When you’re trying to treat mental health and substance abuse, you can’t just focus on one and hope the other gets better on its own. They’re almost always deeply intertwined. The most effective path forward is an integrated approach—often called dual diagnosis care—that addresses both conditions at the same time. This isn't about treating separate symptoms; it's about treating the whole person to build a foundation for real, lasting healing.
The Link Between Mental Health and Substance Use
Mental health conditions and substance use disorders rarely happen in a vacuum. More often than not, they are two sides of the same coin, a clinical reality known as co-occurring disorders. Trying to treat one without the other is like trying to save a sick tree by only watering one root while letting the other wither.
Think of it like that tree. It has two main roots tangled tightly together just beneath the surface. One root might be a mental health condition like anxiety, depression, or PTSD. The other is a substance use disorder. These roots don't just coexist; they feed each other, creating a cycle that can feel impossible to escape. True wellness only happens when you nourish both roots at once.
Understanding the Cycle of Co-Occurring Disorders
The connection between mental health and substance use is powerful and self-reinforcing. For many people, substance use starts as a way to self-medicate the painful symptoms of an undiagnosed or untreated mental health condition. It might offer a fleeting sense of relief, but it almost always makes the underlying problem worse over time.
This plays out in a few common pairings:
- Anxiety and Alcohol: Someone with crippling social anxiety might find that a few drinks make it easier to be around people. Soon enough, their brain starts depending on alcohol to manage that anxiety, leading to an alcohol use disorder and even more intense "rebound" anxiety when they aren't drinking.
- Depression and Opioids: The emotional numbness from opioids can feel like a welcome escape from the crushing weight of depression. This pattern can quickly spiral into dependency, while the substance itself disrupts brain chemistry and drags the depression even deeper.
- Trauma (PTSD) and Stimulants: A person haunted by intrusive memories and hypervigilance from PTSD might turn to stimulants to feel a sense of control or to simply stay awake and alert. But these substances often ramp up anxiety and paranoia, pouring fuel on the fire of their PTSD symptoms.
This creates a vicious cycle where each condition makes the other worse. The substance use intensifies mental health symptoms, and those worsening symptoms drive a stronger urge to use the substance.
Addressing co-occurring disorders isn't about picking which problem is "worse." It's about recognizing that both are part of a single, complex challenge. Real recovery requires a treatment plan that can skillfully untangle these intertwined roots.
This is exactly why integrated mental health and substance abuse treatment is so critical. Instead of sending someone to one clinic for therapy and another for addiction counseling, this model brings all the necessary care under one roof. It offers a coordinated, evidence-based strategy that honors your entire experience and provides the clearest path to genuine healing.
Why Integrated Outpatient Programs Work
In the past, treatment for mental health and substance use was often kept in separate boxes. This forced people to jump between two different systems, trying to piece together their own recovery. It’s like sending a car with a tricky engine problem to two different shops—one for the electrical system, one for the fuel injectors. They might fix their individual parts, but the engine still won't run right because no one looked at how everything works together.
Integrated outpatient programs completely change that dynamic by treating the whole person, all under one roof.
This unified approach delivers intensive, evidence-based care without making you put your entire life on hold. For countless professionals, students, and parents, residential treatment just isn't a realistic option. Outpatient levels of care, like Partial Hospitalization (PHP) and Intensive Outpatient (IOP), offer a powerful alternative. They give you the structure and support you need while letting you stay connected to your life—a practical path forward for mental health and substance abuse treatment.
Recovery in Real Time
Picture an integrated outpatient program as a supportive co-pilot for your life. When you first start, they’re right there with you, helping you manage the controls as you fly through the turbulence of early recovery. As you get stronger and more confident, they gradually hand over more of the responsibility, but they never leave your side.
The key difference? You’re not learning to fly in a simulator. You're learning in the real world, facing your daily challenges with an expert right there to guide you.
This real-time application is what makes outpatient care so powerful. Instead of being insulated inside a residential facility, you get to immediately test out your new coping skills in the very environments that used to trigger you. You learn how to navigate a stressful workday, manage complicated family dynamics, and handle social events without falling back on old habits.
