The relationship between mental health and substance abuse is more than just a simple link—it's a deeply tangled knot, often called a co-occurring disorder or dual diagnosis. One issue almost always fuels the other. For instance, someone battling anxiety might use a substance for a moment of calm, only to find the anxiety roaring back stronger than before. To truly break this cycle, you have to treat both problems at the same time.
Untangling the Roots of Co-Occurring Disorders
Picture two vines that have grown so tightly together their roots and stems are impossible to tell apart. That’s a perfect visual for the connection between mental health conditions and substance use disorders. Trying to rip one out without touching the other just damages both. That's why the first step toward healing is understanding how they got so tangled in the first place.
When someone is struggling with both a mental health issue and a substance use problem, it creates a powerful feedback loop. The symptoms of one condition can easily trigger or worsen the other, making recovery feel like an uphill battle on shifting sand.
The Two-Way Street of Influence
This connection is never just a one-way street; the influence flows in both directions. Someone living with depression might turn to alcohol to numb their emotional pain, not realizing that alcohol itself is a depressant that will ultimately make their symptoms much worse. On the flip side, someone deep in an addiction might develop crippling anxiety or paranoia as a direct result of their substance use.
This isn't just theory; it’s a challenging reality for millions. The statistics from 2023 show that while 48.5 million people in the U.S. had a substance use disorder, the rate was dramatically higher for those with a mental illness. An estimated 51.9% of adults with a serious mental illness used illicit drugs, compared to just 21.0% of adults with no mental illness.
To better visualize this cycle, consider the table below.
The Two-Way Street of Co-Occurring Disorders
This table breaks down how mental health struggles and substance abuse feed into one another, creating a cycle that can be tough to escape without the right help.
| How Mental Health Issues Can Lead to Substance Abuse | How Substance Abuse Can Worsen Mental Health Issues |
|---|---|
| Self-Medication: Using drugs or alcohol to temporarily relieve symptoms of anxiety, depression, or trauma. | Worsening Symptoms: Substances like alcohol can deepen depression, while stimulants can amplify anxiety and trigger psychosis. |
| Social Isolation: Mental health struggles can lead to isolation, making substance use a way to cope with loneliness. | Brain Chemistry Changes: Prolonged use alters brain circuits involved in mood regulation, making it harder to feel good naturally. |
| Impaired Judgment: Conditions like bipolar disorder or ADHD can affect impulse control, increasing the risk of substance misuse. | Triggering New Issues: Heavy substance use can lead to new mental health problems, such as drug-induced paranoia or psychosis. |
| Coping with Side Effects: Some may use substances to manage the side effects of psychiatric medications. | Undermining Treatment: Substance use can interfere with the effectiveness of medications and therapy for mental health. |
As you can see, each side of the issue reinforces the other, making an integrated approach to treatment not just helpful, but essential.
This concept map helps illustrate the tangled, cyclical relationship between these two challenges.
