Substance abuse group therapy is a cornerstone of effective outpatient treatment, creating a space for shared experience, skill-building, and mutual accountability. For clinicians leading these sessions, selecting the right topics for group therapy substance abuse is critical to fostering engagement, addressing core recovery challenges, and facilitating lasting change. Meaningful group work hinges on more than just open discussion; it requires structured, evidence-based frameworks that meet clients where they are.
This comprehensive guide moves beyond generic prompts, offering a curated list of ten impactful topics designed for today's clinical settings. Each topic is broken down with actionable objectives, practical activities, and specific adaptations for different levels of care, including Intensive Outpatient (IOP), Partial Hospitalization (PHP), and supportive outpatient programs. For clinicians dedicated to making their group therapy sessions impactful and reaching a wider audience, understanding client acquisition strategies is vital. Explore a comprehensive digital marketing strategy for healthcare to connect with individuals who need your services most.
Whether you're working with clients managing co-occurring disorders, navigating family dynamics, or helping individuals reintegrate into daily life, these frameworks will help you structure sessions that empower clients on their journey. The following sections provide detailed outlines for sessions on relapse prevention, CBT and DBT skills, trauma-informed care, and more, all designed to facilitate real healing and sustained growth.
1. Relapse Prevention Planning
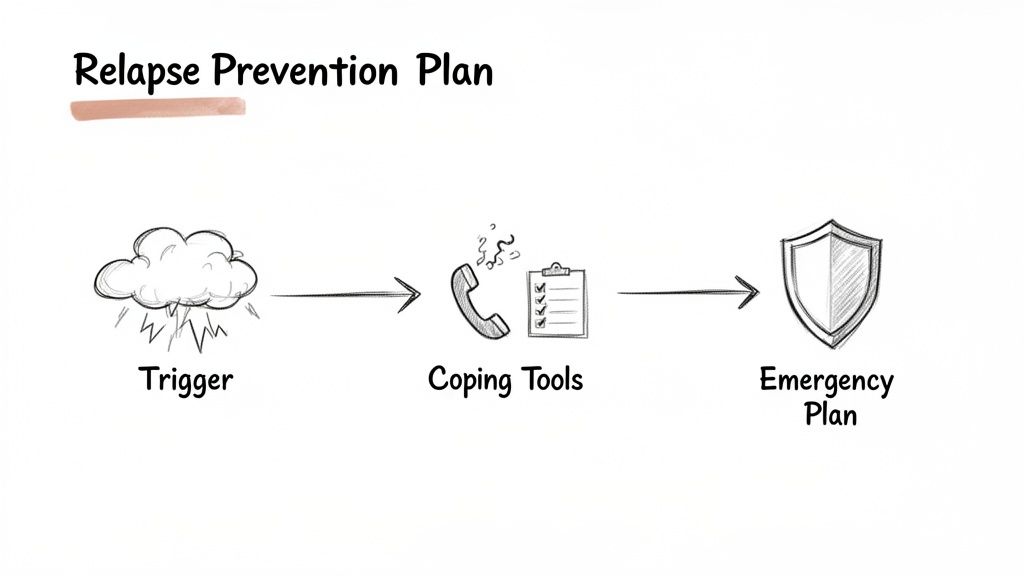
Relapse Prevention Planning is a cornerstone of effective substance abuse treatment. This topic focuses on equipping group members with the tangible skills to identify personal triggers, develop proactive coping strategies, and create a structured action plan for navigating high-risk situations. It moves beyond abstract concepts of avoiding relapse and into the practical, day-to-day work of maintaining sobriety.
This structured approach, popularized by Terence Gorski and the Marlatt & Gordon model, helps clients build a personalized recovery roadmap. It’s one of the most essential topics for group therapy substance abuse because it directly addresses the chronic nature of addiction and prepares individuals for life outside the structured treatment environment. The group setting is particularly powerful here, as members can share common triggers and brainstorm effective coping mechanisms together, reducing feelings of isolation.
Session Objectives
- Identify at least three personal high-risk situations (people, places, things, or feelings).
- Develop a written list of at least five healthy coping skills to use when triggered.
- Create a concrete emergency contact list and a step-by-step action plan for moments of intense craving.
Suggested Activities & Prompts
- Trigger Mapping: Have members draw a "trigger map" that visually connects specific people, places, and emotional states to their substance use. Discuss these maps in the group.
- Role-Playing Scenarios: Act out common high-risk situations, such as being offered a drink at a social event or running into a former using partner. Practice saying "no" and using exit strategies.
