Outpatient mental health programs are structured treatment options that let you live at home while getting serious, comprehensive care for mental health and substance use disorders. They offer a flexible but powerful alternative to residential treatment, weaving evidence-based therapy right into your daily life without forcing you to hit pause on your career or family responsibilities.
What Are Outpatient Mental Health Programs?
Figuring out the right path to mental wellness can feel a lot like planning a trip. Sometimes, you need an all-in, immersive retreat to reset—that’s similar to inpatient or residential treatment. But for many people, a different approach works better, one that provides robust support while keeping them plugged into their everyday lives. That’s the whole idea behind outpatient mental health programs.
Think of outpatient care as a spectrum of support, kind of like different levels of academic coaching. Someone might need intensive, daily tutoring to catch up (that’s like a Partial Hospitalization Program). Others do great with consistent weekly study groups (an Intensive Outpatient Program). And some just need a few check-ins to stay on track (a Supportive Outpatient Program). Each level is built to meet you exactly where you are.
Who Benefits Most from Outpatient Care?
This model isn't a one-size-fits-all fix, but it’s an incredibly good fit for a huge range of people. It creates a practical path to healing for anyone who needs more than a weekly therapy session but doesn’t require 24/7 supervision.
Here are a few common situations where outpatient programs are the perfect choice:
- Professionals and Students: People who need to keep up with their jobs, academic schedules, or family duties can fold treatment into their lives without having to step away completely.
- People Transitioning from Higher Levels of Care: For someone leaving a residential or inpatient facility, outpatient care is a critical "step-down." It acts as a structured bridge back to the real world, helping them solidify new coping skills in everyday settings.
- Those with a Strong Home Support System: If you have a stable, supportive living situation, outpatient treatment lets you lean on that network as a core part of your recovery.
- People with Co-Occurring Disorders: Many programs are experts at treating both mental health conditions (like anxiety or depression) and substance use disorders at the same time, offering integrated care that looks at the whole picture.
The main goal of any good outpatient program is to build a strong, sustainable foundation for recovery. By applying therapeutic skills directly to real-life challenges, you learn to manage triggers, build resilience, and create lasting change right inside your own community.
This approach means you get to practice what you learn in therapy almost immediately—whether that’s navigating a stressful work meeting, communicating better with family, or handling a tough social situation. The focus is squarely on practical application, making sure the skills you develop aren't just theories but become a natural part of how you live. Ultimately, outpatient care offers a path to healing that adapts to you, building independence and long-term wellness without putting your life on hold.
Navigating Different Levels of Care
Choosing an outpatient mental health program isn't about picking a single, generic option. It’s more about finding the right intensity of support for where you are right now in your recovery journey. Think of it like adjusting the difficulty on a video game—you need a level that’s challenging enough to push you forward but not so overwhelming that you get stuck.