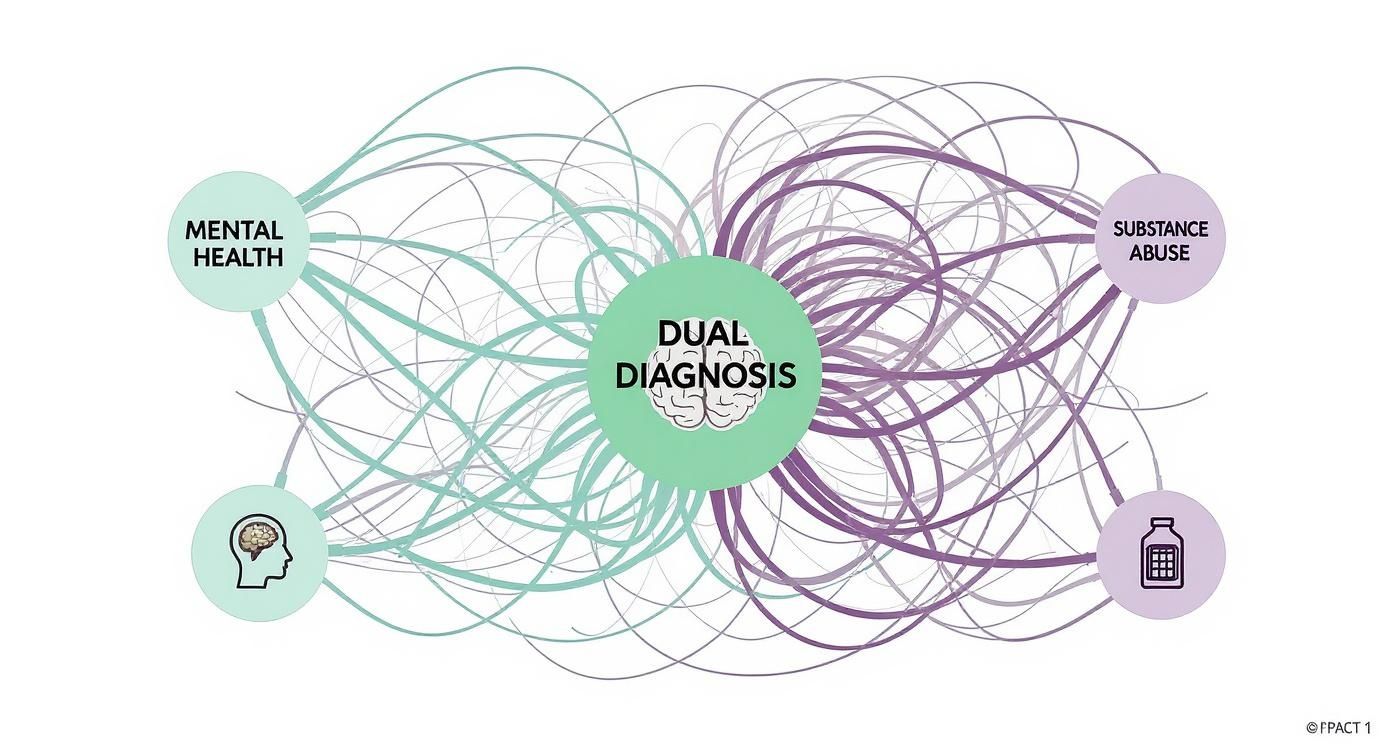
The image clearly shows how both mental health and substance abuse branch out from the core issue of a dual diagnosis, reinforcing why they must be treated as one interconnected problem.
A co-occurring disorder isn't about having two separate problems; it's about having one complex condition where mental health and substance abuse are two sides of the same coin. Addressing them together isn't just a best practice—it's essential for lasting recovery.
Understanding what makes something a substance use disorder is a critical piece of this puzzle. Knowing the specifics helps clarify why professional, integrated care is so vital for anyone caught in this challenging cycle.
Understanding Why These Conditions Occur Together

Why do mental health struggles and substance abuse so often show up as a pair? The link is no coincidence. It’s a complicated knot of biology, life experience, and the ways we learn to cope. Think of it like a puzzle where several different pieces—genetics, brain chemistry, and personal history—snap together to create the full picture.
There are a handful of core reasons that make someone more vulnerable to both challenges at the same time. These shared risk factors act like a common foundation, making it easier for both a mental health condition and a substance use disorder to take root.
Shared Biological Risk Factors
At the deepest level, our own biology can set the stage. Genetics, for instance, can predispose someone to both mental health conditions like depression or anxiety and a higher risk for addiction. This doesn't mean it's a guarantee, but it does mean some people start with a genetic blueprint that makes them more vulnerable from day one.
Brain chemistry is another huge piece of the puzzle. Neurotransmitters—our brain's chemical messengers like dopamine and serotonin—are the stars of the show when it comes to regulating mood and registering pleasure. Many mental health conditions involve an imbalance of these exact chemicals, and guess what? Substances of abuse often work by hijacking these very same pathways, forging a powerful and often destructive link.