The goal of integrated outpatient treatment isn't just to get you sober in a clinical setting. It’s to help you build a resilient, sober life right inside your own community, surrounded by your own support system.
This approach turns recovery from an abstract idea into a lived, daily reality. You’re weaving a foundation for lasting change directly into the fabric of your life, making it stronger and far more sustainable.
Bridging a Critical Gap in Care
The need for this kind of effective, accessible treatment is staggering. One sobering global study found that only 6.9% of people with mental health or substance use disorders ever receive effective care. The road to recovery is filled with roadblocks; while many people know they need help, very few actually get the quality of care that leads to real change.
Integrated outpatient programs are designed to bridge that gap. A core component of the best programs is adopting approaches like trauma-informed care principles to create a truly safe healing environment. This ensures every part of the program is built on safety, trust, and empowerment—addressing the deep wounds that so often fuel co-occurring disorders.
This model delivers clear advantages that lead to better outcomes:
- Flexibility for Real Life: With day, evening, and virtual sessions, you can get help without having to sacrifice your job, school, or family commitments.
- Immediate Skill Application: You can put the coping strategies you learn in therapy to use in real-world situations that very same day, which reinforces learning and builds genuine confidence.
- Building a Local Support Network: You connect with peers right in your own community, creating a sober support system that will be there for you long after you complete the program.
- Reduced Stigma: By integrating treatment into your daily routine, the whole process of seeking help feels more normal, which helps reduce feelings of shame and isolation.
Choosing the Right Level of Outpatient Care
When you’re looking into mental health and substance abuse treatment, the jargon can be overwhelming. What on earth are PHP, IOP, and SOP? Getting a handle on these different levels of care is the first real step toward finding support that actually fits your life.
I find it helps to think of recovery not as a single, giant leap but as a staircase. Each level of care is a solid step designed to move you toward lasting independence, ensuring you get the right intensity of support at exactly the right time. This approach builds a stable foundation before you move on, guiding you from intensive clinical support back to a confident, self-directed life. The goal is simple: match the program to your needs, so you're never overwhelmed or left wanting more.
This visual shows how an integrated care model creates that structured path from intensive treatment back to a fulfilling daily life.
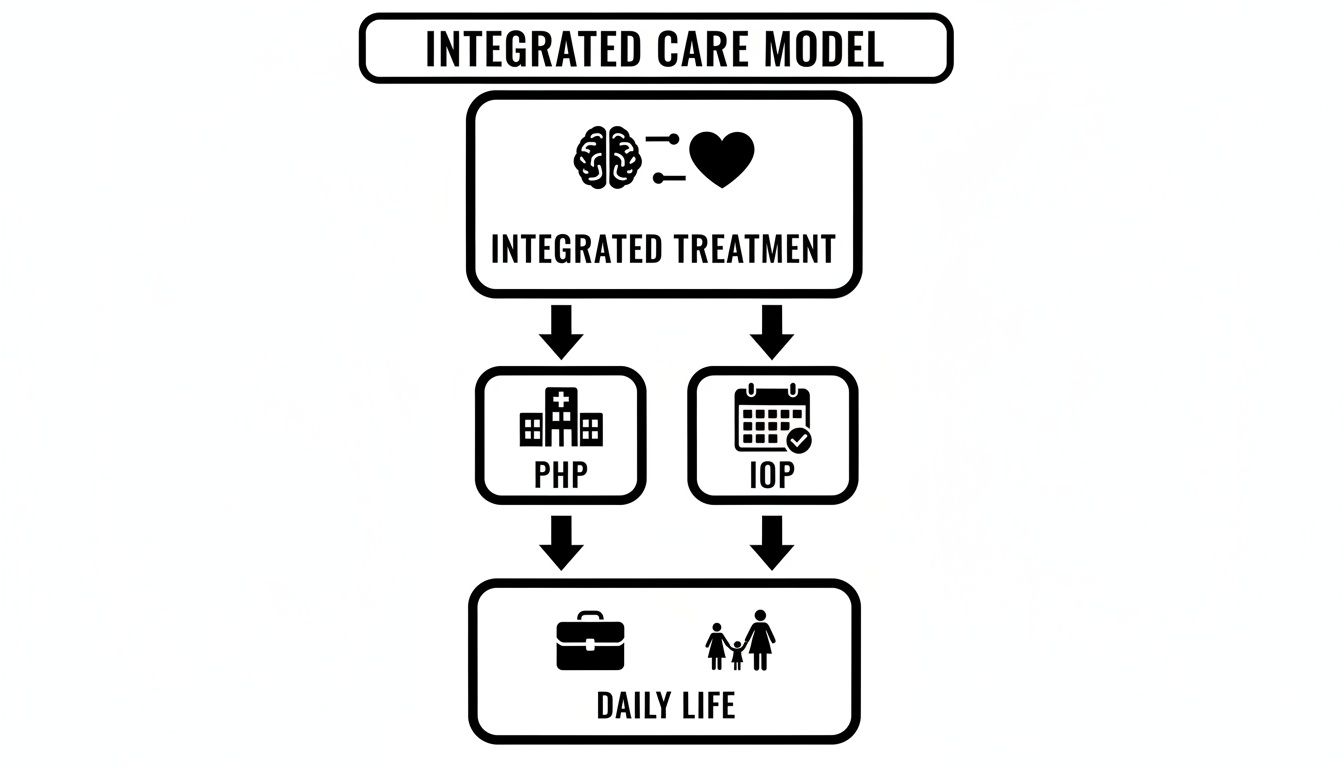
As you can see, stepping down from more structured programs like PHP and IOP gives you more autonomy to manage your career, family, and personal growth on your own terms.