- Coping Skills Inventory: Use a worksheet where clients list their triggers and then write a specific, corresponding coping skill for each one (e.g., Trigger: feeling lonely; Coping Skill: call a support person).
Trauma-Informed & Co-Occurring Disorder Adaptations
For clients with co-occurring disorders like PTSD or anxiety, it's crucial to link relapse prevention to emotional regulation. The focus should be on how unmanaged symptoms can become primary triggers for substance use.
Key Adaptation: Instead of only asking, "What situations make you want to use?" reframe the question to, "What feelings, memories, or physical sensations from your trauma or anxiety feel unmanageable and lead to thoughts of using?" This connects the co-occurring disorder directly to the relapse cycle and validates their experience.
2. Cognitive Behavioral Therapy (CBT) Group Sessions
Cognitive Behavioral Therapy (CBT) group sessions are a fundamental component of modern substance abuse treatment. This topic centers on teaching clients to identify, challenge, and change the distorted thought patterns and core beliefs that fuel addictive behaviors. The core principle is that thoughts, not external events, directly influence feelings and actions. By changing these thoughts, clients can change their response to triggers and stressors.
Developed by pioneers like Aaron Beck, this evidence-based model provides a structured framework for understanding the cycle of addiction. It is one of the most vital topics for group therapy substance abuse because it gives clients a practical, life-long tool for self-regulation. The group dynamic is especially beneficial, as members can offer feedback on each other's thought distortions and collectively reinforce new, healthier ways of thinking, which normalizes the recovery process.
Session Objectives
- Identify the connection between specific thoughts, feelings, and substance-related behaviors (the "CBT Triangle").
- Recognize and name at least three common cognitive distortions (e.g., all-or-nothing thinking, catastrophizing).
- Practice using a thought record to challenge and reframe an automatic negative thought related to cravings or low self-worth.
Suggested Activities & Prompts
- Thought Record Worksheets: Use a structured worksheet where members identify a triggering situation, record their automatic thoughts and feelings, identify the cognitive distortion, and then develop a more balanced, alternative thought. When structuring your Cognitive Behavioral Therapy group sessions, it's beneficial to consult practical treatment plan examples for substance abuse and CBT to ensure comprehensive and effective intervention strategies.
- Cognitive Distortion "Charades": Write different cognitive distortions on slips of paper. Have a member pick one and act out a scenario exemplifying that thought pattern, while the group guesses the distortion and discusses it.
- Behavioral Experiments: Assign homework where clients test their negative predictions. For example, a client who thinks, "I can't have fun sober," is tasked with attending a social event and recording evidence that contradicts this belief.
Trauma-Informed & Co-Occurring Disorder Adaptations
For clients with co-occurring PTSD or anxiety, automatic negative thoughts are often deeply rooted in traumatic experiences. The goal is to connect these thoughts directly to their trauma history without forcing them to relive it.
Key Adaptation: Instead of a generic prompt like, "What negative thought are you having?" ask, "What is the story your trauma is telling you in this moment?" This phrasing validates that the thought is a symptom of a past event, not a current reality or personal failing. It separates the client from the thought, making it easier to observe and challenge.
3. Dialectical Behavior Therapy (DBT) Skills Training
Dialectical Behavior Therapy (DBT) Skills Training is a highly structured, evidence-based approach that equips clients with practical skills to manage overwhelming emotions and reduce impulsive, self-destructive behaviors like substance use. Developed by Marsha Linehan, DBT focuses on four core skill modules: Mindfulness, Distress Tolerance, Emotion Regulation, and Interpersonal Effectiveness. It operates on the core dialectic of balancing acceptance and change, helping clients accept their current reality while actively working to build a life worth living without substances.
The group format is central to DBT, providing a space for members to learn, practice, and receive feedback on new skills in a supportive environment. For individuals whose substance use is driven by emotional dysregulation, DBT offers a concrete alternative to using drugs or alcohol to cope with painful feelings. This makes it one of the most effective topics for group therapy substance abuse, especially for clients with co-occurring disorders.