The scale of this issue is massive. The World Health Organization reported that as of 2024, over one billion people were living with a mental health disorder. The sheer number of people facing these challenges, paired with the complexities of substance use, makes it clear why accessible, integrated care is so critical.
The Cycle of Self-Medication
One of the most common bridges between mental health and substance abuse is a pattern known as self-medication. This isn't about recreational use; it's when someone uses alcohol or drugs to try and quiet the relentless symptoms of a mental health condition.
Picture someone whose mind is constantly racing with anxiety. A few drinks might feel like they slow those thoughts down, offering a moment of peace. Or consider someone wrestling with the deep, hollow feeling of depression who uses a stimulant to feel a temporary jolt of energy or happiness.
Self-medication is an attempt to solve a problem with a tool that ultimately makes it worse. The temporary relief substances offer comes at the cost of long-term stability, often intensifying the very symptoms a person is trying to escape.
This creates a vicious cycle. The relief doesn't last, and when the substance wears off, the original symptoms often come roaring back, sometimes even stronger than before. This rebound effect pushes the person to use again, and over time, that pattern can build a physical and psychological dependence, layering a substance use disorder right on top of the original mental health struggle.
The Impact of Trauma and Stress
Our life experiences, particularly trauma and chronic stress, are powerful triggers for both mental health issues and substance use. Experiencing a traumatic event can fundamentally rewire the brain's stress-response system, leaving a person in a constant state of "fight or flight." This makes them far more susceptible to conditions like PTSD, anxiety, and depression.
For someone carrying the weight of trauma, substances can feel like a way to numb painful memories or dissociate from emotions that feel too big to handle. While this coping strategy is understandable, it prevents real healing and can quickly spiral into addiction. That's why understanding trauma-informed care principles is so crucial; it provides a framework for healing that truly respects the profound impact of past events.
In the same way, chronic stress—whether from a high-pressure job, financial worries, or a toxic relationship—slowly erodes our mental and emotional reserves. Being under that kind of prolonged strain can activate underlying mental health symptoms and make substance use look like a very tempting escape hatch.
By seeing how these pathways connect—from our DNA to the way we manage pain—it becomes obvious why treating mental health and substance abuse together isn’t just a good idea. It’s the only way to achieve real, lasting recovery.
How to Recognize the Signs of a Dual Diagnosis

Trying to spot a co-occurring disorder in yourself or someone you care about can feel incredibly confusing. It’s like trying to listen to two songs playing at the same time—it’s tough to figure out where one ends and the other begins. The symptoms of mental health conditions and substance abuse often overlap, creating a murky picture that makes it hard to see what’s really going on.
The goal isn't to make a diagnosis, but to start recognizing patterns that don't add up. Are there sudden behavioral shifts that feel out of character? Are emotional reactions becoming more extreme or unpredictable? Answering these questions can be the first step toward seeking professional guidance.
Behavioral Warning Signs to Watch For
Actions often speak louder than words, especially when someone is struggling. Significant changes in day-to-day behavior are usually the first and most visible clues that something deeper is at play.
These shifts might start small but often escalate over time. You might notice a loved one suddenly pulling away from friends, family, or hobbies they used to love. This kind of social isolation can be a classic sign of depression, but it also creates the perfect cover for substance use to take hold and grow.
Other behavioral red flags include:
- Neglecting Responsibilities: This can look like frequently missing work or school, letting bills pile up, or ignoring essential household duties.
- Risky Behaviors: Getting involved in dangerous activities like driving under the influence, having unsafe sex, or running into legal trouble often points to issues with impulse control, which can be fueled by both conditions.
- Sudden Financial Problems: A sudden, unexplained need for money can be a sign that funds are being diverted to support a substance use habit.
- Changes in Social Circles: Abruptly dropping long-time friends for a new group, especially one that encourages substance use, is a major warning sign.
Think of these signs as the check engine light on a car's dashboard. It doesn’t tell you the exact problem, but it’s a clear signal that something under the hood needs a professional's attention before it gets worse.
