Withdrawal symptoms are the collection of physical and psychological responses your body unleashes when you stop or cut back on a substance it has learned to depend on. This isn't a sign of weakness; it's a biological reaction that happens because your brain has fundamentally adapted to the presence of a drug and now has to figure out how to function without it.
Understanding Your Body's Response to Sobriety
When you consistently use a substance like alcohol, opioids, or benzodiazepines, your body doesn't just tolerate it—it actively rewires itself in a process called neuroadaptation.
Think of your brain as a finely tuned orchestra, naturally producing its own chemicals—like dopamine for pleasure or GABA for calm—to keep everything in balance. When an outside substance comes in, it's like a blaring new instrument that forces the whole orchestra to adjust. To maintain equilibrium, your brain dials down its own production of these natural chemicals. Over time, it learns to rely on the substance just to feel "normal."
The Sudden Silence
So, what are withdrawal symptoms in this context? They’re what happens when that loud, external instrument is suddenly yanked away.
The orchestra is left in an abrupt silence, completely unprepared to play its own music at the right volume. Your brain scrambles to ramp its internal chemical production back up, but this recalibration process isn't instant.
This internal chaos is what triggers the flood of physical and psychological effects we call withdrawal. It's a predictable, biological signal that your body is fighting to find its natural rhythm again.
Physical vs. Psychological Symptoms
The symptoms of withdrawal generally fall into two main categories, although they often overlap and feed into one another. Knowing what to look for can help demystify the initial stages of recovery.
Physical vs Psychological Withdrawal Symptoms at a Glance
This table offers a clear overview of the two main categories of withdrawal symptoms, helping you quickly identify what you or a loved one might experience.
| Symptom Category | Common Examples |
|---|---|
| Physical Symptoms | Nausea, vomiting, muscle aches, sweating, tremors, headaches, fatigue, increased heart rate. |
| Psychological Symptoms | Anxiety, depression, irritability, intense cravings, insomnia, confusion, mood swings. |
Understanding these distinct yet connected symptoms is the first step toward preparing for a safe and supported detox process.
The intensity of withdrawal is the body's way of signaling just how much it had to adapt to the substance's presence. It is a direct reflection of the healing process beginning.
This adjustment period is an unavoidable—and critical—first step on the path to sobriety. The symptoms, while incredibly difficult, are tangible proof that your body is working hard to heal and regain its natural balance. Recognizing this empowers you to seek the right support and ensures a safer, more sustainable journey toward lasting recovery.
Navigating the Physical Symptoms of Withdrawal
When your body starts detoxing, the physical symptoms are usually the first and most intense hurdles you'll face. These aren't just minor annoyances; they can feel all-consuming, making it nearly impossible to focus on anything besides how sick you feel. Getting a handle on what these symptoms are—and why they’re happening—is the first real step toward managing them.

Think of it like this: your central nervous system has been running with the emergency brake on, constantly suppressed by a substance. When you suddenly take that substance away, the system doesn't just return to normal. It lurches forward violently. That abrupt jolt is what triggers the cascade of physical reactions.
As rough as these experiences are, they are tangible proof that your body is fighting to find its natural balance again. It’s not a sign of failure but a powerful signal that the healing process has begun.
Common Physical Manifestations
While the specifics change depending on the drug, a few common physical challenges pop up for almost everyone. Each one is a sign of your body trying to recalibrate its internal chemistry without the substance it learned to rely on.
- Flu-Like Symptoms: So many people describe early withdrawal as the worst flu of their life. We're talking muscle and bone aches, a runny nose, and a deep sense of malaise that makes even getting out of bed feel like climbing a mountain.
- Gastrointestinal Distress: Nausea, vomiting, and diarrhea are incredibly common. Your digestive system is tightly linked to your nervous system, so when one is in chaos, the other follows suit. This makes it tough to stay hydrated and nourished when your body needs those resources the most.
- Tremors and Shakes: That uncontrollable shaking, especially in the hands, is a classic sign. It happens as your central nervous system gets overexcited and loses its ability to regulate fine motor control.