The Foundational First Step: Partial Hospitalization Program (PHP)
The Partial Hospitalization Program (PHP) is the most intensive level of outpatient care—the strong, sturdy base of the staircase. It’s built for individuals who need significant clinical support but are stable enough to live at home or in a sober living environment. Think of PHP as a bridge, perfect for those transitioning out of residential treatment or for whom standard weekly therapy just isn't cutting it.
In a PHP, you’ll typically spend 5-6 hours a day, 5 days a week, immersed in therapeutic activities. This high level of engagement provides the structure and accountability so crucial in early recovery. A typical day often includes:
- Individual Therapy: One-on-one time to dig into personal challenges and set treatment goals.
- Group Therapy: Clinician-led groups covering topics like relapse prevention, emotional regulation, and communication skills.
- Psychiatric Care: Regular check-ins with a psychiatrist for medication management and evaluation.
- Holistic Modalities: Activities like mindfulness, art therapy, or yoga to support your overall well-being.
PHP is the ground floor of your recovery. It gives you the maximum support needed to stabilize, develop core coping skills, and build a strong sober network before you take the next step.
Gaining Autonomy: Intensive Outpatient Programs (IOP)
Once you’ve built a solid foundation in PHP—or if your needs are less acute from the get-go—the next step up is the Intensive Outpatient Program (IOP). This level represents a deliberate move toward greater independence. While you still get robust clinical support, an IOP requires a smaller time commitment, allowing you to reintegrate more fully into work, school, or family life.
IOP is where you start road-testing the skills you’ve learned in a more independent setting. It’s about using your new tools in the real world while still having a strong clinical safety net to catch you.
An IOP usually involves 3-4 hours of therapy, 3-5 days per week. The flexible scheduling, often with day and evening options, makes it a great choice for working professionals or parents. You’ll continue with individual and group therapy, but with more time to apply your recovery principles in your daily life—a critical phase for building genuine confidence and resilience.
Maintaining Progress: Supportive Outpatient Programs (SOP)
The final step on the staircase is the Supportive Outpatient Program (SOP), often called aftercare. This is the top landing. You have the most freedom here, but you still benefit from consistent, ongoing support to keep you on track. SOP is designed for people who have successfully completed a higher level of care and are confidently managing their recovery.
An SOP acts as a vital connection to your clinical team and sober community, making it a powerful tool for long-term relapse prevention. This level of care typically involves:
- Attending group therapy once or twice a week.
- Continuing individual therapy on a bi-weekly or monthly basis.
- Participating in alumni groups and community events.