Emotional and Psychological Indicators
Beyond what you can see, a dual diagnosis profoundly impacts a person's inner world. Their emotional landscape can become a turbulent and unpredictable place, marked by intense mood shifts and distorted thinking.
One of the most common signs is extreme mood swings that go far beyond normal ups and downs. A person might swing from euphoria and high energy to deep despair and lethargy in a very short time. This volatility can be a symptom of a mental health condition like bipolar disorder, but it’s often magnified by substance use.
Keep an eye out for these other emotional and psychological signs:
- Increased Anxiety or Paranoia: Feeling constantly on edge, being suspicious of others, or having panic attacks can be driven by an anxiety disorder or induced by substance use.
- Cognitive Difficulties: Trouble concentrating, making decisions, or remembering things can stem from depression or be a direct side effect of drug or alcohol use.
- Feelings of Hopelessness: A persistent sense of despair or worthlessness is a hallmark of depression but is also a common feeling for those trapped in the cycle of addiction.
It's the overlap between symptoms that makes a dual diagnosis so tricky to identify without a professional evaluation. The table below shows just how easily a single symptom can be attributed to either a mental health disorder or a substance use disorder.
Common Overlapping Symptoms
This table highlights common symptoms and shows how they can manifest in both mental health disorders and substance use disorders, illustrating the complexity of diagnosis.
| Symptom | Manifestation in Mental Health (e.g., Depression) | Manifestation in Substance Abuse (e.g., Alcoholism) |
|---|---|---|
| Social Isolation | Withdrawing from friends and family due to lack of energy, interest, or feelings of worthlessness. | Hiding substance use from others or spending time only with those who also use. |
| Sleep Disturbances | Difficulty falling asleep, staying asleep (insomnia), or sleeping too much (hypersomnia). | Substance use disrupts natural sleep cycles, causing insomnia or excessive drowsiness. |
| Changes in Appetite | Significant weight loss or gain due to a loss of appetite or emotional eating. | Substances can suppress appetite or lead to poor nutritional choices and weight changes. |
This overlap is precisely why looking at the bigger picture is so important.
Ultimately, the most telling sign is when you see a combination of these symptoms. If you notice behavioral, emotional, and physical changes all happening at once, it strongly suggests a complex problem that needs an integrated approach to heal effectively.
Why Integrated Treatment Is the Key to Recovery
When you’re struggling with both a mental health condition and a substance use disorder, treatment can’t be an either-or choice. For years, the approach was often siloed, forcing people to pick which problem to tackle first. You might have been told, "Get sober, and then we'll work on your depression," or the other way around. This outdated, sequential model usually failed because it completely missed the point: these conditions are deeply intertwined.
Think about trying to fix a car with both a flat tire and a dead battery. If you only change the tire, the car still won’t start. If you only charge the battery, you’re not going anywhere. To actually get back on the road, you have to address both problems at the same time. This is the simple, powerful idea behind integrated treatment.
What Is Integrated Treatment
Integrated treatment is a modern, evidence-based approach that addresses co-occurring disorders simultaneously. Instead of juggling separate providers in different locations, you work with a single, coordinated team that creates one cohesive treatment plan. This ensures the strategies for managing your mental health and achieving sobriety actually support each other, rather than clashing.
This method gets that one condition directly fuels the other. For instance, learning healthy coping skills for anxiety in therapy will naturally reduce the urge to self-medicate with alcohol. At the same time, getting sober clears your head, making therapies like Cognitive Behavioral Therapy (CBT) far more effective.
The Essential Components of an Integrated Plan
A strong integrated treatment plan is more than just a good idea—it’s a structured framework built on several key components that work in tandem. Each piece plays a vital role in building a solid foundation for a recovery that actually lasts.
These core components include:
- Comprehensive Assessment: It all starts with a thorough evaluation to accurately diagnose both the substance use disorder and the mental health condition. This first step ensures the entire treatment plan is built around your specific needs.
- Dual-Diagnosis Therapy: This means using therapeutic models that are specifically adapted for co-occurring disorders. Therapies like CBT and Dialectical Behavior Therapy (DBT) are incredibly effective at teaching skills to manage both cravings and mental health symptoms.