These symptoms often hit their peak within the first 72 hours, though they can linger. This is the most acute phase of your body’s rebellion.
The Autonomic Nervous System in Overdrive
Many of the most jarring physical symptoms come from the dysregulation of your autonomic nervous system—the part of you that controls all the background functions like heart rate, body temperature, and blood pressure.
During withdrawal, this system goes completely haywire.
The body's "fight or flight" response, which was chemically suppressed, rebounds with overwhelming force. This leads to a racing heart, profuse sweating, and wild temperature swings that leave you freezing one minute and burning up the next.
Pounding headaches are also frequent, caused by chaotic changes in blood flow and pressure inside the brain as it adjusts. This combination of internal turmoil creates a state of constant physical agitation that makes rest feel impossible. It’s a physiological storm that you have to weather with proper support and care.
Overwhelming Fatigue and Sleep Disruption
One of the most profound physical symptoms is a deep, bone-crushing fatigue. Your body is pouring a massive amount of energy into healing and rebalancing, leaving you feeling utterly drained.
But here's the cruel twist: despite the exhaustion, sleep is often nowhere to be found. Insomnia is a hallmark of withdrawal because that overactive nervous system won't let your brain shut down. This creates a vicious cycle where your body is desperate for rest, but the symptoms themselves keep it just out of reach.
This lack of sleep can amplify every other symptom, from muscle aches to psychological distress. It's a key reason why managing the physical side of withdrawal is so critical for a successful recovery journey. It helps to reframe these brutal experiences as signs of healing—that perspective can give you the strength to push through this challenging but temporary phase.
Managing the Emotional and Psychological Rollercoaster
While the physical side of withdrawal feels like an all-out war on your body, the psychological battle is often the more grueling, long-lasting fight. These are the invisible wounds—intense anxiety, deep depression, and sudden irritability—that can kick up an emotional storm that feels impossible to navigate.
Understanding these psychological symptoms is key to preparing for and overcoming them. This emotional upheaval isn’t a sign of personal failure; it's a direct result of brain chemistry in total disarray.
Your brain, having grown dependent on a substance to regulate mood, is now struggling to produce its own stabilizing chemicals. The result? A volatile internal state where emotions swing wildly without warning. This is the phase where the risk of relapse becomes incredibly high. The mind screams for a quick fix, for any way to silence the noise and feel normal again, even just for a moment. That’s why professional mental health support during detox isn't just helpful—it's a critical lifeline.
The Invisible Struggle of Withdrawal
The psychological symptoms of withdrawal are often more isolating than the physical ones. A loved one can see you shaking, but they can't see the crushing weight of depression or the panic attack brewing just beneath the surface. This internal struggle can make you feel completely alone.
Here are some of the most common emotional and psychological challenges you might face:
- Intense Anxiety and Panic: This isn't just everyday worry. Withdrawal can trigger a profound, constant sense of dread, racing thoughts, and even full-blown panic attacks that come out of nowhere.
- Deep Depression and Anhedonia: A heavy, suffocating sadness is common. This is often paired with anhedonia, the inability to feel pleasure, which can drain all the color from life, making everything feel gray and meaningless.
- Extreme Irritability and Agitation: Small frustrations can trigger explosive anger. This happens because the brain’s ability to manage impulse control and emotional responses is temporarily offline.
- Cognitive Fog: Concentration can feel impossible. You might struggle with your memory, thinking clearly, and making simple decisions, which only adds to the frustration and sense of incompetence.
These symptoms create a powerful barrier to recovery, making it feel like you are losing your mind. It’s absolutely essential to remember these are temporary chemical imbalances, not who you are.
Rebound Anxiety and Persistent Cravings
One of the toughest challenges is something called rebound anxiety. If you used a substance like alcohol or benzodiazepines to calm your nerves, your brain dialed down its own production of calming neurotransmitters to compensate. When you take the substance away, the nervous system overcorrects, launching you into a state of anxiety far more intense than what you originally experienced.
It's like holding a beach ball underwater. For a long time, the substance kept the pressure on. When you let go, the ball doesn't just surface—it shoots into the air with explosive force. That’s rebound anxiety.