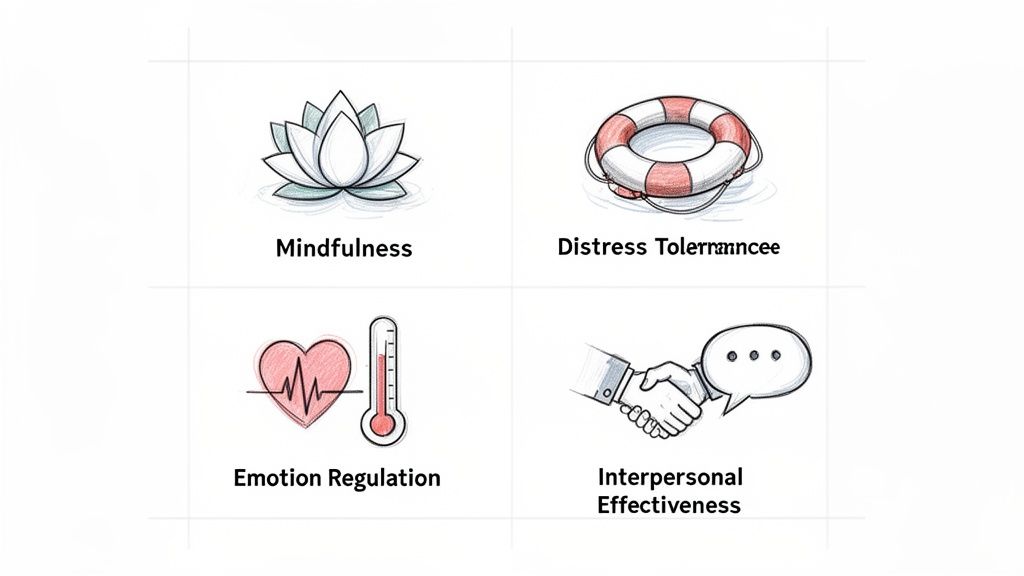
Session Objectives
- Identify and practice at least one skill from each of the four DBT modules.
- Complete a "diary card" to track urges, emotions, and skill use between sessions.
- Apply an interpersonal effectiveness skill (e.g., DEAR MAN) to a real-life relationship challenge.
Suggested Activities & Prompts
- Mindfulness Practice: Begin each group with a 5-minute mindfulness exercise, such as observing the breath or a "What" skill practice (observe, describe, participate).
- Distress Tolerance Skill Building: Use the "TIPP" skill (Temperature, Intense exercise, Paced breathing, Paired muscle relaxation) in session to demonstrate how to manage a crisis moment without resorting to substance use.
- Chain Analysis: Have a group member present a recent relapse or near-miss. As a group, complete a chain analysis worksheet to map the chain of events, identify vulnerabilities, and find points where a different skill could have been used.
Trauma-Informed & Co-Occurring Disorder Adaptations
DBT is inherently well-suited for clients with co-occurring disorders, particularly PTSD and BPD. The focus on distress tolerance is crucial for individuals who use substances to escape trauma-related flashbacks, memories, or overwhelming anxiety.
Key Adaptation: When teaching distress tolerance skills, explicitly link them to managing trauma symptoms. Frame skills like radical acceptance not as condoning past trauma, but as a tool to stop fighting reality and reduce the suffering that fuels substance use. Ask, "How can using the 'Self-Soothe' skill with your five senses help ground you when a flashback begins?" This directly connects DBT practice to trauma symptom management.
4. Family Systems and Communication Group Therapy
Family Systems and Communication Group Therapy explores the profound impact of substance use on family dynamics. This topic shifts the focus from the individual in isolation to the individual within a network of relationships, recognizing that addiction often develops and is sustained within a family context. It teaches members how family roles, communication patterns, and unwritten rules can either support or hinder recovery efforts.
Based on the foundational work of theorists like Murray Bowen and Salvador Minuchin, this approach helps clients understand how their substance use affects their family and vice versa. It is one of the most vital topics for group therapy substance abuse because long-term recovery is significantly strengthened when the home environment becomes a source of support rather than stress. The group provides a safe space to dissect these complex dynamics, learn new communication skills, and strategize for healthier interactions without the family being physically present.
Session Objectives
- Identify at least one dysfunctional family role (e.g., hero, scapegoat, lost child) they have played.
- Practice using "I" statements to express a personal need or boundary to a family member.
- Create a plan to establish or reinforce one healthy boundary with a specific family member.
Suggested Activities & Prompts
- Family Genogram Mapping: Clients create a simple family tree (genogram) to map patterns of addiction, communication styles, and major family events. They can then share insights about how these intergenerational patterns have influenced their own lives.
- Boundary Setting Role-Play: Set up scenarios where clients practice setting boundaries, such as saying no to a request for money from an enabling parent or asking a sibling not to bring alcohol to a family gathering.
- "I" Statement Practice: Provide a worksheet with prompts like "When you _____________, I feel _____________ because _____________. I need _____________." Group members complete and share their statements.
Trauma-Informed & Co-Occurring Disorder Adaptations
For clients with a history of family trauma or C-PTSD, discussions about family can be highly activating. The facilitator must create an environment of extreme safety and choice, emphasizing that members never have to share more than they are comfortable with.
