At the heart of it, the main difference between a Partial Hospitalization Program (PHP) and an Intensive Outpatient Program (IOP) boils down to time commitment and structure. Think of PHP as a highly structured, full-day program—almost like a 9-to-5 job focused entirely on your recovery. On the other hand, an IOP delivers robust, part-time therapeutic support, giving you more flexibility to manage life outside of treatment.
Deciding between them really depends on what you need right now. Are you looking for immersive, daily structure to build a strong foundation? Or do you need to balance intensive therapy with work, school, or family responsibilities?
Understanding The Continuum Of Care
Navigating the road to recovery means finding the right level of support at the right time. Both partial hospitalization and intensive outpatient programs are crucial stops on this journey, bridging the gap between 24/7 residential care and traditional weekly therapy. They offer structured, evidence-based treatment while allowing you to live at home, creating a vital support system without completely upending your life.
The rise of these programs marked a major shift in behavioral healthcare, providing effective alternatives to long, disruptive inpatient stays. Historically, the demand for more flexible and cost-effective treatment models fueled the growth of PHP and IOP. For example, between 1995 and 1997, Medicare payments to PHP providers more than doubled from $245 million to $550 million as the healthcare system began to fully embrace non-residential care.
Key Program Distinctions
Getting clear on the core differences between these programs is the first step in figuring out which one is the right fit. It’s not just about the number of hours spent in therapy; it’s about the clinical intensity and the type of person each program is designed to support. As you weigh your options, it's also helpful to start understanding the different roles of mental health professionals like therapists and psychiatrists who will make up your care team.
To give you a clearer picture, here’s a quick side-by-side look at the fundamental differences between PHP and IOP.
PHP vs IOP Quick Comparison Guide
This table offers a high-level summary of the fundamental differences between Partial Hospitalization (PHP) and Intensive Outpatient (IOP) programs, focusing on time commitment, structure, and ideal candidate profile.
| Feature | Partial Hospitalization Program (PHP) | Intensive Outpatient Program (IOP) |
|---|---|---|
| Weekly Time Commitment | 25-30 hours per week | 9-15 hours per week |
| Daily Schedule | 5-6 hours per day, 5 days a week | 3 hours per day, 3-5 days a week |
| Best For | Individuals needing daily structure, often as a step-down from inpatient care. | Individuals who need significant support but must balance work, school, or family. |
| Level of Autonomy | Moderate; highly structured daily routine. | High; integrates recovery into an existing daily life schedule. |
Ultimately, both PHP and IOP are designed to provide more support than traditional outpatient therapy but with more freedom than residential treatment. The choice depends entirely on your specific clinical needs and life circumstances at this moment.
A Detailed Comparison of Program Structures
When you’re looking at a Partial Hospitalization Program (PHP) versus an Intensive Outpatient Program (IOP), the biggest differences are in the daily grind—how your hours and days are structured. While both are a step down from 24/7 residential care, they’re built with very different levels of intensity and freedom in mind. Getting these structural nuances right is the key to picking the program that actually fits where you are in your recovery.
Think of a PHP as a full-time job focused on your recovery. It’s designed to give you an immersive, highly supportive environment during the day without the overnight stay. This makes it a perfect bridge for someone leaving an inpatient facility or for anyone whose symptoms are severe enough that they need daily clinical oversight to stay out of the hospital.
An IOP, on the other hand, is built to weave recovery into your current life. It delivers a strong therapeutic punch but on a part-time schedule, letting you keep up with work, school, or family responsibilities. This model works best for people who have a stable home life and have already built some foundational coping skills but still need more structure than once-a-week therapy can provide.
Weekly Time Commitment and Daily Schedule
The most obvious difference between PHP and IOP is the time you’ll spend in treatment each week. A Partial Hospitalization Program is, by its nature, far more demanding.
- PHP Commitment: You can expect to be in treatment for 5 to 6 hours per day, usually 5 days a week. That adds up to a substantial 25 to 30 hours of programming each week, creating a routine that puts your healing and stability front and center.
- IOP Commitment: An Intensive Outpatient Program is more manageable. Sessions typically run for 3 hours per day, 3 to 5 days a week. This brings the total to 9 to 15 hours weekly, a schedule built to help you manage recovery while juggling your other responsibilities.
