Therapy for addiction isn't just about "talking through your problems." It's a structured, science-backed process for healing the brain, learning new ways to cope, and building a life where sobriety feels not just possible, but natural. It gives you the psychological tools to manage triggers, get to the root of the issue, and lay a resilient foundation for long-term recovery.
How Therapy for Addiction Builds a Foundation for Recovery
Think about what happens after a major physical injury, like a torn ACL. You wouldn't just sit around and talk about how much it hurts; you'd see a physical therapist. Their job is to guide you through specific, targeted exercises that rebuild strength, restore normal function, and prevent you from getting hurt again. You learn new ways to move and start trusting your body's ability to heal.
Addiction therapy works in a surprisingly similar way—it’s like physical therapy for your brain. Addiction literally rewires neural pathways, creating deeply ingrained habits and emotional reflexes. A good therapist acts as your guide, using proven methods to help you understand those pathways and start forging new, healthier ones.
Healing From the Inside Out
Effective therapy doesn't just put a bandage on substance use; it digs into the "why" behind it. Most people don't start using substances out of the blue. They turn to them to cope with underlying issues that feel too big or painful to face on their own.
Therapy creates a safe, completely confidential space to finally unpack these core drivers, which very often include:
- Unresolved Trauma: Past events can leave behind emotional wounds that substances seem to numb, at least for a little while.
- Co-Occurring Mental Health Conditions: Anxiety, depression, or PTSD are frequent travel companions to addiction, creating a vicious cycle where one condition makes the other worse.
- Chronic Stress: When you don't have healthy ways to manage life's pressures, substances can feel like the only release valve available.
- Family Dynamics: Sometimes, the relationship patterns and behaviors we learned growing up can unintentionally fuel an addictive cycle.
By getting to these root causes, you’re not just stopping a behavior. You are healing the very wounds that made the behavior feel necessary in the first place.
"Treating addiction without addressing its underlying causes is like trying to fix a cracked foundation with a fresh coat of paint. True recovery requires digging deeper to build a structure that can withstand life’s pressures."
Building Your Psychological Toolkit
One of the most powerful goals of addiction therapy is to arm you with a new set of skills—a toolkit for navigating life without needing to fall back on old habits. Instead of constantly reacting to cravings and triggers, you learn how to be proactive. This means developing real-world abilities to manage the thoughts, feelings, and situations that used to lead directly to using.
This focus on structured, evidence-based methods is exactly why therapy is a cornerstone of modern addiction treatment. The field is always moving forward, with incredible progress in modalities like cognitive behavioral therapy (CBT) and medication-assisted treatment (MAT) changing what's possible in recovery. For us at Altura Recovery, where we specialize in outpatient programs, this progress confirms what we see every day: offering these proven therapeutic interventions gives people the best possible shot at success. You can learn more about these addiction treatment market trends and see how they are shaping the future of recovery.
Exploring Evidence-Based Therapies That Work
Stepping into addiction therapy means you’ll find several powerful, science-backed approaches designed to help you heal. Instead of a one-size-fits-all solution, modern treatment is built on specific therapies that tackle different parts of addiction. Getting a handle on how these core methods work can demystify the process and empower you to dive deeper into your recovery.
These aren't just "talk therapy" sessions; they are structured, goal-oriented strategies for changing the way you think, feel, and behave. Each one offers a unique lens for understanding your experiences and a distinct set of tools for building a life free from substance use.
This map shows the foundational pillars that successful therapy helps to build: getting to the root causes, developing practical coping skills, and fostering genuine resilience.