Key Adaptation: Frame the discussion around chosen family and current support systems, not just the family of origin. Ask, "What does a 'healthy family' look like to you now, and who is in it? How can you practice these communication skills with the safe people currently in your life?" This empowers clients to build healthy new systems, especially if their family of origin remains unsafe.
5. Trauma-Informed Recovery Group
A Trauma-Informed Recovery Group acknowledges the profound and often direct link between traumatic experiences and substance use disorders. This topic shifts the therapeutic question from "What's wrong with you?" to "What happened to you?" It creates a safe, contained environment where members learn how trauma impacts the brain and nervous system, and how substance use frequently becomes a strategy to cope with overwhelming memories, emotions, or physical sensations.
This approach, guided by principles from SAMHSA and models like Seeking Safety, is one of the most vital topics for group therapy substance abuse because it addresses a root cause of addiction for a significant number of individuals. Instead of treating addiction in a vacuum, it integrates psychoeducation on trauma responses, grounding techniques for nervous system regulation, and skills for establishing safety. The group setting normalizes these experiences, helping members understand they are not alone in using substances to manage trauma symptoms.
Session Objectives
- Define trauma and identify at least two ways it has personally impacted substance use patterns.
- Practice at least three grounding techniques (e.g., 5-4-3-2-1 method, deep breathing) to manage distressing feelings in the moment.
- Develop a "safety plan" that includes safe people, places, and activities to turn to when feeling triggered or unsafe.
Suggested Activities & Prompts
- Psychoeducation Session: Use a whiteboard or handout to explain the "fight, flight, freeze" response and how chronic activation can lead to seeking substances for relief. Discuss how this shows up in members' lives.
- Grounding Skill Practice: Begin and end each session by leading the group through a grounding exercise. Ask members to rate their distress level before and after to demonstrate the technique's effectiveness.
- Safe Place Visualization: Guide members through a gentle, optional meditation to visualize a safe and peaceful place. Discuss what elements create a sense of safety and how they can access this feeling outside of the group.
Trauma-Informed & Co-Occurring Disorder Adaptations
By its nature, this topic is already adapted for co-occurring trauma. The key is ensuring the group does not become a trauma-processing group, which could be re-traumatizing without the proper clinical container. The focus must remain on the intersection of trauma symptoms and substance use.
Key Adaptation: Frame all discussions around skill-building for the present, not detailed processing of the past. Use prompts like, "When the memory of a past event comes up, what is a safe and sober coping skill you can use today?" This keeps the focus on present-day safety and recovery, which is the core principle of models like Seeking Safety.
6. Motivational Enhancement and Recovery Coaching Group
A Motivational Enhancement and Recovery Coaching Group is designed to build and sustain the internal drive necessary for lasting sobriety. This approach draws heavily from the principles of Motivational Interviewing (MI), focusing on resolving ambivalence and helping clients find their own compelling reasons to change. It shifts the dynamic from the therapist telling the client why they should be sober to the client discovering and articulating it for themselves.
This topic is essential for group therapy substance abuse because it meets clients wherever they are in their readiness for change, from pre-contemplation to action. Developed by William R. Miller and Stephen Rollnick, this collaborative style avoids confrontation and instead uses empathy and open-ended questions to foster a partnership. The group format amplifies this effect, as members witness peers navigating their own ambivalence, which normalizes their struggles and reinforces shared goals.
Session Objectives
- Articulate at least two personal reasons for pursuing sobriety that are linked to core values (e.g., family, career, health).
- Identify and verbalize one specific goal for the upcoming week related to behavioral change.
- Express a statement of commitment to change using their own words.
Suggested Activities & Prompts
- Decisional Balance Sheet: Members complete a four-quadrant worksheet listing the pros and cons of using substances and the pros and cons of staying sober. Discussing these in a group can reveal common themes and new perspectives.
- Values Card Sort: Provide a deck of cards with different values (e.g., "Honesty," "Family," "Security," "Adventure"). Ask clients to sort them into "Very Important," "Important," and "Not Important" piles and discuss how their substance use aligns or conflicts with their top values.
- Change Talk Elicitation: Use prompts like, "If you did decide to make a change, what might be the first step?" or "On a scale of 1-10, how important is it for you to change, and why didn't you pick a lower number?" to encourage clients to argue for their own change.
Trauma-Informed & Co-Occurring Disorder Adaptations
For clients with co-occurring disorders, motivation is often deeply intertwined with feelings of hopelessness or the belief that change is impossible due to their mental health symptoms. The focus must be on building self-efficacy and celebrating small, achievable steps.
