When you’re trying to heal, it’s not enough to treat just one issue while a related one continues to cause problems. That’s why effective mental health and addiction treatment has to address both conditions at the same time, a practice known as integrated care or dual diagnosis treatment.
Substance use and mental health disorders are almost always deeply tangled, with one feeding the other in a difficult cycle. Lasting recovery isn't about fixing an isolated problem—it's about healing the whole person.
Understanding the Dual Challenge of Co-Occurring Disorders
When someone struggles with both a substance use disorder and a mental health condition like depression, anxiety, or PTSD, it’s called a co-occurring disorder. Think of it like a leaning tree. You can’t just trim the branches and expect it to stand tall if the roots are damaged.
That’s what happens when you treat addiction but ignore the underlying depression, or manage anxiety without acknowledging a substance use issue. The approach is incomplete and, frankly, often ineffective.
This guide starts with a simple, powerful truth: mental health is health and is completely inseparable from your physical well-being. The two aren't separate issues; they're two sides of the same coin, each one influencing the other. For example, a person might drink to quiet their social anxiety, only to find the anxiety comes roaring back worse than ever when the alcohol wears off. This is the frustrating cycle that can feel impossible to break alone.
Why a Unified Approach Matters
The relationship between substance use and mental health is different for everyone. For some, a mental health condition like trauma or depression comes first, and substances become a way to self-medicate the pain. For others, chronic substance use actually changes the brain’s chemistry, eventually triggering a mental health disorder that wasn't there before.
An integrated treatment plan is the key to breaking this cycle. It acknowledges that both conditions must be addressed at the same time, by a single, coordinated team, to pave the way for real, sustainable recovery.
This unified method ensures that the treatment for one issue doesn't accidentally make the other one worse. It creates a clear, comprehensive roadmap for what genuine healing looks like.
In this guide, we will explore:
- The science behind why these conditions so often appear together.
- Evidence-based therapies that offer real hope and tangible skills.
- Practical steps for finding the right support for you or a loved one.
Why Integrated Treatment Is the Gold Standard
Trying to treat mental health and addiction separately is like trying to fix a leaky boat by patching only one hole at a time. It’s an outdated approach that often leaves people stuck in a frustrating loop—making progress on their anxiety, for instance, only to have it undone by untreated substance use, and vice versa.
The modern, evidence-backed solution is integrated treatment, where both conditions are addressed at the same time, by the same team, under one roof.
This approach acknowledges the destructive relationship between mental health and substance use. Think about it: someone struggling with PTSD might drink to numb intrusive memories. It works for a little while, but it also prevents them from actually processing the trauma. When the alcohol wears off, the PTSD symptoms can roar back even stronger, fueling the urge to drink again.
This creates a vicious cycle where each condition feeds the other. The substance use makes the mental health symptoms worse, and those worsening symptoms increase the reliance on the substance. Breaking this cycle requires a single, cohesive plan that understands this deep connection.
The Problem with Fragmented Care
In the past, treatment systems were completely siloed. You might have been told to get sober before you could get therapy for your depression, or that your anxiety needed to be managed before you could enter an addiction program. This created impossible barriers to care.
This fragmented model fails because it ignores the fundamental nature of co-occurring disorders. It's not a "chicken or egg" problem to be solved in order. It’s a single, intertwined issue that demands a unified response.
An integrated approach brings together a multidisciplinary team—therapists, psychiatrists, and addiction specialists—who all collaborate on your care. This ensures everyone is working from the same playbook, providing consistent support that addresses the whole person, not just a collection of symptoms.
This collaborative environment is the heart of effective mental health and addiction treatment. It gets rid of conflicting advice and ensures that the progress you make in therapy is supported by your medication plan and relapse prevention strategies, and the other way around.
The Dangers of Untreated Co-Occurring Disorders
When co-occurring disorders go untreated or are handled separately, the consequences can be severe. Constantly battling both conditions at once can lead to profound feelings of hopelessness and despair, which significantly increases the risk of self-harm and other dangerous behaviors.