At the same time, cravings become a constant psychological torment. They're more than just a desire to use; they are intrusive, hijacking thoughts that can demolish your focus and willpower. These cravings are often triggered by people, places, or even emotions tied to past use, making them incredibly difficult to escape. It's also worth noting that similar experiences can happen with prescribed medications; understanding the discontinuation symptoms of antidepressants like Escitalopram can help manage the emotional impact when stopping those treatments, too.
Why Professional Support Is Essential
Trying to navigate this emotional rollercoaster alone is an unfair fight. The psychological symptoms of withdrawal can distort your thinking, convincing you that recovery is impossible or that you're just not strong enough. This is precisely why professional mental health support is so critical.
At Altura Recovery, our clinicians provide the tools needed to manage this turmoil. Through evidence-based therapies like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), you learn to identify, challenge, and reframe the destructive thought patterns that fuel anxiety and depression.
This support helps you build healthy coping mechanisms to weather the emotional storm without turning back to a substance. For families, understanding these dynamics is just as important. Knowing how to support a loved one can make all the difference, which is why resources on how to help an alcoholic spouse can be so valuable. Ultimately, this therapeutic foundation is what transforms a painful detox into the very first step toward lasting emotional wellbeing.
How Withdrawal Timelines Differ by Substance
Understanding the symptoms of withdrawal is just the starting line. The real roadmap to recovery comes from knowing how those symptoms unfold over time, and that timeline looks dramatically different depending on the substance involved.
There’s no one-size-fits-all schedule for this process. The experience is shaped by the specific drug, how long it was used, and your own unique health. Each substance rewires the brain and body differently, so the path back to balance—the withdrawal—follows its own distinct pattern. For some, it’s a short, intense physical fight. For others, it’s a longer, more psychological marathon. Knowing what to expect demystifies the process, cuts down on the fear, and empowers you to get the right level of help when you need it most.
Alcohol Withdrawal Timeline
Alcohol withdrawal is in a class of its own because, without medical supervision, it can be fatal. After being suppressed by alcohol for a long time, the central nervous system can rebound with a dangerous, uncontrolled hyperactivity.
- First 6-12 Hours: The first signs usually appear here—anxiety, nagging headaches, and waves of nausea.
- 12-24 Hours: Things can ramp up quickly. Hand tremors (the "shakes") may start, and in some cases, hallucinations can occur.
- 24-48 Hours: This is the highest-risk window for seizures, making medical monitoring critical.
- 48-72 Hours: The risk of delirium tremens (DTs) emerges. This is a medical emergency marked by severe confusion, a racing heart, high blood pressure, and fever. It requires immediate hospital care.
Most of the acute physical storm subsides after the first week. However, the psychological aftershocks, like anxiety and insomnia, can linger for much longer.
Opioid Withdrawal Timeline
Opioid withdrawal is notorious for being one of the most physically grueling experiences, often described by those who’ve endured it as being profoundly "dope sick." The statistics paint a stark picture: medical experts estimate that around 85% of people who misuse opioids will face these debilitating symptoms when they try to stop.
Globally, the World Health Organization reported that about 60 million people used opioids in 2021. The consequences are devastating, with opioids linked to nearly 80% of the 600,000 drug-related deaths in 2019. You can explore more detailed findings on opioid withdrawal and its management on ncbi.nlm.nih.gov.
Symptoms can kick in just hours after the last dose: muscle aches, nausea, vomiting, diarrhea, sweating, chills, insomnia, and an overwhelming sense of anxiety. This peaks around days 2-3 and can last for a week or more.
While opioid withdrawal is rarely life-threatening on its own, the sheer physical and emotional agony makes it incredibly difficult to get through without support. This intense discomfort is one of the biggest reasons people relapse—they return to the drug just to make the pain stop.
The exact timeline depends on whether the drug is short-acting, like heroin, or long-acting, like methadone. For short-acting opioids, the acute phase typically lasts about 7-10 days.
The infographic below shows how the psychological battle can shift over the first few weeks.