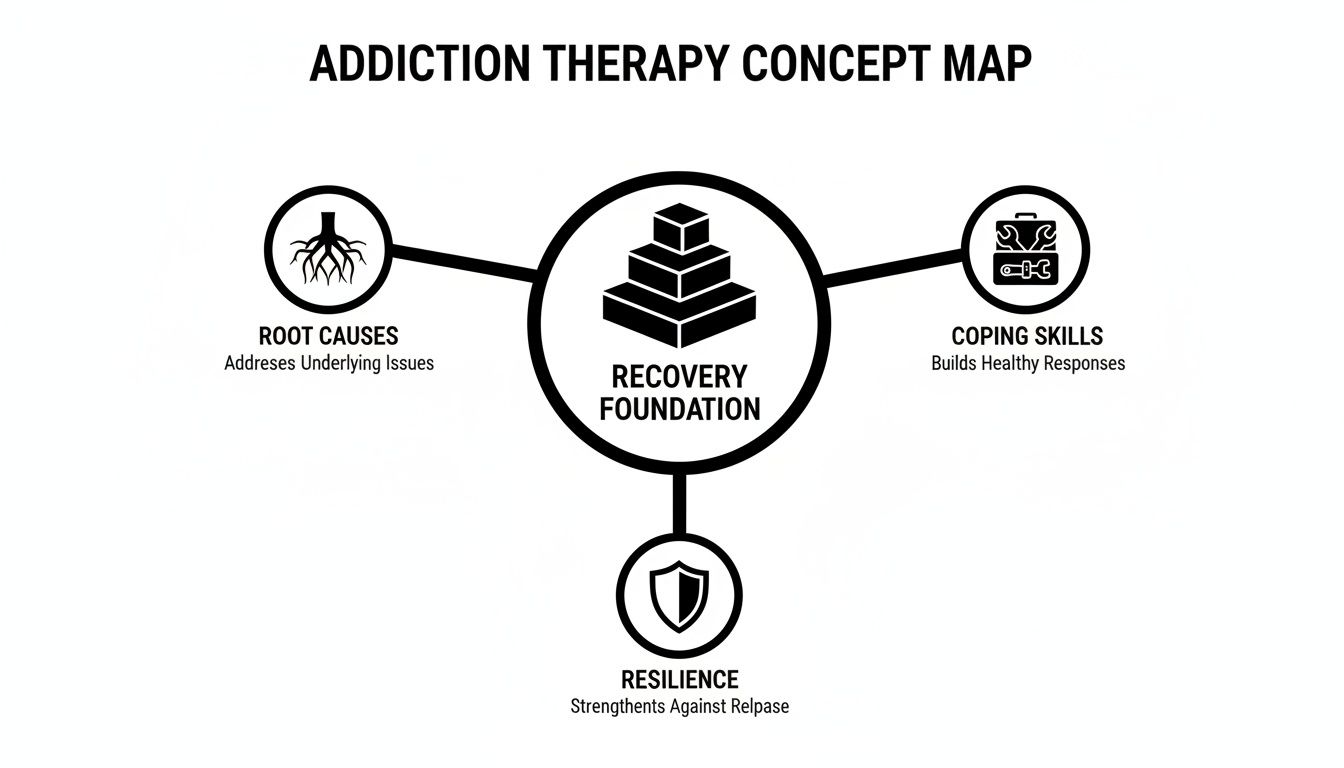
As you can see, effective therapy doesn’t just skim the surface by addressing substance use. It strengthens the core psychological structures you need for a recovery that actually lasts.
Cognitive Behavioral Therapy: Rewiring Your Thoughts
Cognitive Behavioral Therapy (CBT) is one of the most widely used and researched therapies for addiction, and for good reason. It’s built on a simple but powerful idea: our thoughts, feelings, and behaviors are all connected. Change your thinking, and you can change your actions.
Think of it like this: addiction carves automatic "highways" in your brain. A trigger appears—like stress from work—and your mind immediately speeds down the familiar path that leads to using. CBT helps you build new "roads." It teaches you to pause, identify the unhelpful thought ("I can't handle this without a drink"), challenge it, and intentionally choose a different, healthier response.
In a CBT session, you and your therapist will get practical. You'll work together to:
- Identify Triggers: Pinpoint the specific people, places, and feelings that spark cravings.
- Challenge Distorted Thinking: Learn to spot and reframe thoughts like "one time won't hurt" or "I've already failed, so I might as well keep going."
- Develop Coping Strategies: Practice actionable skills for managing stress, navigating social events, and dealing with cravings constructively.
This hands-on approach equips you with the mental tools to disrupt the cycle of addiction right where it starts—in your mind.