This isn't just about scheduling; it shapes the entire rhythm of your life during treatment. A PHP schedule demands that you organize your life around the program, whereas an IOP schedule is designed to fit within your existing life.
A crucial distinction is that PHP often mirrors the structure of inpatient care during the day, providing a high level of containment and support. IOP, however, intentionally provides less structure to encourage you to practice recovery skills in real-world settings between sessions.
Therapeutic Modalities and Clinical Intensity
Both PHP and IOP use proven methods like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT). The real difference is in the depth, frequency, and application of these therapies.
In a PHP, you’ll have more frequent one-on-one sessions, a broader range of group therapies, and consistent check-ins with a psychiatrist. The longer days allow for a much deeper dive into complex issues. For example, a single day in a PHP might include a process group, a skills-based DBT group, an individual session with your therapist, and a meeting with a psychiatrist for medication management. This all-in-one daily structure provides immediate support and reinforces new skills on the spot.
In contrast, an IOP's shorter sessions are more targeted. A typical IOP day might consist of one or two group therapy sessions focused on specific topics, like relapse prevention or emotional regulation. Individual therapy and psychiatric services are still key, but they happen less often—maybe once a week—to supplement the group work. Many programs also weave in specialized approaches like trauma-informed therapy techniques to get at underlying issues, with the intensity adjusted to fit the program's structure.
Research backs both models, showing they lead to significant reductions in emergency room visits. Contemporary models describe PHP as providing 4–6 hours of structured treatment per day, 5–7 days per week. In contrast, IOP commonly delivers around 3–4 hours of therapy per day, 3–5 days per week, for a total of roughly 9–12 hours weekly. To see the full context, you can explore the research on outpatient program structures.
The Balance of Support and Autonomy
The final structural difference comes down to the balance between clinical support and personal freedom. A PHP is designed to build a "scaffolding" of support around you. The constant presence of clinical staff and peers creates a protective bubble where you can safely try out new behaviors and get immediate feedback. This high-touch support is vital for anyone who feels overwhelmed by daily triggers or is struggling to stay stable on their own.
An IOP, however, deliberately pushes you toward greater autonomy. With more time spent outside the treatment center, you're challenged to apply the skills you’re learning directly to your work, family, and social life in real time. This structure requires a higher degree of self-motivation and the ability to manage your time and stressors independently between sessions. It’s an environment that both tests and strengthens your recovery skills, setting you up for a successful transition to even less intensive care.
Determining the Right Fit for Your Needs
Choosing between a partial hospitalization program (PHP) and an intensive outpatient program (IOP) isn't about picking the "better" program. It's about honestly assessing which one fits your life and clinical needs right now. The right decision comes down to your symptom severity, your daily environment, and how much structure you need to make real progress.
Think of it this way: PHP is designed for someone who needs a level of care just a step down from residential treatment. It's a stabilizing force, creating a safe and structured container for most of the day.
IOP, on the other hand, is built for those who have a foothold in stability but need more support than a weekly therapy session can provide. The focus is on weaving recovery skills into your existing, functioning daily life.
The Ideal Candidate for a Partial Hospitalization Program
Let's imagine someone named Alex, who just finished a short inpatient stay for a severe depressive episode. While Alex no longer needs 24/7 monitoring, going home without significant daily support feels terrifying. The relapse risk is high, and the triggers of everyday life still feel too big to handle alone.
Alex is the perfect candidate for a PHP. Here’s why:
- Need for Structure: The program's full-day schedule (5-6 hours daily) gives Alex the routine and accountability needed to build a solid foundation in early recovery.
- High Symptom Acuity: Alex's symptoms, while better, still make daily functioning a struggle. The intensive clinical oversight in a PHP addresses these challenges in real-time.
- Step-Down from Inpatient Care: PHP is the ideal bridge, slowly reintroducing independence while keeping a high level of therapeutic support.
For anyone whose symptoms make it tough to keep up with work, school, or even basic self-care, PHP offers the necessary containment. It creates a therapeutic "bubble" that allows for deep healing without the stressors of an unstructured environment.
This decision tree helps visualize the core choice between a PHP and an IOP.