Key Adaptation: Instead of focusing solely on the motivation to stop using, broaden the scope to include motivation for managing mental health. Ask, "What would it feel like to have more control over your anxiety?" or "How would your life be different if you felt less depressed?" This connects the desire for change to symptom relief, making sobriety a tool for mental wellness rather than just another demand.
7. Dual Diagnosis Support Group (Mental Health + Substance Use)
A Dual Diagnosis Support Group is a specialized forum for individuals managing both a substance use disorder and a co-occurring mental health condition like depression, bipolar disorder, or PTSD. This topic is designed to address the complex interplay between mental health symptoms and substance use, creating a space where clients can explore how each condition impacts the other. It moves beyond treating them as separate issues and focuses on an integrated recovery path.
This integrated approach, championed by organizations like SAMHSA, is vital because one disorder often exacerbates the other, creating a vicious cycle that can derail recovery if not addressed simultaneously. It’s one of the most critical topics for group therapy substance abuse because a high percentage of individuals with SUD also have a mental health diagnosis. The group setting normalizes this dual challenge, allowing members to share experiences with medication, symptom management, and integrated coping strategies without stigma.
Session Objectives
- Define "dual diagnosis" and identify how personal mental health symptoms and substance use cravings interact.
- Discuss the role of prescribed psychiatric medication in recovery and differentiate it from substance misuse.
- Develop at least three integrated coping strategies that address both mental health symptoms and substance use triggers simultaneously.
Suggested Activities & Prompts
- Symptom & Craving Timeline: Have members create a timeline that maps out significant mental health episodes alongside periods of heavy substance use. Discuss the connections and patterns observed.
- Medication Q&A: Facilitate a structured discussion (without giving medical advice) about members' experiences with psychiatric medications, including benefits, side effects, and the importance of communicating with their prescriber.
- Integrated Action Planning: Using a worksheet, ask clients to list a mental health symptom (e.g., panic attack) and a substance use trigger (e.g., social anxiety), then brainstorm one integrated action plan to manage both. For instance, an integrated strategy for Ambien dependence co-occurring with insomnia and anxiety might be a key focus. You can find more information about weaning off certain medications safely on our blog.
Trauma-Informed & Co-Occurring Disorder Adaptations
By its nature, this group is already adapted for co-occurring disorders. The key trauma-informed principle is to ensure the environment feels safe enough for clients to discuss psychiatric symptoms, hospitalizations, or medication challenges without judgment.
Key Adaptation: Frame the conversation around empowerment and self-advocacy. Instead of asking, "What's wrong with you?" ask, "What tools and supports help you manage your mental health and your recovery together?" This shifts the focus from pathology to proactive wellness and helps clients see themselves as capable managers of their integrated health.
8. Life Skills and Reintegration Group
A Life Skills and Reintegration Group focuses on building the practical competencies clients need to function successfully and independently in society. Active addiction often erodes fundamental abilities like financial management, time management, and job readiness. This topic directly addresses those deficits, preparing members to reintegrate into work, school, and community life with confidence and structure.
This approach, central to frameworks like the Community Reinforcement Approach (CRA) and SAMHSA life skills programs, is a critical component in holistic recovery. It helps bridge the gap between the supportive treatment environment and the demands of everyday life. The group setting is ideal for this topic, allowing members to collaboratively problem-solve real-world challenges, such as creating a budget or preparing for a job interview, which normalizes their struggles and builds shared motivation.
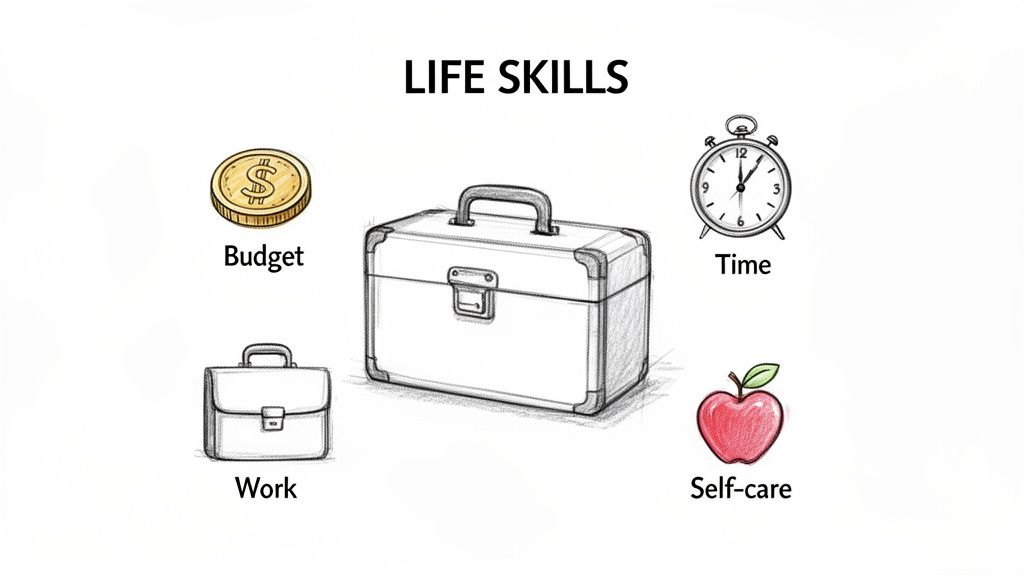
Session Objectives
- Create a simple, realistic weekly budget and identify one area for financial improvement.