Dialectical Behavior Therapy: Building Your Emotional Toolkit
While CBT zeroes in on thoughts, Dialectical Behavior Therapy (DBT) places a greater emphasis on managing intense emotions. DBT was originally developed to treat borderline personality disorder, but its skills have proven incredibly effective for people whose substance use is driven by emotional turmoil.
Imagine trying to build a house with only a hammer. You wouldn't get very far. DBT provides a full toolkit for managing your emotional world, so you aren't stuck trying to solve every problem with the same blunt instrument. It gives you more options when you're faced with distress.
These four skill modules work together to create emotional balance:
- Mindfulness: Learning to stay present and observe your thoughts and feelings without judging them.
- Distress Tolerance: Getting through crisis situations without making them worse (like turning to substances).
- Emotion Regulation: Understanding your emotions and learning how to influence them when they aren't helping.
- Interpersonal Effectiveness: Building skills to communicate your needs, set boundaries, and navigate relationships in a healthy way.
DBT is a game-changer for anyone who feels overwhelmed by their emotions and has historically used substances to escape or numb out.
EMDR: Processing the Past to Heal the Present
So many people struggling with addiction are also carrying the weight of past trauma. Eye Movement Desensitization and Reprocessing (EMDR) is a specialized therapy designed to help the brain properly process and heal from these distressing memories.
Think of an unprocessed traumatic memory like a messy, disorganized file cluttering your mental desktop. Every time you accidentally click on it, the entire chaotic experience comes flooding back with the same intensity. EMDR acts like a powerful organizational tool that helps you properly file that memory away. It doesn't erase what happened, but it removes the intense emotional charge, so it no longer hijacks your present.
An analysis of cocaine use disorder treatment trials showed that a 75% reduction in use was associated with significant long-term improvements in psychosocial functioning, highlighting the value of therapies that address the deep-seated drivers of addiction.
During an EMDR session, a therapist guides you to focus on a traumatic memory while engaging in bilateral stimulation, like side-to-side eye movements. This process helps kickstart the brain’s natural information processing system, allowing the memory to be stored in a way that is no longer psychologically disruptive. For individuals whose substance use began as a way to cope with trauma, EMDR can be a crucial part of lasting recovery by finally healing the original wound.
Comparing Addiction Therapy Modalities
To help you see the differences at a glance, here’s a simple breakdown of CBT, DBT, and EMDR. While they all aim to support recovery, their focus and methods are distinct.
| Feature | Cognitive Behavioral Therapy (CBT) | Dialectical Behavior Therapy (DBT) | EMDR |
|---|---|---|---|
| Primary Focus | Identifying and changing unhelpful thought patterns and behaviors related to substance use. | Managing intense emotions, tolerating distress, and improving relationships to reduce the need for substance use. | Processing and healing from past traumatic memories that often fuel addiction. |
| Key Goal in Addiction | To break the cycle of thoughts-feelings-actions that leads to substance use. | To build a "life worth living" by equipping clients with skills to handle emotional pain without substances. | To reduce the emotional charge of traumatic memories so they no longer trigger cravings or self-medication. |
| What a Session Looks Like | Structured, often with homework. Focuses on specific situations, thoughts, and alternative responses. | A mix of individual therapy, group skills training, and phone coaching. Emphasis on practicing new skills. | A therapist guides the client through specific protocols involving bilateral stimulation (e.g., eye movements) to process memories. |
| Best For Individuals Who… | Struggle with automatic negative thoughts and want a practical, goal-oriented approach. | Experience intense emotional swings, self-harm, or use substances to escape overwhelming feelings. | Have a history of trauma (PTSD) and find that memories or flashbacks are a primary trigger for their substance use. |
Each of these therapies offers a proven path forward. The best one for you depends on your personal history, your primary struggles, and your recovery goals. At Altura, we help you figure that out.
How Therapy Fits into Outpatient Recovery Programs
It’s one thing to understand therapies like CBT or EMDR on their own, but seeing how they click together inside a structured recovery plan is where the real work—and real healing—begins. Outpatient programs are the engine that drives this process, using evidence-based therapy to help you recover while still connected to your daily life. It’s a powerful and practical alternative to residential treatment, especially for working professionals, students, or anyone with responsibilities at home.