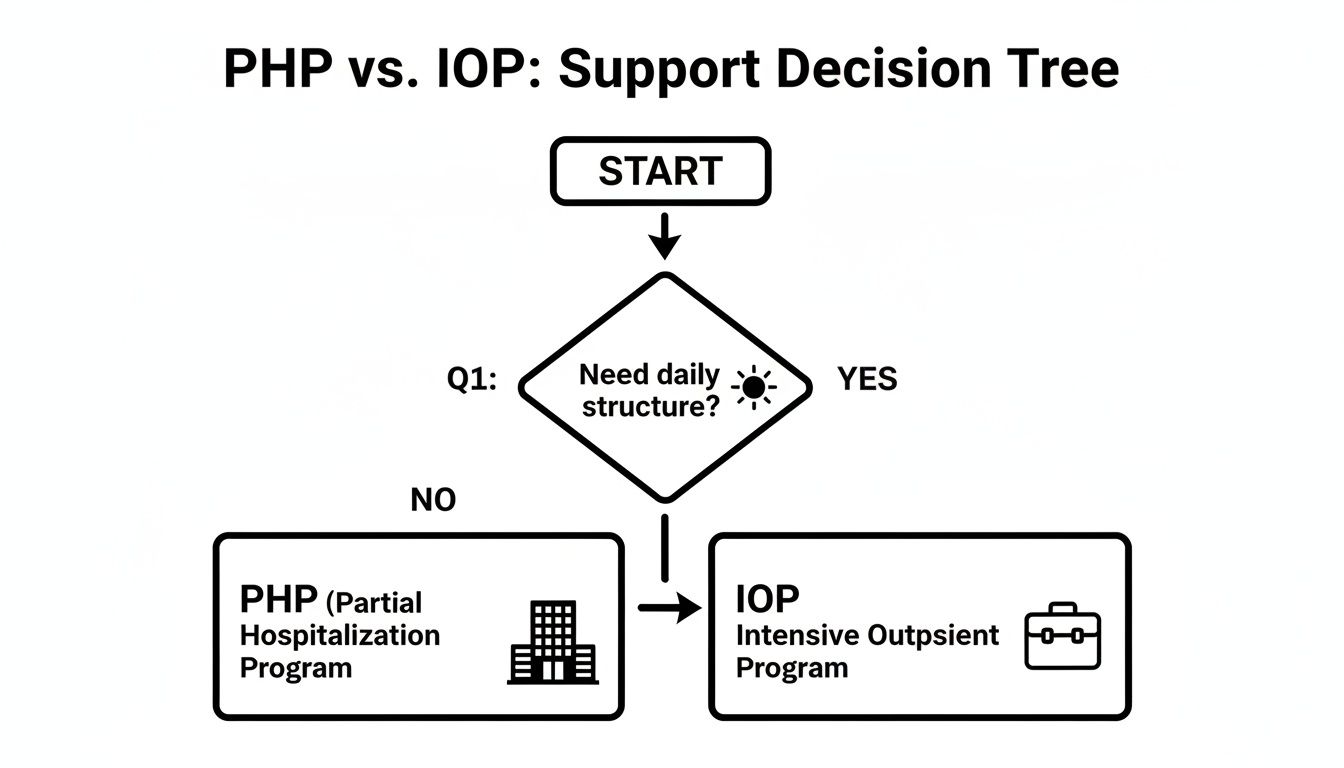
As you can see, the main question often boils down to whether you need daily, immersive structure or a more flexible, integrated approach to your care.
When an Intensive Outpatient Program Is the Right Choice
Now think about Sarah, a working professional and mother who has been managing her anxiety and substance use with a weekly therapist. She’s made progress but knows she needs a stronger set of tools to handle workplace stress and prevent relapse. She has a supportive family and a stable home life, but she can't step away from her job.
Sarah is a great fit for an IOP.
- Balancing Responsibilities: The IOP schedule (3 hours a day, 3-5 days a week) lets her attend treatment while still meeting her professional and family commitments.
- Applying Skills in Real-Time: Sarah can learn a new coping skill in her afternoon group session and practice it at home with her kids that very evening. This immediate application makes the learning stick.
- Established Foundational Stability: Unlike Alex, Sarah isn’t in an acute crisis. She has a baseline of stability and is ready to do the deeper work of recovery.