The outpatient world is built on a "step-down" model, which allows you to move between different levels of care as your confidence and skills grow. This structure ensures you always have the right amount of clinical support. As you move through these stages, maintaining continuity of care is what makes the whole process work seamlessly.
This diagram shows how these levels are structured, from the most hands-on to the least.
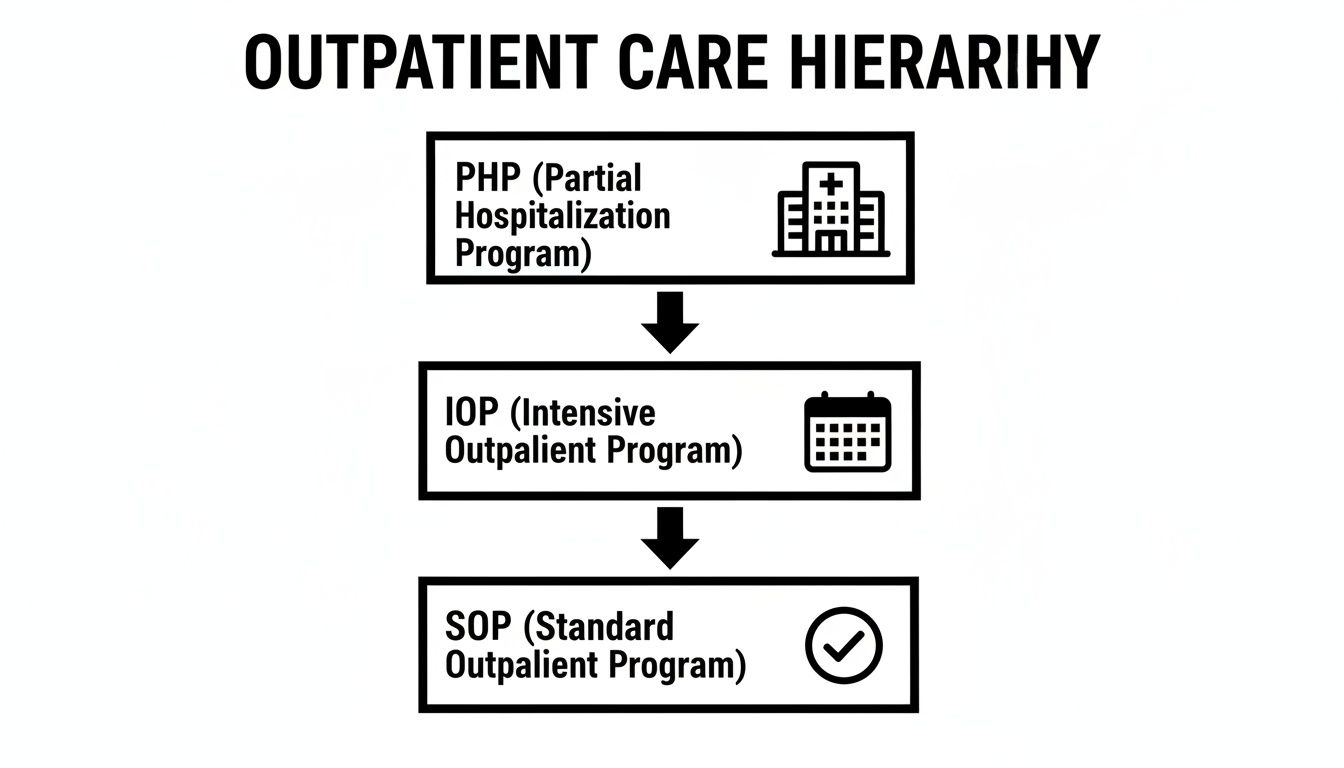
You can see the natural progression here. People often start with more structured support and then gradually "step down" into programs that encourage more independence.
Partial Hospitalization Programs (PHP)
The most structured and time-intensive option is the Partial Hospitalization Program (PHP). A PHP is designed for people who need daily medical and therapeutic oversight but have a stable enough home environment to return to each evening.
Imagine someone who just finished a 30-day residential program. They've made huge strides but aren't quite ready to face the world without serious daily backup. A PHP serves as that critical bridge, providing 5-6 hours of therapy and clinical services, 5 days a week. It’s the highest tier of outpatient care and a solid alternative to being fully hospitalized.
Intensive Outpatient Programs (IOP)
Next up is the Intensive Outpatient Program (IOP). This level strikes a powerful balance between structured treatment and personal freedom, making it one of the most common starting points for outpatient care.
An IOP usually involves 3-4 hours of treatment, 3-5 days per week. The schedule is built to fit around work, school, or family life. For instance, a working professional struggling with anxiety and substance use could join evening IOP sessions without having to quit their job. It delivers the "intensive" support required for real change while letting you practice new coping skills in your actual day-to-day life.
An IOP is like having a dedicated coaching staff for your mental health. You get consistent, focused training several times a week, building the strength and resilience you need to handle life's curveballs without needing round-the-clock supervision.
The structure of an IOP helps build accountability and a sense of community—two things that are absolutely vital for long-term recovery. This is especially important when you consider that nearly 50% of people with a dual diagnosis have both a substance use disorder and a mental health condition, highlighting the need for consistent, integrated support like an IOP provides.
Supportive Outpatient Programs (SOP)
The final step on this ladder is the Supportive Outpatient Program (SOP), sometimes just called standard outpatient care. This is the least time-intensive level, focusing squarely on maintaining progress and preventing relapse.
SOP sessions are much less frequent, often just 1-2 times per week for an hour or two. This stage is for people who have already built a strong foundation in a PHP or IOP and have shown they can use their new coping skills on their own.
Think of an SOP as the maintenance phase of recovery. It’s like graduating from intensive physical therapy to monthly check-ins with your trainer. The main goal is to reinforce the skills you've learned, troubleshoot any new challenges that pop up, and make sure your support network stays strong as you step into full independence. It’s this gradual transition that helps make long-term wellness stick.
The Core Components of Effective Treatment
Stepping into an outpatient mental health program can feel a bit like starting a new fitness plan with a team of expert trainers. You know the goal is to get stronger, but what do the workouts actually look like? The best programs don't rely on guesswork; they use a specific combination of evidence-based therapies and support systems, each designed to address a different part of your well-being.