This ongoing connection ensures you never feel alone on your journey. It provides a dedicated space to process challenges, celebrate successes, and stay accountable as you build a fulfilling, meaningful life in recovery. Each step on this staircase is designed to empower you, moving you closer to real, sustainable freedom.
To make these levels even clearer, here's a side-by-side comparison.
Comparing Outpatient Treatment Levels
This table breaks down the key differences between PHP, IOP, and SOP to help you see where you or a loved one might fit best.
| Program Level | Time Commitment | Clinical Intensity | Best For |
|---|---|---|---|
| Partial Hospitalization (PHP) | 25-30 hours/week | High | Individuals needing daily structure and intensive therapy without 24/7 residential care. Ideal for stepping down from inpatient or for those needing more than standard outpatient. |
| Intensive Outpatient (IOP) | 9-12 hours/week | Moderate | People who have stabilized and are ready to reintegrate into work, school, or family life while still receiving consistent clinical support and accountability. |
| Supportive Outpatient (SOP) | 1-3 hours/week | Low | Those who have completed higher levels of care and are managing recovery well but benefit from ongoing connection and relapse prevention support. |
Ultimately, choosing the right level is about finding the program that meets you where you are today while providing a clear path forward.
Core Therapies for Dual Diagnosis Recovery
Once you understand the different levels of care, the next question is obvious: what actually happens in treatment? The real "how" behind dual diagnosis recovery comes down to a handful of powerful, evidence-based therapies. These aren't just clinical buzzwords; they're proven methods for rewiring your responses to stress, cravings, and emotional pain.
Think of it like this: you wouldn't use a hammer to fix a delicate watch, and you wouldn't use tiny screwdrivers to build a house. Effective mental health and substance abuse treatment uses the right tool for the right challenge. Before diving into specifics here, it can be helpful to get a big-picture view by exploring various types of therapy for mental health to see the range of interventions available.
This integrated approach has never been more vital. The substance abuse treatment market is expected to surge from USD 15.61 billion in 2025 to USD 36.83 billion by 2034, driven by a staggering need for care. In 2023, while one in five U.S. adults required treatment, only about 24% got it, revealing a massive gap that integrated, evidence-based therapies are designed to close. You can see the full findings on the substance abuse treatment market on Precedence Research.
Cognitive Behavioral Therapy (CBT): Learning to Pilot Your Thoughts
One of the absolute cornerstones of dual diagnosis care is Cognitive Behavioral Therapy (CBT). At its heart, CBT works on a simple but profound principle: your thoughts, feelings, and behaviors are all linked in a continuous loop. Unchecked negative thought patterns almost always lead to self-destructive actions, like turning to a substance to cope.
Imagine your mind is a cockpit and your automatic negative thoughts are a faulty navigation system screaming that you're off course. CBT doesn't just tell you to ignore the alarm bells. It hands you the manual, teaching you how to read the instruments, spot the errors, and manually correct your flight path. You learn to challenge distorted thinking and choose healthier responses, putting you back in control.
Dialectical Behavior Therapy (DBT): Building an Emotional First-Aid Kit
For many people battling co-occurring disorders, emotions aren't just feelings—they're tidal waves that threaten to pull you under. Dialectical Behavior Therapy (DBT) was created specifically to help you navigate this emotional intensity without turning to substances to numb out.
Think of DBT as learning to build an emotional first-aid kit. It gives you practical, easy-to-use tools for specific kinds of emotional injuries:
- Mindfulness: The skill of staying present and observing your feelings without getting swept away by them.
- Distress Tolerance: Real-world techniques to survive a crisis without making things worse.
- Emotion Regulation: Strategies to manage and even change overwhelming emotions.
- Interpersonal Effectiveness: Skills for clearly communicating your needs and setting healthy boundaries.
With this kit, you're prepared to handle emotional emergencies with skill instead of substances.
EMDR: Guiding Your Brain to Heal Past Wounds
It's no secret that unresolved trauma is often a root cause of both mental health struggles and substance use. Eye Movement Desensitization and Reprocessing (EMDR) is a powerful, specialized therapy designed to help the brain properly process traumatic memories that have gotten "stuck."