Shockingly, among adults with both a substance use disorder and any mental illness, only 58.8% received treatment for at least one of those conditions. This massive treatment gap has devastating results. Suicide claimed an estimated 727,000 lives worldwide in 2021 and remains a leading cause of death among young people. Without a major shift toward integrated care, the world is projected to fall far short of the UN's goal to reduce suicide deaths, a reality highlighted in these important mental health statistics.
Benefits of a Unified Treatment Plan
Choosing an integrated program gives you a real advantage, leading to better, more sustainable outcomes. A unified plan is built to be efficient, effective, and supportive, creating a solid foundation for a recovery that lasts.
Here are the key benefits:
- Simultaneous Treatment: You work on both your mental health and substance use in the same place, at the same time. This means the skills you learn to manage anxiety can be immediately applied to your addiction triggers.
- Coordinated Care Team: Your psychiatrist, therapist, and case manager are constantly talking. Medication changes are made with full awareness of your therapeutic progress and challenges.
- Improved Outcomes: Research consistently shows that people in integrated programs have higher rates of long-term sobriety, better management of mental health symptoms, and an improved overall quality of life.
- Reduced Stigma: Integrated programs treat mental health and addiction as interconnected health issues, which helps reduce the shame that can stop people from asking for help in the first place.
Ultimately, integrated treatment is the gold standard because it’s the most logical, compassionate, and effective way to deal with the complex reality of co-occurring disorders. It offers a clear path toward healing by treating you as a whole person, giving you the tools to manage both conditions and build a resilient future.
Exploring Evidence-Based Therapies That Work
Effective treatment for co-occurring disorders isn't a single magic bullet. It’s more like a skilled tradesperson's toolkit, filled with evidence-based therapies—specialized methods that are rigorously studied and proven to help people build real, lasting recovery skills. These therapies give you the practical strategies you need to manage both your mental health and addiction at the same time.
Think of it like building a house. You wouldn't use just a hammer; you'd need saws, drills, and measuring tapes, too. In the same way, a strong treatment plan uses different therapeutic tools, each with a specific job, to construct a solid foundation for your recovery.
This image shows the vicious cycle that keeps so many people stuck. A mental health condition can lead someone to use substances to cope, but that substance use only makes the original condition worse. It’s a feedback loop that integrated, evidence-based therapies are designed to break.