- Develop a structured daily or weekly schedule that balances recovery activities, work/school, and self-care.
- Practice and demonstrate effective communication skills for a professional setting (e.g., a job interview).
Suggested Activities & Prompts
- Budgeting Workshop: Provide worksheets for members to track one week of spending. In the group, discuss spending habits, identify financial triggers, and create a basic budget together.
- Mock Interviews: Have members practice interviewing for a job with the group facilitator or a peer. Provide constructive feedback on communication, body language, and how to address gaps in employment history.
- Time Management Matrix: Use the Eisenhower Matrix (Urgent/Important) to help clients categorize their daily tasks. Discuss how prioritizing responsibilities can reduce stress and prevent overwhelm, which are common relapse triggers.
Trauma-Informed & Co-Occurring Disorder Adaptations
For clients with co-occurring disorders like depression or social anxiety, life skills can feel overwhelming and impossible. The focus must be on breaking tasks down into manageable, non-threatening steps and linking skill-building directly to symptom management.
Key Adaptation: Instead of asking, "Why can't you find a job?" reframe the prompt to, "What is one small step you can take this week toward employment that feels manageable with your current anxiety or energy levels?" This approach validates their challenges, promotes self-compassion, and builds momentum through small, achievable wins.
9. Mindfulness-Based Relapse Prevention (MBRP) Group
Mindfulness-Based Relapse Prevention (MBRP) integrates the practice of mindfulness with cognitive-behavioral relapse prevention strategies. This topic teaches group members how to increase their awareness of thoughts, cravings, and emotions without immediately reacting to them. Instead of trying to suppress or fight urges, participants learn to observe these internal experiences with curiosity and non-judgment, creating space between the trigger and a potential response.
Developed by Sarah Bowen and rooted in the work of Jon Kabat-Zinn, MBRP is one of the most transformative topics for group therapy substance abuse because it fundamentally changes a person's relationship with discomfort. It empowers individuals by showing them that urges are temporary, survivable sensations. The group dynamic is crucial for normalizing these experiences and collectively practicing a new, more mindful way of navigating the recovery journey.
Session Objectives
- Practice a 5-10 minute guided mindfulness meditation (e.g., body scan, mindful breathing).
- Define the concept of "urge surfing" and identify how it can be applied to a personal craving.
- Describe the difference between reacting to a thought and observing a thought without judgment.
Suggested Activities & Prompts
- Guided Urge Surfing: Lead the group in a guided meditation where they imagine a craving as a wave. Prompt them to notice its physical sensations, how it builds, crests, and eventually subsides on its own.
- Mindful Eating Exercise: Use a raisin or small piece of chocolate to guide members through a mindful eating exercise, focusing on sensory details. Connect this heightened awareness to noticing the early signs of a trigger or craving.
- Thought Labeling: Have participants practice silently labeling thoughts as they arise during meditation (e.g., "planning," "worrying," "judging"). This helps them detach from the content of the thoughts and see them as transient mental events.
Trauma-Informed & Co-Occurring Disorder Adaptations
For clients with PTSD, anxiety, or other trauma-related disorders, silent meditation can sometimes increase hypervigilance or intrusive thoughts. The focus must be on creating a sense of safety and choice during practice.
Key Adaptation: Offer multiple options for mindfulness practice. Instead of only a silent, eyes-closed meditation, provide alternatives like a walking meditation, gentle mindful stretching, or an eyes-open practice focused on an external object (e.g., a candle flame). Always remind clients they have permission to stop the exercise if they feel overwhelmed.
10. Peer Support and Accountability Group
A Peer Support and Accountability Group leverages the profound power of shared lived experience to foster connection, hope, and mutual responsibility. This topic shifts the focus from a purely clinical model to one of community and reciprocity, where members support each other in maintaining sobriety. It is built on the principle that those who have navigated the challenges of addiction are uniquely equipped to guide and understand others on the same path.