Both PHP and IOP are critical for meeting a huge need for accessible mental healthcare. In the United States, over 20% of adults had a mental illness in 2023, yet more than half of them aren't getting the treatment they need. Programs like PHP and IOP help close that gap by offering high-quality services that are more flexible and affordable than inpatient care. You can discover more about the expanding access to behavioral healthcare on Valant.io.
Ultimately, the best choice depends on an honest look at your needs. A consultation with a mental health professional can provide a clinical evaluation, helping you confidently choose the program that will best support your journey toward lasting wellness.
Navigating Insurance Coverage and Costs
Let's talk about the financial side of things—it’s a major source of stress for most people, but it doesn't have to be a mystery. The good news is that both Partial Hospitalization Programs (PHP) and Intensive Outpatient Programs (IOP) are considered essential behavioral healthcare services, so they’re typically covered by most major insurance plans.
The real key is understanding how your insurance provider decides which level of care they’ll approve.
Insurance companies operate on a standard called medical necessity. This just means they'll cover a program if a clinical assessment shows it’s the right level of care for your specific condition. Because PHP is much more intensive, it requires a higher level of medical necessity. In practice, this means showing that without this structured, daily support, a person would be at risk of needing to be hospitalized.
IOP coverage, on the other hand, is usually based on the need for a step-down from a higher level of care or a step-up from weekly therapy. It’s for folks who are stable enough to not need daily oversight but still require more support than a traditional therapist can provide to keep moving forward and prevent relapse.
Demystifying Insurance Terms
Trying to understand your benefits can feel like learning a whole new language. Before you can make a clear-headed decision when comparing partial hospitalization vs intensive outpatient options, you need to know what a few key terms actually mean for your wallet.
- Deductible: This is the amount you have to pay out-of-pocket for your healthcare before your insurance plan starts chipping in. If your deductible is $1,000, you’re responsible for the first $1,000 of covered services.
- Copay: This is a flat fee you pay for a specific service after you’ve met your deductible. For example, you might have a $40 copay for each day you attend the program.
- Out-of-Pocket Maximum: This is the absolute most you’ll have to pay for covered services in a plan year. Once you hit this number through your deductibles and copays, your insurance plan is supposed to pay 100% of any further covered costs.
A good admissions team, like the one here at Altura Recovery, can verify your specific benefits and lay all of this out for you in plain English so there are no surprises. They’ll also handle the pre-authorization with your insurance company, submitting the clinical documentation needed to get your care approved.
Because PHP involves more clinical hours each week, your daily copays and deductible costs can add up faster than in an IOP. Still, the total cost is almost always significantly less than an inpatient or residential stay.
Actionable Steps for Financial Clarity
You can make this whole financial process much less stressful by taking a proactive approach. Before you commit to any program, work with the admissions team to get straight answers.
Don't be afraid to ask specific questions like:
- Have you verified my in-network benefits for both PHP and IOP?
- Can you estimate what my daily copay will be for each program?
- How much of my deductible have I already met this year?
- What is my out-of-pocket maximum, and how close am I to reaching it?
By asking these direct questions and partnering with an experienced admissions team, you can get the financial clarity you need. That peace of mind allows you to focus on what really matters: your recovery.
The Critical Role of Aftercare in Long-Term Recovery
Finishing a Partial Hospitalization Program (PHP) or an Intensive Outpatient Program (IOP) is a massive accomplishment, but it's not the finish line. Think of it as a powerful first leg in a much longer race. Real, lasting recovery hinges on what comes next, which is why a solid aftercare plan isn’t just an add-on—it's one of the most vital parts of your treatment.