These pieces all work together, much like a well-rounded exercise routine that blends strength training, cardio, and flexibility. The whole idea is to treat the whole person, not just a single symptom. This integrated approach ensures you build the mental and emotional muscles needed for lasting recovery.
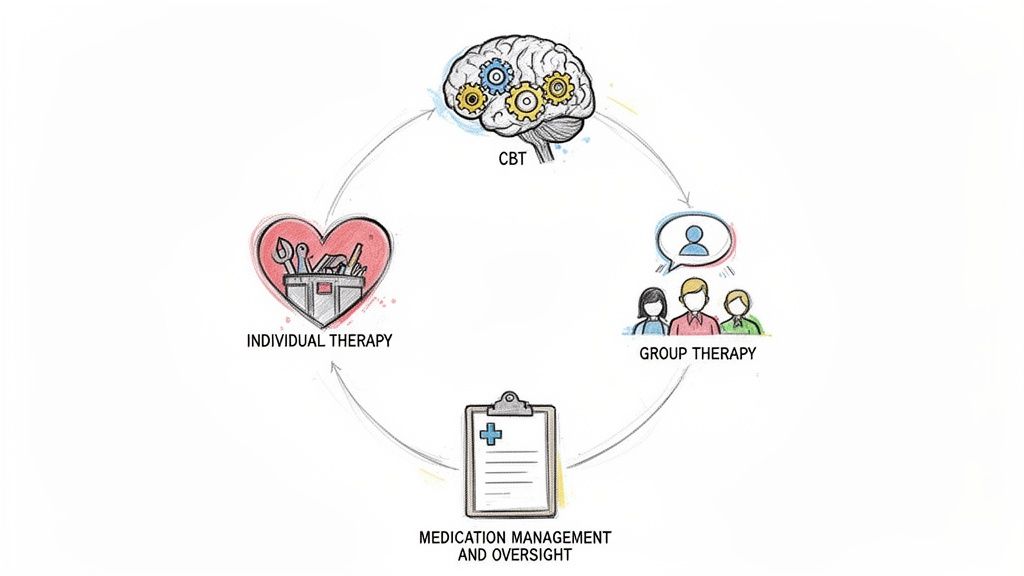
Foundational Therapeutic Modalities
At the heart of any quality outpatient program are specific therapeutic models that have been proven to work. Think of these as the core "playbooks" therapists use to help you understand your thoughts, manage your emotions, and change your behaviors.
Cognitive Behavioral Therapy (CBT): This is one of the most widely used therapies for a reason. CBT operates on a simple but powerful idea: your thoughts, feelings, and actions are all connected. By learning to identify and challenge negative or distorted thinking, you can change your behavior and improve how you feel. It's like becoming a detective of your own mind, spotting the unhelpful clues (thoughts) and replacing them with more accurate ones.
Dialectical Behavior Therapy (DBT): Originally developed for borderline personality disorder, DBT is now used for a wide range of conditions, especially for people who experience intense emotions. DBT teaches practical skills in four key areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. It’s like building a toolkit full of strategies to handle emotional crises without making things worse.
Eye Movement Desensitization and Reprocessing (EMDR): This is a specialized therapy designed to help people process traumatic memories. Using bilateral stimulation (like side-to-side eye movements), EMDR helps the brain reprocess and store traumatic memories so they lose their emotional intensity. The goal isn't to erase the memory, but to take away the distressing charge it holds.
Building a Comprehensive Support Structure
Beyond these core therapies, outpatient programs build a multi-layered support system around you. Each layer serves a unique purpose, from deep personal exploration to building a community of peers who get it.
Individual Therapy is your one-on-one time with a clinician. This is where you can dive deep into personal issues, set recovery goals, and work through challenges in a completely confidential space. It’s the cornerstone of your treatment plan, providing personalized guidance tailored just for you.
Group Therapy is where the magic of shared experience really comes alive. In these sessions, you connect with others facing similar struggles, which is incredibly powerful for reducing feelings of isolation and shame. Research shows just how effective group settings are; in fact, 79% of participants in some programs at risk for depression or anxiety recover after getting this kind of support. You can learn more about how groups foster healing by exploring different relapse prevention activities for groups.
Medication Management plays a critical role for many people. A psychiatrist or psychiatric nurse practitioner will evaluate whether medication could help stabilize your mood, reduce anxiety, or manage other symptoms. This piece is carefully integrated with your therapy to ensure your treatment is both balanced and effective.