This approach, exemplified by organizations like Alcoholics Anonymous (AA) and SMART Recovery, is a vital component of a comprehensive treatment plan. It provides a crucial bridge from the structured environment of formal therapy to long-term, self-directed recovery in the community. As one of the most enduring topics for group therapy substance abuse, it addresses the deep-seated need for belonging and purpose that addiction often erodes, making it an indispensable element of sustained wellness.
Session Objectives
- Identify at least two individuals in the group or in a wider support network to contact for accountability.
- Articulate a personal recovery goal and share it with the group, asking for specific support.
- Practice active listening and offering non-judgmental encouragement to a peer sharing a struggle.
Suggested Activities & Prompts
- Check-In/Check-Out: Start and end each session with a structured check-in where members share a recent success, a current challenge, and what they need from the group.
- Milestone Celebrations: Dedicate time to acknowledge and celebrate recovery milestones (e.g., 30 days, 6 months, 1 year). Have the individual share what has worked for them.
- "Phone List" Exchange: Facilitate the creation and exchange of a voluntary contact list. Encourage members to practice reaching out to one another for support between sessions.
Trauma-Informed & Co-Occurring Disorder Adaptations
For individuals with social anxiety, PTSD, or a history of relational trauma, the concept of peer accountability can feel intimidating or unsafe. The group must be framed as a source of support, not judgment, with an emphasis on voluntary participation.
Key Adaptation: Instead of framing it as "accountability," which can imply scrutiny, use language like "mutual support" or "recovery allies." Ask, "Who in your life makes you feel safe and understood, and how can we help you build more of those connections?" This prioritizes psychological safety and empowers the client to define what supportive relationships look like for them.
10 Substance Abuse Group Therapy Topics Comparison
| Approach | 🔄 Complexity | ⚡ Resources & Time | ⭐ Expected Outcomes / 📊 Impact | 💡 Ideal Use Cases | Key Advantages |
|---|---|---|---|---|---|
| Relapse Prevention Planning | Moderate 🔄 (structured, iterative) | Low–Moderate ⚡ (facilitator, worksheets) | High ⭐ — improved relapse awareness; sustained coping 📊 | Step-down care; IOP/SOP clients balancing daily responsibilities 💡 | Concrete coping toolkit; peer accountability |
| Cognitive Behavioral Therapy (CBT) Group Sessions | Moderate 🔄 (structured curriculum, homework) | Moderate ⚡ (trained CBT clinician, materials) | High ⭐ — measurable cognitive/behavioral change 📊 | Dual-diagnosis; co-occurring mental health conditions 💡 | Evidence-based skills; improves emotional regulation |
| Dialectical Behavior Therapy (DBT) Skills Training | High 🔄🔄 (multi-module, individual+group) | High ⚡⚡ (specialized training, long duration) | Very high ⭐⭐ — reduces crises; better relationships 📊 | Emotional dysregulation, impulsivity; young adults 💡 | Comprehensive emotion & crisis management skills |
| Family Systems & Communication Group Therapy | High 🔄 (complex relational dynamics) | Moderate–High ⚡ (family involvement, skilled facilitator) | Moderate–High ⭐ — improved home stability and trust 📊 | Family-involved cases; rebuilding boundaries & support 💡 | Addresses relational root causes; strengthens support network |
| Trauma-Informed Recovery Group | High 🔄 (safety protocols; careful pacing) | High ⚡⚡ (trauma-trained clinicians, support infrastructure) | High ⭐ — reduced trauma symptoms; deeper healing 📊 | Clients with trauma history; EMDR integration; stabilized care 💡 | Targets root trauma; reduces shame and isolation |
| Motivational Enhancement & Recovery Coaching Group | Low–Moderate 🔄 (MI techniques; goal work) | Low–Moderate ⚡ (skilled facilitator, coaching tools) | Moderate–High ⭐ — increased motivation & engagement 📊 | Early recovery; ambivalence about change; readiness building 💡 | Builds intrinsic motivation; reduces defensiveness |
| Dual Diagnosis Support Group | High 🔄 (complex clinical coordination) | High ⚡⚡ (clinician expertise; psychiatric coordination) | High ⭐ — integrated symptom management; less cycling 📊 | Co-occurring SUD + psychiatric disorders; core specialty 💡 | Comprehensive integrated care; reduces stigma |
| Life Skills & Reintegration Group | Moderate 🔄 (broad practical curriculum) | Moderate ⚡ (guest speakers, varied expertise) | Moderate ⭐ — better daily functioning & employability 📊 | Young adults; working professionals transitioning from care 💡 | Practical competencies for reintegration; boosts self-efficacy |
| Mindfulness-Based Relapse Prevention (MBRP) Group | Moderate 🔄 (practice + relapse work) | Low–Moderate ⚡ (trained facilitator; practice materials) | High ⭐ — reduced cravings; improved regulation 📊 | Mindfulness-friendly clients; remote/virtual delivery 💡 | Teaches non-reactive coping; sustainable practice |