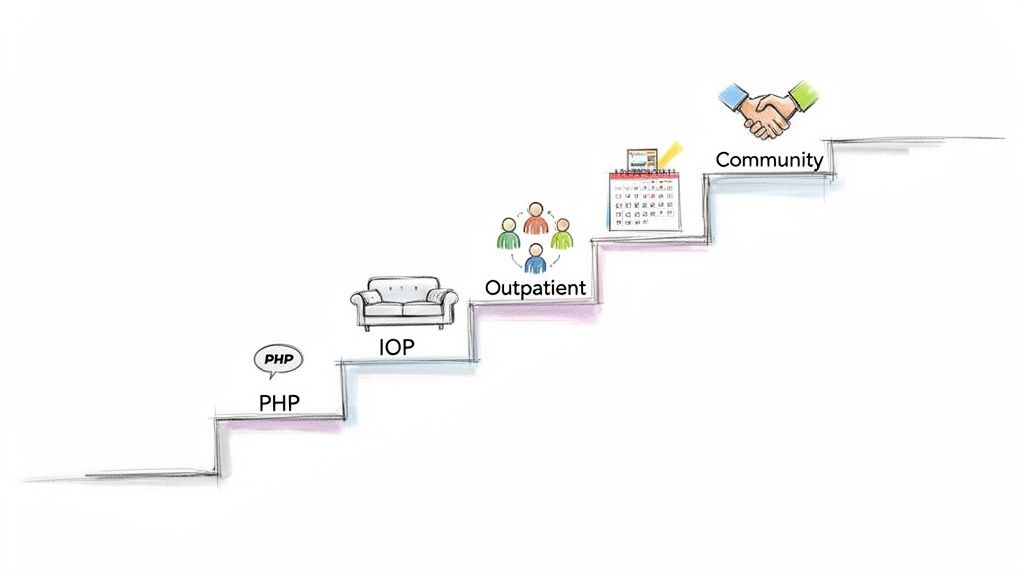
The goal was never just to get through a program; it's to build a foundation you can stand on for life. This is where the "step-down" process comes in. It’s a carefully mapped-out transition from high levels of clinical support to greater independence, making sure you’re never left scrambling without a safety net while navigating the real world.
The Step-Down Journey in Practice
A typical step-down path isn't just a theory; it shows how different levels of care link together to create sustainable change. It’s a gradual release of clinical structure, which is replaced by your own growing confidence and hard-won coping skills.
Here’s what that progression often looks like:
- From PHP to IOP: After graduating from a PHP, stepping down to an IOP is a common next move. The time commitment drops from 25-30 hours per week to 9-15 hours, freeing up your schedule to start applying recovery skills at work, school, or home.
- From IOP to Outpatient Therapy: Once you've found your footing and feel stable in the IOP, the next logical step is traditional outpatient care. This usually means weekly one-on-one therapy sessions and maybe some occasional group meetings to stay connected.
- Engaging with Community Support: The final phase is about fully weaving yourself into a personal support system. This is where you lean on regular support groups (like AA or SMART Recovery), continue any necessary medication management, and rely on your healthy network of family and friends.
This gradual handoff prevents the jarring shock of going from an immersive therapeutic environment straight back to an unstructured life—a transition that can be a huge trigger for relapse.
An effective treatment program doesn't spring aftercare on you during your last week. The conversation starts on day one, weaving relapse prevention and life skills into every single therapy session so you're prepared for the long haul.
Key Components of a Strong Aftercare Plan
A robust aftercare plan is more than a list of appointments. It’s your personalized roadmap for managing challenges and supporting your continued growth. A huge piece of this is knowing how to handle triggers before they lead you back to old patterns. You can get a head start by reading our guide on identifying and overcoming self-defeating behaviors.
A truly comprehensive plan always includes these core elements:
- Ongoing Therapy: Continuing individual sessions with a therapist to work through new challenges and keep your coping strategies sharp.
- Support Group Involvement: Actively showing up for peer support groups to maintain accountability and stay connected to others who get it.
- Medication Management: Regular check-ins with your psychiatrist to make sure any prescribed medications are still working effectively and are adjusted as needed.
- Healthy Support System: Intentionally nurturing relationships with supportive family and friends who understand your journey and genuinely cheer you on.
This commitment to what happens after the program is what separates a temporary fix from real, effective treatment. It’s the focus on building resilience that empowers you to not just recover, but to truly thrive for years to come.
How We Tailor PHP and IOP at Altura Recovery
Knowing the textbook difference between PHP and IOP is one thing. Seeing how a program is built to fit your life is another. At Altura Recovery, we don't just offer cookie-cutter programs; we design treatment that meets you where you are, recognizing that every recovery journey is unique. Our PHP and IOP are intentionally built with flexibility and your individual needs at the forefront.
