public funding, making it a viable option for just about everyone. You can learn more about these market trends on cognitivemarketresearch.com. This kind of financial backing is a clear signal that CBT is seen not just as a therapy, but as a smart investment in public health.
The Rise of AI and Self-Guided Tools
Another exciting frontier is the wave of AI-powered mental health tools and self-guided CBT apps. These resources offer another layer of support, providing immediate access to exercises and coping strategies whenever you need them.
These tools aren't meant to replace therapists. Instead, they supplement treatment and make foundational skills more available to everyone. They often include features like:
- Guided Journals: To help you get into the habit of spotting and challenging negative thoughts.
- Mood Trackers: Which let you connect the dots between your thoughts, activities, and emotional states over time.
- Behavioral Activation Planners: That nudge you to schedule and follow through with positive, rewarding activities.
These innovations are making the core principles of what is cognitive behavioral therapy more democratic. They empower you to take an active role in your own mental wellness journey, offering skill-building resources you can use anytime, anywhere. This blend of professional guidance and accessible technology is truly defining the future of mental healthcare.
Walking into your first therapy session can feel a lot like stepping into the unknown, which, ironically, is often the very thing that brings people to therapy in the first place. But here's the good news: a Cognitive Behavioral Therapy (CBT) session isn't some mysterious, intimidating ordeal. It’s a structured, collaborative meeting where you and your therapist start to function as a team right from the get-go.
Your first appointment is really about two things: assessment and connection. It’s a two-way street. You’re getting a feel for the therapist and their style, and they’re beginning to understand your unique challenges and what makes you tick.
Expect to talk about what brought you in, a bit about your personal history, and what you’re hoping to walk away with at the end of this process. This isn’t just venting; it’s the crucial information-gathering that helps your therapist shape an action plan that’s actually built for you.
Setting the Stage for Success
Unlike some other forms of talk therapy that can feel more open-ended, CBT is highly goal-oriented. From the very beginning, the focus is on defining clear, measurable objectives. You won’t just talk about "feeling less anxious." You'll work together to nail down exactly what that looks like in your day-to-day life.
For instance, a goal might sound something like this: "To reduce panic symptoms in social situations from three times a week to once a week within the next two months."
That level of specificity is key because it gives both of you a clear benchmark for success. The first session is where this process kicks off. You'll likely leave with a shared understanding of the problems you want to tackle and a rough idea of how you'll approach them as a team.
A Collaborative Partnership: Think of your CBT therapist as a personal trainer for your mind. They've got the expertise, the guidance, and the tools. But you're the one who does the work—both in and out of sessions—to build up that mental strength and resilience.
The Structure of a Typical Session
Most CBT sessions follow a predictable, three-part structure. This isn't meant to be rigid or robotic; it's designed to keep things focused and make sure you're always moving forward. This consistent format helps the whole process feel safe and productive.
A session usually breaks down like this:
- A Check-In: You’ll kick things off by briefly going over your week. You’ll discuss your mood and talk about any "homework" or skills you practiced since your last meeting.
- Setting an Agenda: This is a team effort. You and your therapist will decide together what specific issues or skills you want to zero in on during that day's session.
- Learning and Practicing: This is the heart of the session. You’ll learn a new CBT concept or technique, practice it right there with your therapist’s guidance, and then create a game plan for how you’ll apply it in the week ahead.
It can also be helpful to understand how different therapeutic approaches work; our guide on individual therapy vs group therapy offers some extra context. Ultimately, that first CBT session is all about demystifying the process, replacing uncertainty with a clear, collaborative roadmap for change.
Common Questions About Cognitive Behavioral Therapy
When you're looking into something like cognitive behavioral therapy, the theoretical stuff is great, but the practical questions are what really matter. How long will this take? Can I do it without medication? How is this any different from just… talking to a therapist?
Getting clear on these real-world details helps you decide if CBT is the right next step for you. Let's tackle some of the most common questions head-on.
How Long Does CBT Usually Take?
Unlike some therapies that can be an open-ended exploration, CBT is built to be a short-term, goal-oriented treatment. The whole point is to give you a set of practical skills you can use for the rest of your life, not to create a long-term dependency on therapy.
Everyone's journey is different, of course, but a typical round of CBT usually lasts for 12 to 20 sessions. For very specific issues, some people see incredible progress in as few as 6 to 8 weeks. The timeline is always shaped by your specific needs, your goals, and the challenges you're working through.
The ultimate goal of CBT is to help you become your own therapist. Its finite structure is deliberate—it’s designed to empower you with coping strategies that last long after your final session.
Can CBT Work Without Medication?
Absolutely. For many conditions, especially mild-to-moderate depression and a whole spectrum of anxiety disorders, CBT has proven to be incredibly effective all on its own. The impact isn't just powerful; it's durable.
Study after study shows that the benefits of CBT can be just as significant as those from medication. And because it teaches you lasting skills for managing your own thoughts and behaviors, CBT often has a lower relapse rate compared to using medication alone. That said, for more severe symptoms, a doctor or psychiatrist might recommend a combined approach, using both medication and therapy to give you the most comprehensive support possible.
How Is CBT Different From Traditional Talk Therapy?
The biggest difference comes down to structure and focus. Traditional talk therapies often take a deep dive into your past, exploring the historical roots of your feelings in a process that can be quite open-ended.
CBT, on the other hand, is intensely present-focused and action-oriented. While your past is acknowledged as important context, the real work is about solving the problems you have right now. It directly targets the unhelpful thought patterns and behaviors that are causing you distress today.
It's a very hands-on and collaborative process. The key distinctions are:
- Structure: Sessions are agenda-driven to make sure you're always making progress.
- Action: Therapy includes skill practice and "homework" between sessions to help you apply what you learn in the real world.
- Focus: The emphasis is squarely on making tangible changes in the here and now.
This practical, skills-based approach is what makes CBT a uniquely empowering form of therapy.
At Altura Recovery, we specialize in using evidence-based methods like CBT to create personalized treatment plans that foster real, sustainable change. If you're ready to build the skills for long-term well-being, our compassionate team is here to guide you. Learn more about our outpatient programs.