Think of an outpatient program like a support scaffold around a building under construction. In the beginning, that scaffold is everywhere, providing maximum support when the structure is most vulnerable. But as the building gets stronger and can stand on its own, sections of the scaffold are gradually taken away. Outpatient care works exactly the same way, adapting to your progress step-by-step.
This flexible structure is key. It lets you start building real-world recovery skills from day one, applying what you learn in a therapy session directly to your life that same evening.
The Power of Different Levels of Care
Outpatient care isn't a one-size-fits-all solution. It's offered at different levels of intensity, creating a "step-down" process that matches support to your specific needs at every stage of the journey.
Partial Hospitalization Program (PHP): This is the most intensive level of outpatient care. You’ll typically attend therapy for several hours a day, five days a week, participating in a mix of individual and group sessions. PHP is a perfect fit for those transitioning from inpatient care or anyone who needs a high degree of support without 24/7 supervision.
Intensive Outpatient Program (IOP): The next step down is an IOP, which offers a robust schedule of therapy, usually for a few hours a day, several days a week. This structure is designed to integrate recovery into your work or school schedule, giving you the accountability and skills you need to navigate daily triggers.
Supportive Outpatient Program (SOP): As you build confidence and find your footing in recovery, you might transition to an SOP. This level involves less frequent sessions—often once or twice a week—focused on maintaining your progress, sharpening relapse prevention skills, and strengthening the foundation for long-term sobriety.
This tiered approach ensures that the therapy for addiction you receive is always aligned with where you are in your journey, never giving you too little support or holding you back when you’re ready to move forward.
Combining Individual and Group Therapy
The real magic of outpatient treatment comes from its dynamic blend of individual and group therapy. Each format plays a completely different—but equally critical—role in your recovery. Together, they create a comprehensive support system that addresses both your internal world and your connection to others.
Individual therapy is your personal strategy session. It's a confidential, one-on-one space to work with a therapist, dig into the root causes of your addiction, process trauma with modalities like EMDR, and fine-tune your treatment plan. This is where you do the deep, personalized work that is foundational to healing.
Group therapy transforms recovery from a solitary struggle into a shared journey. It provides a community of peers who genuinely understand what you’re going through, shattering the isolation that so often accompanies addiction.
In group sessions, you get to practice the skills you’re learning in a safe, supportive environment. You learn how to communicate your needs, set healthy boundaries, and get honest feedback from others who are walking the same path. That peer connection is invaluable, building a sense of belonging and accountability that can sustain you long after you complete the program.
Together, these two types of therapy create a powerful synergy, equipping you with both the personal insight and the community you need to thrive.
The Role of Family in Building Sustainable Recovery
Addiction is rarely a solo journey; its effects ripple outward, touching spouses, parents, children, and close friends. Think of it like a stone tossed into a pond—the splash might start in one spot, but the waves reach every shore. In the same way, substance use disrupts the entire family system, straining relationships and wearing down trust.
Because the family unit is so deeply affected, it also has to be a central part of the healing process.
Engaging loved ones in recovery isn't just a nice idea; it's a strategic part of building a foundation that will actually last. Recovery is a team sport. If only one player understands the new game plan while everyone else keeps running the old, dysfunctional plays, the odds of winning are slim. Family therapy gets everyone on the same page, learning new rules for communication, support, and healthy boundaries together.
This approach transforms the family from a potential source of stress and triggers into a powerful, unified support network. It creates an environment where sustainable recovery isn't just possible—it's actively encouraged by the people who matter most.
Rebuilding Trust and Improving Communication
Trust is almost always the first casualty of addiction. A long pattern of broken promises, secrecy, and unpredictable behavior leaves deep wounds that don't magically heal the moment someone walks into treatment. Family therapy provides a structured, safe space to start rebuilding that foundation, one brick at a time.
Guided by a clinician, family members learn to talk to each other in new, healthier ways. Instead of falling back into old patterns of blame, anger, or silent resentment, everyone is taught practical skills to express their feelings and needs constructively.