When a traumatic event happens, the memory can get locked in the brain with all the original sights, sounds, and gut-wrenching feelings. EMDR uses bilateral stimulation (like guided eye movements) to act as a gentle guide, helping your brain kickstart its own natural healing process. It allows you to file the memory away correctly, so it no longer carries the same intense emotional charge and loses its power over you.
An integrated treatment plan doesn't just use one therapy; it combines individual, group, and family sessions to create a complete support system. Each modality plays a unique and vital role in building a foundation for lasting recovery.
Individual counseling offers a confidential space to untangle personal history and challenges. Group therapy crushes the isolation of addiction by connecting you with peers who truly get it. And finally, family therapy works to heal damaged relationships and build a supportive home environment, which is absolutely critical for long-term success.
Building a Fulfilling Life Beyond Treatment

Real mental health and substance abuse treatment does more than help you stop using a substance. Its true purpose is to help you build a life so full of meaning, purpose, and connection that the old patterns just don't seem appealing anymore. Recovery isn’t about deprivation; it’s about construction.
This is the phase where clinical progress turns into real-world freedom. It’s about moving beyond the therapy room to develop the practical skills and supportive relationships you need to build a thriving, independent life. This is where you lay a strong foundation for the long haul.
From Clinical Healing to Real-World Skills
Sobriety is strongest when it’s backed by practical life skills that dial down stress and build up self-sufficiency. Many people enter recovery without a solid grasp of these core abilities—not because of any personal failing, but because all their energy was consumed by just surviving. Learning these skills helps dismantle common relapse triggers before they can even take hold.
High-quality outpatient programs weave this kind of training right into their curriculum, focusing on crucial areas like:
- Financial Literacy: Learning to budget, save, and manage money responsibly is a game-changer. It removes one of the biggest sources of stress people face.
- Stress Management: Developing healthy ways to cope—like mindfulness, hitting the gym, or finding a creative outlet—gives you real alternatives when life’s pressure starts to mount.
- Vocational Support: Getting help with a resume, practicing interview skills, or exploring educational paths can open doors to meaningful work, which builds both self-esteem and stability.
Think of these skills as the building blocks of a resilient life. They empower you to handle daily challenges with confidence, proving to yourself that you can absolutely thrive without substances.
The Power of a Sober Community
One of the most powerful forces in long-term recovery is connection. Addiction thrives in isolation, but healing happens in community. A supportive sober network acts as a bridge, guiding you from the structured environment of a treatment program to a fully independent life.
The ultimate goal isn't just to stop using; it's to build a life you don't want to escape from. This happens when you find your people—a community that understands, supports, and celebrates your journey.
This community offers so much more than accountability. It’s a space for genuine friendship, shared experiences, and sober fun. Whether it's through alumni groups, mutual support meetings, or sober social events, these connections are a constant reminder that you are not alone. They reinforce the reality that a joyful, engaging life isn't just possible—it's happening all around you.
Rebuilding Relationships and Finding Purpose
Beyond practical skills and community, long-term fulfillment often grows from healing relationships and rediscovering a sense of purpose. Family therapy can be incredibly helpful here, working to mend broken trust and establish healthier ways of communicating. As these core relationships get stronger, your primary support system becomes a source of encouragement instead of conflict.
The stakes are incredibly high, and the need for this holistic approach is crystal clear. Every year, harmful substance use leads to over 3 million deaths worldwide. In 2023, 48.5 million people in the U.S. had a substance use disorder, yet only about 1 in 4 received the treatment they desperately needed. To learn more about this critical gap, you can read the 2025 statistics on substance use disorders from TherapyRoute.
Ultimately, recovery is a journey of rediscovery. It's about figuring out what truly matters to you, whether that’s a new career, a creative passion, volunteer work, or simply being a present and loving family member. This is the real work: building a meaningful life, one day at a time.
How to Find the Right Integrated Program
Making the decision to get help is the single most courageous step you can take. Now, the goal is to find a high-quality program that honors that courage. Knowing what to look for transforms an overwhelming search into an empowering process of choosing the right partner for your recovery.