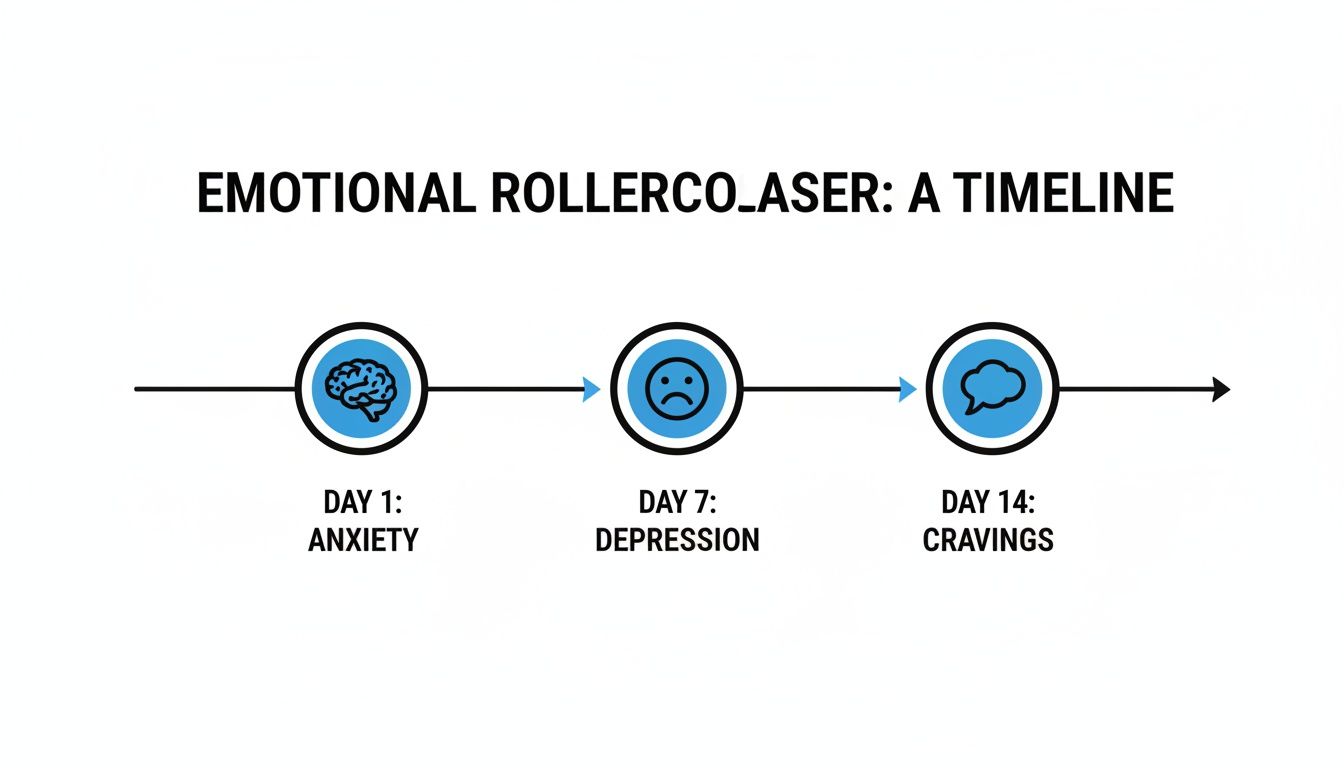
As you can see, while intense anxiety might be the first big challenge, a deeper depression and relentless cravings often become the main obstacles as the weeks progress.
Benzodiazepine Withdrawal Timeline
Withdrawal from benzodiazepines—medications like Xanax or Valium—is known for being a long, drawn-out, and often unpredictable ordeal. Much like with alcohol, stopping without a doctor's guidance can be dangerous because of the high risk of seizures.
The timeline often unfolds in distinct phases:
- Early Withdrawal (1-4 days): "Rebound" symptoms are common first signs, where the original anxiety and insomnia come roaring back.