This process involves:
- Learning "I" Statements: This is a game-changer. Shifting from accusatory language like "You always…" to expressing personal feelings ("I feel hurt when…") fosters understanding instead of immediate defensiveness.
- Active Listening: We practice how to truly hear and validate what someone else is saying, even when it’s difficult or you don't agree.
- Setting Healthy Boundaries: This means establishing clear, respectful limits that protect everyone's well-being and support the recovery process itself.
These are the tools that allow a family to navigate conflicts, celebrate successes, and finally move forward as a cohesive unit.
Healing for the Whole Family
It’s crucial to understand that family therapy isn't just for the benefit of the person in recovery. Loved ones also carry their own trauma, anxiety, and exhaustion from living in the orbit of addiction. They often develop their own unhealthy coping mechanisms, like enabling behaviors or constant hypervigilance.
Family involvement in the treatment process can significantly improve outcomes, including higher rates of treatment engagement and longer periods of abstinence for the individual with a substance use disorder.
Family therapy offers loved ones a space to heal, too. It gives them permission to focus on their own well-being and equips them with tools to manage the immense stress that addiction has placed on their lives. By participating, they learn how to offer support without sacrificing their own mental health.
This transforms the dynamic completely. Instead of feeling like helpless bystanders, family members become active, empowered participants in their own healing journey. They learn to detach with love, offering support that is genuinely helpful rather than enabling. This shift is essential, as it stops the cycle of codependency and allows everyone in the family to grow stronger, both individually and together. At Altura Recovery, our family workshops are designed to foster this exact kind of mutual healing.
Finding the Right Addiction Therapist for You
Choosing a therapist is one of the most important decisions you'll make in your recovery. It’s less like hiring a professional and more like finding a trusted guide for a tough but rewarding expedition. The right person won’t just have the clinical skills—the map, so to speak—but will also be someone you feel you can genuinely trust and connect with.
That connection is what we call the therapeutic alliance, and it’s one of the single most reliable predictors of success in therapy. It's that feeling of being truly seen, understood, and supported without judgment. When you have that, you’re far more likely to lean into the process, do the hard work, and see real results.
What to Look for in an Addiction Therapist
Finding the right professional means looking beyond a gut feeling. You need to be sure they have the right background and approach to handle your specific situation. Here’s a practical checklist to help you narrow down the field:
- Credentials and Licensing: Look for licensed professionals like a Licensed Professional Counselor (LPC), Licensed Clinical Social Worker (LCSW), or a Licensed Psychologist (PhD or PsyD). These aren't just letters; they guarantee the person has met strict educational and ethical standards.
- Specialized Experience: Don't be afraid to ask directly about their experience with substance use disorders and any co-occurring issues you might have, like anxiety, depression, or trauma. A general therapist might not have the focused expertise you really need.
- Therapeutic Approach: Do they specialize in the evidence-based therapies we've talked about, like CBT, DBT, or EMDR? Their methods should feel like they could actually work for you.
Screening for these basics helps you build a strong shortlist, making the next step—the initial consultation—way more productive.
Essential Questions to Ask a Potential Therapist
Most therapists offer a short, free consultation call. This is your chance to interview them and see if the chemistry is there. Don't hold back; this is your recovery on the line.
The search for a therapist can feel overwhelming, especially when you realize how many people who need help struggle to find it. A massive treatment gap exists in the United States, where only about 23.6% of people who needed substance use treatment in the past year actually got it. Flexible, accessible programs are essential to closing this gap. You can discover more insights about these addiction statistics on TherapyRoute.com.
Use this call to ask direct questions that get to the heart of their philosophy and style. Try asking some of these:
- What’s your philosophy on addiction and recovery?
- How do you involve clients in creating their own treatment plans?
- What does a typical therapy session with you actually look like?
- How will we track progress toward my recovery goals?
- What’s your take on relapse? Do you see it as a failure or part of the process?
Their answers will tell you a lot about how they operate and whether their style fits with yours. Remember, you're looking for a partner in your recovery—someone who empowers you, challenges you, and has your back every step of the way.
Trust your intuition. The right therapist will make you feel hopeful and understood, even on that first call.