Finding effective mental health and substance abuse treatment isn’t about finding a quick fix. It’s about finding a supportive environment where real healing can happen. The right program will feel less like a rigid institution and more like a team of dedicated guides ready to walk alongside you. This is about reclaiming your life, and you deserve a program that treats it with that level of importance.
Your Checklist for Quality Care
When you start evaluating potential programs, focus on a few key indicators of excellence. Think of these as the non-negotiables that ensure you’re receiving care that is safe, effective, and built on a foundation of clinical skill.
A quality program will always have:
- Proper Accreditation and Licensing: Look for credentials from recognized bodies like The Joint Commission or CARF. This is your guarantee that the facility meets rigorous national standards for patient safety and care.
- Specialization in Dual Diagnosis: The program absolutely must have proven experience in treating co-occurring disorders. Their clinical team should be skilled in addressing both mental health and substance use at the same time.
- Evidence-Based Therapies: Make sure they use proven modalities like CBT, DBT, and EMDR. These are the gold-standard tools for creating lasting change, not just temporary relief.
Reaching out for help is not a sign of defeat—it is a powerful act of hope. It’s the moment you decide your future is more important than your past.
Once you’ve shortlisted a few options, the next step is to pick up the phone. A brief conversation can reveal a ton about a program's culture and approach.
Come prepared with a list of questions to ask during that initial call. This helps you make a truly informed decision about where you'll invest your time and energy. Consider asking about the staff-to-client ratio, opportunities for family involvement, and what their aftercare and alumni support looks like. A transparent, compassionate response is a very good sign. Taking these steps ensures you find a place that feels right, making the path forward feel both hopeful and clear.
Frequently Asked Questions
Taking that first step toward getting help for mental health and substance abuse always brings up a lot of questions. Knowing the practical details can make the whole process feel a lot less intimidating and much more doable. Here are some straightforward answers to the things people ask us most often.
Can I Keep My Job While in an Outpatient Program?
Yes, absolutely. Outpatient programs like PHP and IOP are specifically built for this. They offer flexible schedules—including day, evening, and even virtual sessions—that allow you to get the intensive clinical care you need while keeping up with your professional life.
The whole point is to integrate recovery into your world, not pull you out of it. This setup lets you learn new coping skills in a therapy session and apply them to real-world challenges at work that very same day.
What Makes Dual Diagnosis Treatment Different?
Many standard addiction programs focus almost exclusively on stopping substance use. A dual diagnosis approach is different because it treats both the substance use disorder and any co-occurring mental health conditions—like anxiety, depression, or PTSD—at the same time.
These two issues are almost always tangled together, with one often fueling the other. Treating them as a single, integrated issue is the only way to get at the root causes of the cycle, which is what it takes to prevent relapse and build lasting wellness.
Dual diagnosis care isn't about treating two separate problems; it's about treating one whole person. This unified strategy is the key to untangling the complex relationship between mental health and substance use for good.
How Does Family Involvement Help Recovery?
Addiction and mental health struggles don't just happen to one person; they ripple out and impact the entire family. Bringing family into the recovery process is a powerful way to heal those dynamics and build a much stronger foundation for everyone's future.
Through dedicated family therapy and educational workshops, your loved ones learn to:
- Understand the nature of co-occurring disorders so they can better grasp what you're going through.
- Develop healthier ways to communicate to start rebuilding trust and resolving conflict without blame.
- Establish supportive boundaries that protect both your recovery and their own well-being.
When the whole family heals together, it creates a positive home environment that dramatically improves long-term outcomes and strengthens your most important support network.
Is Relapse Considered a Failure?
Not at all. Relapse is never seen as a failure. It’s simply a sign that your recovery plan might need a few adjustments. A good treatment program prepares you for this possibility with a solid relapse prevention strategy and provides immediate support to help you get right back on track.
The most important thing is to view it as a learning opportunity. It shines a light on a trigger you hadn't identified or a coping skill that needs more practice. Reconnecting with your clinical team and support system right away lets you address the challenge without shame, turning a tough moment into a powerful step forward.
At Altura Recovery, we provide compassionate, evidence-based care to help you navigate the path to healing without putting your life on hold. If you’re ready to take the next step, contact us for a confidential assessment.