- Acute Withdrawal (10-14 days, but can be longer): This is where the full spectrum of symptoms hits, including severe anxiety, panic attacks, tremors, muscle pain, and even distorted perceptions.
- Protracted Withdrawal (months to years): A tough reality for many is Post-Acute Withdrawal Syndrome (PAWS). Here, symptoms like anxiety, brain fog, and depression can appear in waves, coming and going for a very long time.
Because many benzodiazepines have a long half-life, the body takes much longer to clear them, making the entire withdrawal process far more prolonged than with many other substances.
Stimulant Withdrawal Timeline
When it comes to stimulants like cocaine and methamphetamine, the withdrawal battle is fought mostly in the mind. While there are physical symptoms, they are usually far less severe than what you see with opioids, alcohol, or benzos.
The process typically begins with an intense "crash."
- First 24-72 Hours: The crash is defined by an overwhelming sense of fatigue, a ravenous appetite, and a deep, heavy depression or apathy. Cravings during this initial stage are incredibly powerful.
- Week 1-2: The extreme exhaustion might lift a bit, but it's often replaced with volatile mood swings, irritability, and an inability to feel any pleasure at all (a condition called anhedonia). Sleep is usually still a mess.
- Weeks 3-4 and Beyond: The psychological symptoms, especially depression and cravings, can stick around for weeks or even months. The biggest challenge here is navigating the emotional lows and finding healthy ways to cope without turning back to the substance.
The severity is often tied directly to the pattern of use. Someone coming off a multi-day binge, for instance, is likely to face a much harder and longer crash. This is why knowing the details of what withdrawal symptoms are for each substance is so crucial—it helps create a realistic and effective path toward healing.
Finding Safe and Effective Professional Support
Trying to ride out withdrawal on your own isn't just tough—it can be downright dangerous. When your body and mind are screaming for relief, the risk of relapse is sky-high. This is where getting professional support becomes less of a helpful option and more of a critical lifeline.

Stepping into a structured program means you’re in a safe, controlled environment where medical experts manage your symptoms. It takes the guesswork and isolation out of the equation, replacing them with proven strategies and compassionate care. This support is the foundation that gets you through the roughest phase safely and sets you up for the real work of recovery.
The Role of Medical Detox and Medication-Assisted Treatment
For many, the first step is medical detox. This is more than just stopping; it's a medically supervised process where your body can recalibrate safely. For substances like alcohol or benzodiazepines, this isn't negotiable—it’s essential for preventing life-threatening complications like seizures.
To make the process as comfortable as possible, clinicians often use Medication-Assisted Treatment (MAT). This approach uses specific, FDA-approved medications to:
- Dial down the intensity of painful or dangerous withdrawal symptoms.
- Quiet the intense cravings that can so easily derail the best intentions.
- Stabilize your brain chemistry, helping your body find its footing again more gently.
MAT significantly boosts the odds of getting through detox successfully, creating a much stronger bridge to the next phase of your treatment.
Think of MAT as a guide rope on a treacherous mountain path. You still have to do the climbing, but the rope provides crucial stability and safety, preventing a catastrophic fall during the most difficult parts of the ascent.
For those seeking direct medical attention and oversight during recovery, a doctor on call service can also provide discreet and immediate assistance, offering another layer of support in the journey.
Structuring Your Recovery Journey
Once your body is stabilized, the real healing can begin. Recovery programs aren't one-size-fits-all; they come in different levels of intensity to meet you exactly where you are. This step-down approach ensures you get the right amount of support as you slowly and steadily regain your independence.
Partial Hospitalization Programs (PHP)
A PHP is a highly structured option, often requiring you to be at the facility for several hours a day, five days a week. It’s perfect for those who need more support than a typical outpatient program but don’t require 24/7 residential supervision. You get an immersive therapeutic environment but still get to go home at night.
Intensive Outpatient Programs (IOP)
An IOP delivers a robust level of care with a bit more flexibility. You’ll typically meet for a few hours a day, several days a week, which allows you to keep up with work, school, or family life. It’s a great way to start putting your new recovery skills into practice in the real world.