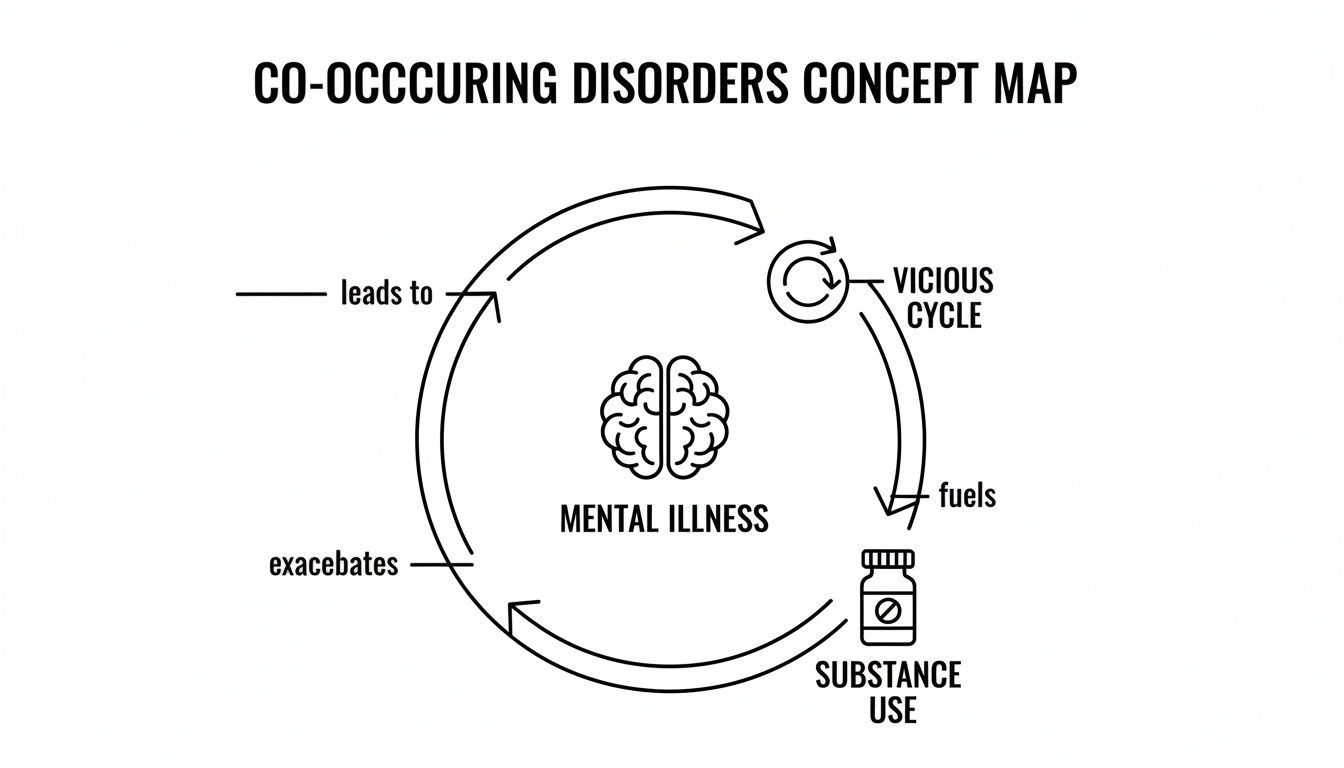
Breaking this cycle is where the real work of recovery begins, and it’s why using the right tools for the job is absolutely critical.
Cognitive Behavioral Therapy for Rewiring Thoughts
One of the most powerful and widely used tools is Cognitive Behavioral Therapy (CBT). At its heart, CBT operates on a simple but profound idea: our thoughts, feelings, and behaviors are all connected. If we can change the negative or inaccurate thought patterns we’ve fallen into, we can change how we feel and what we do.
For someone with co-occurring disorders, this is a game-changer. CBT helps you pinpoint the exact thoughts that trigger anxiety or depression, which then kick off cravings for a substance. A thought like, "I'm a total failure, so what's the point? I might as well drink," can be challenged, reframed, and replaced with a healthier, more realistic thought and a positive coping skill.
Dialectical Behavior Therapy for Managing Emotions
While CBT is fantastic for rewiring thoughts, Dialectical Behavior Therapy (DBT) specializes in helping people manage overwhelming emotions. It was first developed for borderline personality disorder but has proven incredibly effective for anyone who struggles with emotional dysregulation—a common thread in both addiction and many mental health challenges.
DBT teaches four core skill sets:
- Mindfulness: Learning to stay grounded in the present moment without judging it.
- Distress Tolerance: Practical skills to get through a crisis without making it worse.
- Emotion Regulation: Understanding your emotions and reducing your vulnerability to painful ones.
- Interpersonal Effectiveness: Building healthier relationships and communicating your needs effectively.
These skills are vital for navigating the emotional rollercoaster of early recovery. Instead of reaching for a substance when things get intense, you can use a distress tolerance skill to get through the moment safely.
Eye Movement Desensitization and Reprocessing for Trauma
For a huge number of people, unresolved trauma is the deep root that feeds both their mental health struggles and their substance use. Eye Movement Desensitization and Reprocessing (EMDR) is a highly specialized therapy designed to help the brain properly process and heal from traumatic memories.
Traumatic events can get "stuck," causing a person to re-experience the sights, sounds, and feelings of the event as if it's happening all over again. EMDR uses bilateral stimulation (like side-to-side eye movements) to help the brain reprocess these memories, filing them away so they no longer cause intense distress. This can dramatically reduce symptoms of PTSD and remove the underlying reason for self-medicating.