| Peer Support & Accountability Group | Low 🔄 (informal, peer-led) | Low ⚡ (minimal cost; volunteer facilitation) | Moderate ⭐ — increased belonging; sustained engagement 📊 | Step-down support; community connection; long-term recovery 💡 | Cost-effective, enduring community support |
Integrating Diverse Topics for Holistic Recovery
The journey to sustainable recovery from substance abuse is not linear, nor is it supported by a single, one-size-fits-all therapeutic approach. As this comprehensive guide illustrates, a truly effective group therapy program is a dynamic mosaic, carefully assembled from a diverse range of evidence-based topics. From the foundational logic of Cognitive Behavioral Therapy (CBT) to the emotional regulation skills of Dialectical Behavior Therapy (DBT), each topic serves as a vital tool in a clinician's toolkit, designed to address the multifaceted nature of addiction. The topics for group therapy substance abuse detailed here represent more than just a curriculum; they are pathways to self-discovery, healing, and lasting change.
By weaving together practical strategies like Relapse Prevention Planning with introspective work in Trauma-Informed Recovery groups, you create a holistic container for healing. This integrated model acknowledges that substance use is often a symptom of deeper, unresolved issues. It respects the individual's unique history, co-occurring mental health conditions, and personal motivations, ensuring that therapy is not just about stopping a behavior but about building a fulfilling life in its place.
Key Takeaways for Building an Effective Program
Mastering the facilitation of these diverse topics is crucial for any clinician dedicated to providing high-quality care. Here are the most important takeaways to remember:
- Integration is Power: No single topic exists in a vacuum. A client struggling with relapse triggers (Relapse Prevention) may benefit immensely from the distress tolerance skills learned in a DBT group or the self-compassion cultivated through Mindfulness-Based Relapse Prevention (MBRP). The most impactful programs intentionally create bridges between these concepts, helping clients see how different skills support a unified goal.
- Adaptability is Essential: The frameworks for IOP, PHP, and supportive outpatient delivery highlight the need for flexibility. A Life Skills group in a PHP setting might focus on foundational tasks like budgeting and meal planning, whereas the same group in an outpatient setting could address career development and healthy relationship building. Tailoring content to the specific level of care and client population is non-negotiable.
- Co-Occurring Disorders are the Norm: The inclusion of a dedicated Dual Diagnosis Support Group underscores a critical reality: addiction and mental health are deeply intertwined. Applying a trauma-informed lens and integrating mental health awareness across all group topics, not just specialized ones, is a best practice that fosters safety and promotes deeper healing.
- Action Creates Momentum: Therapy must extend beyond discussion. The most effective groups incorporate actionable activities, role-playing, and real-world assignments. Whether it's drafting a communication script in a Family Systems group or setting a tangible goal in a Motivational Enhancement session, these practical applications are what transform insight into tangible, real-world change.
From Theory to Practice: Your Next Steps
Moving forward, the challenge is not simply to "cover" these topics but to facilitate them with intention and skill. Clinicians should view this list as a blueprint for creating a responsive and comprehensive group therapy schedule. Start by assessing your current program: are there gaps? Could you better integrate trauma-informed principles or add a dedicated DBT skills component? Use the session objectives and activity prompts provided as a launchpad for developing your own unique, client-centered group modules.
Ultimately, facilitating powerful group therapy for substance abuse is about empowering individuals. It’s about giving them the language to understand their experiences, the skills to navigate their challenges, and the community to support their growth. By thoughtfully selecting and integrating these diverse topics for group therapy substance abuse, you provide a robust framework that honors the complexity of the human experience and equips each person with the tools they need not just to survive, but to build a life of meaning, connection, and real, lasting freedom.
At Altura Recovery, we understand that a successful recovery journey depends on a personalized and comprehensive therapeutic plan. Our outpatient programs in Houston are built on the very principles outlined in this guide, integrating a rich variety of group therapy topics to address the whole person. If you or a loved one is seeking a path to sobriety that is both structured and flexible, discover how Altura Recovery can help you build your foundation for lasting change.