- Medication Management: A psychiatrist or medical professional carefully oversees medications for both conditions. This could include medications to ease withdrawal, reduce cravings, and stabilize your mood or reduce anxiety.
- Peer and Group Support: There is incredible power in connecting with others who just get it. Group therapy and peer support create a safe space to share experiences, build a real community, and learn from people who are on the same path.
Integrated treatment isn't about treating two separate illnesses; it's about healing one person. By addressing mental health and substance abuse in a unified way, recovery becomes more sustainable, empowering individuals to reclaim their lives fully.
Why Separate Treatment Fails
The old model of treating issues separately often locked people in a frustrating and ineffective cycle. Someone in treatment for alcoholism might watch their underlying depression get worse without alcohol as a coping mechanism. That untreated depression could then become a massive trigger for relapse, sending them right back where they started.
Likewise, someone getting therapy for anxiety while still using stimulants would find their progress constantly sabotaged. The substance use would just amplify their anxiety, making it impossible for therapeutic strategies to stick. This kind of fragmented care leaves people feeling defeated and completely misunderstood. You can learn more about how a truly integrated dual diagnosis treatment model brings all these essential pieces together for a much better outcome.
Integrated care, by contrast, stops this revolving door. It provides a stable, consistent environment where you can develop the skills and resilience needed to manage both sides of your condition. The focus shifts from temporarily fixing one problem to building a life of genuine, long-term wellness. This unified approach is the most reliable and compassionate path toward real healing and lasting freedom.
Your Practical Roadmap to Finding Help and Support
Realizing you need help is a huge first step—maybe the biggest one you'll ever take. But figuring out what to do next can feel completely overwhelming. Where do you even begin?
This section is your practical guide, designed to cut through the confusion. We'll break down the process into clear, manageable actions. It's all about moving from awareness to action, armed with the right information to find the support that truly fits.
Locating the Right Professional Care
Finding a qualified provider who specializes in co-occurring disorders is the cornerstone of effective treatment. You need a team that gets the intricate dance between mental health and substance abuse and knows how to treat both at the same time.
Look for facilities or clinicians that specifically mention "integrated treatment" or "dual diagnosis" in their services. That's the language that tells you they're equipped for this.
When you start your search, here are some solid starting points:
- Ask for Referrals: Your primary care doctor is a great first call. A trusted therapist can also point you toward specialized programs they know and respect.
- Use Online Directories: Reputable sources like the SAMHSA National Helpline can guide you to vetted local resources, saving you a lot of guesswork.
- Check with Your Insurance: Your insurance provider can give you a list of in-network specialists who cover both mental health and addiction.
Once you have a shortlist of potential providers, it's time to vet them. This isn't just about finding a program; it's about finding your program.
Key Questions to Ask a Potential Provider
Before you commit, it’s vital to ask some targeted questions. Think of it as an interview—you're hiring the best possible team for your recovery journey, and you have every right to be selective.
Here are a few non-negotiable questions to get you started:
- Do you specialize in treating co-occurring disorders? This is the most important question. A simple "yes" isn't enough; ask them to describe their integrated treatment model and what that looks like day-to-day.
- What specific therapies do you use? Look for evidence-based practices like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), or EMDR. These are proven to be effective for dual diagnosis.
- How is medication managed? Ask if they have a psychiatrist on staff who can manage medications for both your mental health and substance use needs. Coordinated care is key.
- What does family involvement look like? A strong program will offer resources and therapy for family members. Healing doesn't happen in a vacuum, and their support is a powerful asset.
Asking these questions helps you find not just any help, but the right help. You can also learn more about finding the right substance abuse therapy near you to see what options are available in your area.
Building Your Personal Support Network
Professional treatment is crucial, but your personal support network is what will sustain you for the long haul. This is your team of allies—the family, friends, and peers who offer encouragement, accountability, and a safe place to land.