An effective treatment plan is a living document, not a rigid prescription. It combines different therapeutic tools and support systems, adapting them as you progress on your journey toward wellness.
Family Therapy and Education are also crucial, because recovery doesn't happen in a vacuum. These sessions help repair relationships, improve communication, and teach loved ones how they can best support you. Healing your support system is often just as important as healing yourself.
A good treatment plan often takes a holistic approach, including strategies for overall well-being and methods for regulating stress and anxiety, which are fundamental to mental health. By combining all these core components, outpatient programs create a robust framework for real, sustainable change.
Integrated Care for Co-Occurring Disorders
Mental health struggles and substance use rarely stay in their own lanes. More often, they’re like two tangled roots of the same tree—intertwined, feeding into one another, and causing problems that look separate on the surface but are deeply connected underneath.
When someone is dealing with both a mental health condition (like anxiety or PTSD) and a substance use disorder at the same time, it’s called a co-occurring disorder, or sometimes a dual diagnosis.
Trying to treat just the substance use while ignoring the underlying depression is a recipe for relapse. It’s like pulling one weed but leaving the root system intact. This is exactly why modern, effective treatment programs use what’s known as integrated care—a strategy that addresses both conditions simultaneously.
Why an Integrated Approach Is Essential
Think about someone who drinks to quiet their social anxiety. If a treatment program only focuses on stopping the drinking, the core anxiety is left untreated, creating a powerful, ever-present trigger to pick up a drink again. On the flip side, if therapy only tackles the anxiety without addressing the alcohol use, the person continues to lean on an unhealthy coping mechanism that gets in the way of real healing.
Integrated care is designed to break this frustrating cycle. It starts from the understanding that both conditions influence each other, weaving them into a single, cohesive treatment plan.
An integrated care model means that clinicians from both mental health and substance use disciplines are on the same team, working together. They create one comprehensive plan where every therapy session, group discussion, and medication decision is made for the whole person, not just one set of symptoms.
This approach isn’t just a good idea; it’s critical. Nearly 50% of people with a substance use disorder also have a co-occurring mental health diagnosis. Any program that isn’t equipped to handle this complexity is missing half the picture.
How Outpatient Programs Treat Dual Diagnosis
Outpatient programs are perfectly set up to offer this kind of sophisticated, integrated care while still allowing people to stay connected to their lives. The industry reflects this reality: outpatient counseling has grown to account for 48.5% of the behavioral healthcare market revenue in 2025. This model gives clients a realistic way to manage recovery while still going to work, caring for family, and sleeping in their own bed. You can dig deeper into these market trends in the full behavioral health market report.
Here’s how outpatient programs specifically adapt their core services to treat co-occurring disorders:
- Adapted Therapies: Core therapies like CBT and DBT are customized to address both issues at once. A CBT session, for example, might help a client connect anxious thoughts to alcohol cravings and then build new, healthier responses to manage both.
- Specialized Group Therapy: Group sessions are often built around dual diagnosis topics. This creates a powerful space where people can share their struggles with others who truly get the unique challenge of managing a mental health condition while also staying sober.
- Psychiatric Oversight: Medication management is even more crucial here. A psychiatrist can prescribe medications that effectively treat mental health symptoms without interfering with sobriety or posing a risk for dependency.
- Unified Clinical Team: Therapists, case managers, and medical staff all work in close collaboration. This ensures everyone is on the same page, providing consistent support that reinforces both mental wellness and recovery.
By weaving these elements together, outpatient programs provide the nuanced, comprehensive support needed to finally untangle the roots of co-occurring disorders and build a solid foundation for a recovery that lasts.
How to Choose the Right Program for You
Deciding to get help is the hardest part. Now comes the practical step: finding an outpatient mental health program that actually fits you. This part shouldn't add more stress; it should feel like you're finally finding a trusted guide for a tough journey. The key is knowing what to ask and what to look for beyond the polished website.
Think of it like hiring a personal trainer. You wouldn't just pick the closest gym. You'd ask about their certifications, their specific training style, and whether their approach actually matches your fitness goals. The same thinking applies here. You need to be sure the clinical team and the environment are the right match for what you're going through.
Verifying Program Legitimacy and Expertise
Before you get into the details, start with the basics. Your first move should be to confirm the program is properly licensed and its staff are qualified. This is the non-negotiable foundation for safe and effective care.
- Licensing and Accreditation: Is the facility licensed by the state? Is it accredited by a reputable body like The Joint Commission or CARF? These seals of approval are a clear sign that they meet high standards for quality and safety.