Taking Your First Step Toward Healing
The journey from understanding addiction to actually doing something about it is the most important one you'll ever take. All the information about different therapies and recovery programs boils down to a single, powerful moment of decision. That first step—picking up the phone, sending an email—can feel like the hardest part, but it’s also the exact moment your future begins to change.
Recognizing you need support is a sign of incredible strength, not weakness. At Altura Recovery, we’ve designed our entire process to honor that strength by making it as simple and stress-free as possible. There are no confusing hoops to jump through or judgmental conversations to fear. Your first call is just a confidential, compassionate chat about where you are and where you want to go.
Your Path Forward Is Clear
From that initial conversation, we map out a clear and manageable path forward. Taking action doesn't have to be overwhelming.
Here’s what you can expect when you reach out:
- A Confidential Assessment: We start with a conversation to understand your unique story, your struggles, and what you hope to achieve.
- A Personalized Plan: Based on that chat, we'll work with you to design a treatment plan that fits your life, using the evidence-based therapies that will work best for you.
- Flexible Scheduling: We immediately start coordinating care around your work, school, or family commitments, ensuring recovery supports your life instead of disrupting it.
"Recovery is not about becoming a new person, but about becoming the person you were always meant to be. The process of therapy is what helps you find your way back to that authentic self."
You’ve already done the hard work of exploring the solutions and considering a new path. The final piece is simply connecting with someone who can guide you the rest of the way. Therapy for addiction works, and a life of real healing, growth, and freedom is well within your reach.
Take control of your story today. Our team at Altura Recovery is ready to listen and help you build the foundation for a lasting recovery, one step at a time.
Common Questions About Addiction Therapy
Deciding to start therapy for addiction is a huge step, and it’s completely normal to have questions about how it all works. The road to recovery can feel a little confusing at first, but getting clear, honest answers helps build the confidence you need to move forward.
Let’s tackle some of the most common questions we hear from people just like you. Our goal is to give you the practical information you need to feel prepared for the journey ahead.
Can Outpatient Therapy Really Work for Severe Addiction?
Absolutely. Outpatient programs are often highly effective, even for someone dealing with a severe substance use disorder. The most important first step is a thorough clinical assessment to make sure it’s the right level of care for your specific situation.
For many people, intensive options like a Partial Hospitalization Program (PHP) or an Intensive Outpatient Program (IOP) provide the perfect blend of structure and real-world application. If you don’t need 24/7 medical supervision for detox and have a reasonably stable place to live, outpatient care is an excellent path. It lets you build coping skills in the very environment where you’ll use them, all while keeping up with work, school, or family.
What’s the Difference Between Individual and Group Therapy?
Think of individual and group therapy as two essential pillars holding up your recovery plan. Each one serves a unique and vital purpose.
Individual therapy is your private strategy session. It’s where you and your therapist work one-on-one, digging into the personal roots of your addiction, processing difficult emotions, and fine-tuning your treatment plan. This is where the personalized work happens.
Group therapy, on the other hand, is all about community and connection. It shatters the isolation that addiction thrives on, surrounds you with others who genuinely get it, and gives you a safe place to practice new communication skills. A strong recovery almost always involves a healthy mix of both.
Confidentiality is the bedrock of all therapy. Strict legal and ethical standards like HIPAA protect your privacy, creating a safe space where you can be completely open without fear of judgment.
How Long Does Addiction Therapy Usually Last?
There’s no magic number or universal timeline for addiction therapy. The length of your treatment is tailored entirely to you, depending on factors like the severity of the substance use and whether you're also working through co-occurring conditions like anxiety or depression.
While our outpatient programs have distinct phases, recovery is never a one-size-fits-all process. The real goal isn't to rush through a calendar; it's to build a rock-solid foundation for a lifetime of sobriety. We focus completely on your progress, ensuring you have the skills and confidence you need for a recovery that truly lasts.
At Altura Recovery, we believe asking questions is a sign of strength and a critical part of healing. If you’re ready to get answers and take the next step, our compassionate team is here to guide you. Learn how our flexible outpatient programs can support your unique path to recovery at https://www.alturarecovery.com.