This is especially critical for younger people. The burden of mental health and substance use disorders is alarmingly high in this group. Globally, 13% of the population is affected, and despite a 6.8% increase in youth mental disorders since 1990, many still don't get the care they need. This makes strong, accessible support systems more urgent than ever.
Your support network is your safety net. It’s the group of people who will celebrate your victories and help you stand back up when you stumble, reminding you that you are not alone on this journey.
Cultivating this network is an active process. It means opening up to loved ones you trust, showing up for family therapy sessions, and connecting with others who just get it. Specialized support groups like Double Trouble in Recovery or Dual Recovery Anonymous can be invaluable places to find that kind of peer support.
Developing resilience is another key piece of the puzzle. A deeper understanding of unlocking lasting self-control and focus can be incredibly empowering as you build these essential life skills. By combining professional care with a robust support system, you create a powerful, multi-layered strategy for healing.
Answers to Your Pressing Questions
When you're dealing with the tangle of mental health and substance abuse, a lot of questions come up. It's completely normal to feel a bit lost in the terminology and the "what ifs." Let's clear up some of the most common concerns with direct, straightforward answers.
What Is the Difference Between Co-Occurring Disorders and Dual Diagnosis?
You’ve probably heard both of these terms, and honestly, they're often used to describe the exact same thing. Think of "dual diagnosis" as the older, original term. Over time, clinicians and experts started shifting toward "co-occurring disorders," and there's a good reason for it.
The newer term, "co-occurring disorders," does a much better job of capturing what's really happening: a mental health condition and a substance use disorder are happening at the same time, side-by-side. It removes the suggestion that one is more important or that one is just a symptom of the other. At the end of the day, both terms point to the same reality—a complex situation that demands a single, unified treatment plan to heal properly.
Can Substance Abuse Cause a Permanent Mental Health Condition?
This is a big one, and the answer isn't a simple yes or no. Substance use can absolutely trigger temporary mental health symptoms. Think of the intense anxiety that can come from stimulants or the deep depression that often follows alcohol withdrawal. In many cases, these symptoms fade away once a person gets sober and stays that way.
However, long-term or heavy substance use can dig in deeper. It can awaken an underlying mental illness that someone was already genetically predisposed to but hadn't yet surfaced. Chronic use can also physically change the brain's chemistry and structure, potentially leading to a mental health condition that sticks around. That’s precisely why a professional assessment is so vital—it’s the only way to tell the difference between temporary, substance-induced issues and a long-standing disorder.
The line between substance use and mental health symptoms can be blurry. A professional evaluation is the only way to untangle them and map out the right path to long-term wellness.
How Can I Support a Loved One Without Enabling Their Behavior?
This is the tightrope walk so many family members face: how to show love and compassion without accidentally making it easier for the substance use to continue. The secret is to shift your energy from actions that enable the behavior to actions that truly support their recovery.
Enabling might look like making excuses for them, handing over cash no questions asked, or cleaning up the messes they make. It shields them from the natural consequences of their choices. Real support, on the other hand, encourages them to take responsibility.
Here are a few ways to offer genuine support:
- Encourage Professional Help: Don't just suggest it—help them look up treatment centers. Offer to sit with them while they make the call or even drive them to their first appointment.
- Set Clear Boundaries: Communicate what you will and will not tolerate, calmly and firmly. A great example is, "I love you unconditionally, but I cannot allow drugs or alcohol in my home."
- Participate in Family Therapy: Getting involved shows you're committed to healing as a family. It’s not just their problem; addiction impacts the entire family system.
- Take Care of Yourself First: This is non-negotiable. You can't pour from an empty cup. Find your own support in therapy or through groups like Al-Anon to protect your own mental health.
By focusing on support instead of enabling, you create an environment where your loved one is empowered to take real, meaningful steps toward getting well.
At Altura Recovery, we know it takes immense courage to ask for help with co-occurring disorders. Our compassionate team is here to provide integrated, evidence-based care that builds a solid foundation for lasting healing. Learn more about our outpatient programs and start the journey for yourself or your loved one today.