At Altura Recovery, our outpatient programs weave together multiple therapeutic approaches to build a strong foundation for sobriety:
- Individual Therapy: One-on-one sessions to get to the personal root causes of addiction.
- Group Therapy: Building a community and learning from the shared experiences of others. Our guide to substance abuse group ideas shows how these sessions create connection and growth.
- Psychiatric Care and Medication Management: Ongoing support for any co-occurring mental health conditions.
This blend of medical oversight, expert therapy, and peer support creates a powerful framework for not just surviving withdrawal, but building a resilient and fulfilling life in recovery.
Common Questions About Withdrawal Symptoms
When you're staring down the first few days of sobriety, your mind is probably racing with questions. It's a time filled with uncertainty, and getting clear, straightforward answers can make all the difference when things feel shaky. Here are some of the most common concerns we hear from people and their families as they face withdrawal.
Can I Just Manage Withdrawal Symptoms at Home on My Own?
It's completely normal to want to handle things privately, but trying to go through withdrawal alone isn't just tough—it can be downright dangerous.
For certain substances, especially alcohol and benzodiazepines, stopping cold turkey without medical help can trigger life-threatening complications like seizures. Even with other drugs, the physical and psychological pain can be so intense that the urge to use again just to make it stop becomes overwhelming. That risk of relapse is incredibly high.
Professional programs, including flexible outpatient options like those at Altura Recovery, exist for this exact reason. We provide critical medical supervision, medications to take the edge off the worst symptoms, and therapy to help you navigate the emotional storm. It’s all done in a safe environment, creating a solid foundation so you can heal without unnecessary risk.
How Long Do Withdrawal Symptoms Actually Last?
There's no single, one-size-fits-all answer here. The timeline for withdrawal really depends on the specific substance, how long and how much you were using, and your own unique health profile. But, we do see some general patterns.
- The Acute Phase: This is the initial wave where symptoms are most intense. For substances like opioids or alcohol, this period often peaks within 72 hours and can last for about a week.
- The Protracted Phase: Some substances, like benzodiazepines, have a much longer runway. Acute symptoms can stick around for several weeks or even longer.
- Post-Acute Withdrawal Syndrome (PAWS): Long after the physical storm has passed, many people experience PAWS. This is where less intense, but still frustrating, emotional and psychological symptoms—like mood swings, anxiety, and trouble sleeping—can pop up in waves for months.
A good treatment plan is designed to guide you through all of these phases, not just the first few days. It provides ongoing support to help you manage lingering symptoms and feel steady on your feet long-term.
The goal isn't just to get through detox, but to build the skills to navigate the entire recovery timeline. This includes learning to cope with lingering symptoms and potential triggers down the road.
What Is the Difference Between Detox and Rehab?
People often use "detox" and "rehab" interchangeably, but they're two very different—and equally essential—stages of recovery. Knowing the distinction helps clarify the road ahead.
Detoxification (Detox) is always the first step. Its one and only job is to help you safely clear the substance from your body while managing the immediate physical and psychological symptoms of withdrawal. Think of it as stabilizing the patient in the ER. The goal is to get you physically stable under medical supervision.
Rehabilitation (Rehab or Treatment) is what comes next. Once your body is no longer in crisis, rehab is where you do the work to address the why behind the addiction. It’s a comprehensive process that combines different therapies to heal the mind and build the foundation for a new way of living. This stage is all about:
- Therapy: Digging into the root causes with individual and group counseling.
- Skill-Building: Learning healthy ways to cope with stress, triggers, and tough emotions.
- Psychiatric Care: Addressing co-occurring conditions like anxiety or depression that often fuel addiction.
Simply put, detox gets you through the fire of acute withdrawal. Rehab gives you the tools and blueprint to rebuild your life so you don’t have to go through that fire again.
Navigating withdrawal and recovery can feel overwhelming, but you don't have to do it alone. The compassionate, expert team at Altura Recovery is here to create a personalized outpatient treatment plan that fits your life. Learn more about our evidence-based programs and take the first step toward healing by visiting https://www.alturarecovery.com.