Our whole philosophy is about providing the right level of care at precisely the right time. For someone needing significant daily support to get their footing, our Partial Hospitalization Program (PHP) provides that immersive, evidence-based structure. It's built to deliver the clinical intensity and routine that’s crucial for building a strong foundation, especially if you’re managing severe symptoms or stepping down from inpatient care.
Flexible and Focused Care
On the other hand, our Intensive Outpatient Program (IOP) is engineered for real-world integration. We know that recovery has to work within your life, not pull you completely out of it. That’s why we offer multiple schedules, including day and evening sessions. This makes it possible for working professionals, students, and parents to get the robust therapeutic support they need without having to press pause on their responsibilities. This flexibility is key—it lets you apply the coping skills you’re learning in real time.
At Altura Recovery, we specialize in treating dual-diagnosis and co-occurring disorders. Our clinical team is adept at creating integrated treatment plans that address both substance use and mental health conditions simultaneously, ensuring a more complete and sustainable recovery.
Advanced Therapies and Compassionate Guidance
What truly sets our programs apart is our use of advanced therapeutic methods. No two treatment plans look alike because we draw from a range of proven approaches like CBT, DBT, EMDR, and trauma-informed care. This lets us get to the root causes of addiction and mental health struggles, not just manage the symptoms. If you're curious about how we create a well-rounded path to wellness, you can learn more about the benefits of holistic therapy and how these practices complement our core clinical work.
Our experienced clinical team is with you every step of the way, offering compassionate, expert guidance. By blending deep clinical expertise with a genuine understanding of the recovery process, we help you build the resilience and skills needed for lasting change. This is how we take the concepts of PHP and IOP and turn them into real, tangible healing for every person who walks through our doors.
Common Questions About PHP and IOP
Even after comparing the programs side-by-side, you probably still have a few practical questions. That’s completely normal. Let's walk through some of the most common concerns people have when deciding on the right level of care.
Can I Still Work or Go to School?
This is often the first and most pressing question, and the answer gets right to the heart of how these programs differ in intensity.
-
Intensive Outpatient Program (IOP): Yes, absolutely. IOPs are specifically designed with this in mind. Sessions typically run for about three hours a day, three to five days a week, making it possible to schedule treatment around your existing work, school, or family commitments.
-
Partial Hospitalization Program (PHP): This is much harder, if not impossible. A PHP is a significant time commitment, requiring you to be onsite for five to six hours a day, five days a week. That full-day structure makes holding down a regular job or keeping up with a full academic course load extremely difficult.
How Do I Know if I Need More Support?
It’s not uncommon to start in an IOP and realize it isn't quite enough. Your clinical team will be tracking your progress closely, but there are clear signs that stepping up to a more structured program like a PHP might be the right move.
Key indicators that you might need a higher level of care include:
- Finding it hard to prevent relapse or manage cravings between your sessions.
- Noticing that mental health symptoms, like depression or anxiety, are getting worse.
- Struggling to use your new coping skills in your daily life without more direct support.
- Being in a home environment that feels unstable or unsupportive, making your recovery efforts feel undermined.
Realizing you need more help isn't a sign of failure—it's a sign of self-awareness and strength. The entire system of care is built to be flexible, allowing you to move between levels so you always have the right amount of support when you need it.
What Happens After I Finish the Program?
Graduating from a PHP or IOP is a huge accomplishment, but it’s a milestone, not the final destination. A quality treatment program won’t just discharge you; they’ll work with you to create a detailed aftercare plan well before your last day.
This transition plan is your roadmap for what comes next and usually involves:
- Stepping down to a less intensive level of care. This could mean moving from a PHP to an IOP, or from an IOP to weekly individual therapy sessions.
- Getting connected with community support networks like SMART Recovery or other peer-led groups that provide ongoing accountability and connection.
- Establishing care with a psychiatrist for continued medication management, if that’s part of your treatment.
The whole point of aftercare is to methodically transfer the structure and support you received in the program to a sustainable, personal support system you can rely on for the long haul.
At Altura Recovery, we know that choosing the right program is a critical first step. Our admissions team is here to listen, answer your questions, and help you navigate your options with the clarity and compassion you deserve. You can learn more about our personalized PHP and IOP programs on our site, or reach out to start your journey toward healing today.