- Staff Credentials: Ask about the team's qualifications. Are the therapists licensed professionals (like an LCSW, LPC, or LMFT)? Do they have a psychiatrist or psychiatric nurse practitioner on staff to handle medication? A strong program has a team with a diverse range of expertise.
- Specialization: Does the program have real experience with your specific challenges? If you're dealing with trauma, you'll want to know if they offer therapies like EMDR. If you have a co-occurring disorder, ask them to explain their integrated treatment model.
Aligning Treatment with Your Personal Needs
Once you've confirmed a program's credibility, you can zero in on how their approach will work for you personally. This is where you dig into the types of therapy they offer and their overall philosophy of care. It's so important to find a place where you feel seen, heard, and respected.
Choosing a program isn't just about finding good treatment; it's about finding the right treatment for you. The best clinical model in the world won't be effective if you don't feel a connection to the people and the process.
Look at the therapies they use. Do they lean on evidence-based practices like CBT or DBT? Do they encourage family involvement? A good program will be completely transparent about their methods and how they adapt them for each person.
Navigating Logistics: Insurance and Scheduling
Finally, it's time to tackle the practical details that make treatment possible. Insurance and scheduling can feel overwhelming, but a quality program will have administrative staff ready to help you sort it all out.
Understanding your insurance coverage is a critical first step. Most programs will verify your benefits for you, clearly explaining what's covered and what your out-of-pocket costs might look like. Don't be afraid to ask for a detailed breakdown of all expenses so there are no surprises later.
Scheduling flexibility is another huge factor. Many outpatient mental health programs offer both day and evening sessions, plus virtual options, to fit around work, school, or family life. This adaptability is becoming more and more common as the demand for accessible care grows. The U.S. behavioral health market, which was valued at USD 96.9 billion in 2025, is expected to reach USD 159.35 billion by 2035, a jump largely driven by the rise of telehealth. You can find more details on these trends in the latest behavioral health industry report.
Finding the right fit requires looking at a program from all angles—clinical, personal, and logistical. Taking the time to ask these questions upfront will help you choose a program with confidence and set yourself up for a successful recovery journey. The following table provides a checklist to guide your conversations with potential providers.
Key Questions to Ask When Choosing a Program
Use this checklist to evaluate and compare different outpatient mental health programs to find the best fit for your needs.
| Category | Question to Ask | Why It Matters |
|---|---|---|
| Credentials & Safety | Is the facility licensed by the state and accredited by The Joint Commission or CARF? | Accreditation ensures the program meets national standards for safety, quality, and patient care. |
| Clinical Team | What are the credentials of your therapists, psychiatrists, and other clinical staff? | You want a team of licensed, experienced professionals who specialize in the areas you need help with. |
| Treatment Approach | What evidence-based therapies (e.g., CBT, DBT, EMDR) do you use? | Evidence-based practices are scientifically validated to be effective for specific conditions. |
| Personalization | How is my treatment plan developed and customized for me? | A one-size-fits-all approach rarely works. Your plan should be tailored to your unique history, symptoms, and goals. |
| Co-Occurring Disorders | How do you treat co-occurring disorders like anxiety and substance use simultaneously? | Integrated care that addresses both issues at once has far better outcomes than treating them separately. |
| Family Involvement | What opportunities are there for my family to be involved in my treatment? | Family support is often a critical component of lasting recovery, and their involvement can help heal relationships. |
| Scheduling & Format | Do you offer morning, evening, or virtual sessions to fit my schedule? | Flexibility makes it possible to get the help you need without having to put your entire life on hold. |
| Insurance & Cost | Can you verify my insurance benefits and provide a clear breakdown of all out-of-pocket costs? | Financial transparency prevents unexpected stress and helps you plan for the investment in your health. |
| Aftercare & Support | What kind of aftercare planning or alumni support do you provide after I complete the program? | Recovery is an ongoing process. A good program will help you create a plan to maintain your progress long-term. |
By asking these pointed questions, you move from being a passive patient to an active partner in your own care. This diligence ensures you find a program that not only has the right credentials but also feels like the right place for you to heal and grow.
Common Questions About Outpatient Programs
Deciding to get help is a huge step, but the "what comes next?" part can feel overwhelming. It’s completely normal to have questions. In fact, uncertainty is one of the biggest reasons people hesitate to start treatment.
This section is designed to clear up that uncertainty with straightforward answers to the most common questions we hear about outpatient mental health programs. Our goal is to demystify the process, tackle the practical concerns, and help you feel confident about moving forward.
We’ll walk through what a typical day looks like, how treatment can actually fit into your life, and how your family can be a part of the healing process.
What Does a Typical Day in an Outpatient Program Look Like?
While every program has its own unique rhythm, a day in a Partial Hospitalization Program (PHP) or Intensive Outpatient Program (IOP) is anything but unstructured. It’s a carefully planned schedule of therapeutic activities designed to build skills, create connection, and help you heal.
Think of it like this: you might arrive in the morning and start with a group check-in, where everyone shares their goals and immediate challenges for the day. From there, you could move into a process group focused on a specific topic, like managing triggers or learning to communicate more effectively.
After a short break, you might join a skills-based session, like a Dialectical Behavior Therapy (DBT) group where you learn and practice mindfulness or distress tolerance techniques. The day is a dynamic mix of different formats—individual therapy, meetings with a psychiatrist for medication management, or even specialized sessions like art therapy or a relapse prevention workshop. It's an immersive experience that packs a lot of healing into a few focused hours.
How Can I Balance Treatment with Work or Family?
This is probably the single biggest—and most valid—concern people have. It’s also the very reason outpatient mental health programs were created. Their flexibility is their greatest strength, allowing you to weave recovery into your life instead of putting your life on hold for recovery.
Here’s how that balance works in the real world:
- Flexible Scheduling: Many programs offer both daytime and evening IOP sessions. This means a working professional can attend therapy after their workday is done, or a parent can get treatment while their kids are at school.
- Real-World Application: The skills you learn in therapy aren’t theoretical; they’re meant for immediate use. Had a tough conversation with your boss? You can process it in your group session that same evening and get real-time feedback and support.
- A Step-Down Approach: You won’t be in an intensive program forever. You might start with an IOP that requires several hours a week, but as you build stability and confidence, you’ll transition to a supportive outpatient program (SOP) with a much smaller time commitment.
The core idea is that healing shouldn't require you to sacrifice everything else. Outpatient care is built on the principle that you can be a dedicated employee, a present parent, or a committed student while also being a person actively working on your mental wellness.
Are Virtual Programs as Effective as In-Person Treatment?
The rise of telehealth has been a game-changer for mental health, making high-quality care more accessible than ever before. For many people, virtual or hybrid outpatient programs are just as effective as traditional in-person services. The right fit really just depends on your specific needs and situation.
Virtual IOPs offer the same evidence-based therapies—like CBT, DBT, and group sessions—but deliver them through a secure video platform. This format knocks down huge barriers like transportation and can be a lifeline for people living in remote areas or those with mobility challenges. The most important thing is that the program is run by skilled facilitators who know how to create a strong sense of community and connection, even through a screen.
That said, for individuals who need more hands-on support, don’t have a private, quiet space at home, or are at a higher risk, in-person treatment might be a better choice. The best programs often offer both, empowering you to choose the format that makes you feel most comfortable and supported.
How Can My Family and Loved Ones Get Involved?
Recovery is rarely a solo journey; it’s a team sport. Your support system plays a huge role, and the best outpatient programs don’t just acknowledge this—they actively include family and loved ones in the process. This involvement is critical for healing strained relationships and building a strong foundation for long-term success.
Most high-quality programs will offer a few different ways for family to participate:
- Family Therapy Sessions: Led by a clinician, these sessions provide a safe space to improve communication, work through conflicts, and rebuild trust. It’s a chance for everyone to learn a new, healthier way of relating to one another.
- Educational Workshops: Many programs host workshops or family nights to educate loved ones about mental health, addiction, and the recovery process. This helps them understand what you’re going through and learn how to be a more effective source of support.
- Coordinated Care: With your permission, your therapist can keep your family in the loop, making sure everyone is on the same page about your treatment goals and progress.
This collaborative approach helps turn the home environment into a place that actively supports your recovery, rather than getting in the way of it.
The need for this kind of accessible, flexible care has never been greater. Globally, over 1 billion people are living with mental health conditions. Yet despite this staggering number, fewer than 7% of individuals with mental health or substance use disorders receive treatment that is considered effective. You can learn more about these global mental health statistics from the World Health Organization. This reality highlights just how vital outpatient models are for closing the treatment gap and reaching people where they are.
At Altura Recovery, we know these questions are just the beginning. Our team is here to provide the answers and support you need to move forward with confidence. If you're ready to explore how our flexible outpatient programs can fit into your life, visit us at https://www.alturarecovery.com to learn more.