Medication Management for Brain Chemistry
Therapy is the hard work of recovery, but sometimes medication is the foundation that makes that work possible. Medication-Assisted Treatment (MAT) and other forms of medication management are crucial for stabilizing brain chemistry. This isn't about replacing one drug with another; it’s about using specific, FDA-approved medications to correct physiological imbalances.
In dual diagnosis care, medication management tackles both sides of the coin. An antidepressant might lift the fog of depression just enough for someone to engage in therapy, while another medication can reduce intense cravings, giving them the mental space to actually learn and practice new skills.
To help you see how these powerful therapies fit together, here’s a quick-glance comparison of what they do and who they’re best for.
Comparing Key Therapies for Co-Occurring Disorders
| Therapy | Primary Focus | Best Suited For |
|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Identifying and changing negative thought patterns and behaviors. | Anxiety, depression, and learning practical coping skills to prevent relapse. |
| Dialectical Behavior Therapy (DBT) | Building skills for emotion regulation, distress tolerance, and mindfulness. | Intense mood swings, self-harm behaviors, and relationship difficulties. |
| Eye Movement Desensitization (EMDR) | Reprocessing "stuck" traumatic memories to reduce their emotional charge. | Individuals with a history of trauma or PTSD that fuels their substance use. |
| Medication Management | Stabilizing brain chemistry to reduce symptoms and support therapy. | Nearly everyone in early recovery, especially those with severe depression, anxiety, or cravings. |
This integrated approach ensures that the biological and psychological parts of recovery are addressed together. For example, when exploring different ADHD treatment options, you see a similar model of combining medication with behavioral strategies. Ultimately, these therapies work in concert to treat the whole person, giving you the tools you need not just to get well, but to build a resilient and meaningful life.
Navigating Your Outpatient Care Options
Figuring out the right level of treatment for co-occurring disorders can feel overwhelming, but it doesn't have to be. Outpatient care provides a flexible, structured path to healing that lets you stay connected to your life.
Think of it as a step-down system. The goal is to give you intensive support when you need it most, then gradually shift toward more independence as you master new recovery skills. This model ensures you’re never left with too little structure or too much pressure. Instead, it meets you exactly where you are and provides a clear, supportive path forward.
Partial Hospitalization Program (PHP): The Most Intensive Step
The highest level of outpatient support is the Partial Hospitalization Program (PHP). It offers the kind of structure you’d find in a residential facility but allows you to go home each evening. This makes it the perfect starting point for anyone who needs serious daily support but doesn't require 24/7 medical monitoring.
A PHP creates a highly focused environment where you can stabilize and build a solid foundation for your recovery. It’s designed to be immersive, giving you the time and space to concentrate completely on your healing.
A typical week in a PHP looks like this:
- Time Commitment: You'll attend treatment for 5-6 hours per day, five days a week.
- Therapeutic Structure: Your days are packed with individual therapy, multiple group sessions, psychiatric check-ins, and skill-building workshops.
- Who It's For: It’s ideal for people stepping down from an inpatient or detox program, or for those who find that a less intensive program just isn't enough.
Intensive Outpatient Program (IOP): Balancing Treatment and Life
Once you have a strong footing, the next step is often an Intensive Outpatient Program (IOP). An IOP delivers robust clinical care with a lot more flexibility, helping you ease back into work, school, and family routines. It’s the bridge between the high structure of a PHP and true personal autonomy.
You’ll continue to receive consistent, high-quality therapy, but with a smaller time commitment. This gives you the chance to apply the coping skills you’ve learned to real-world situations, all while having the safety net of your treatment team still firmly in place.
An IOP is where your recovery skills get road-tested. It challenges you to handle daily triggers and stressors while still giving you the frequent support of therapists and peers to process what’s happening and keep you on track.
This level of care is all about building confidence. You learn to manage your mental health and sobriety as you start taking on more of your normal responsibilities again.
Supportive Outpatient Program (SOP): Maintaining Long-Term Wellness
The final step on the outpatient ladder is the Supportive Outpatient Program (SOP), sometimes called aftercare. This is the least time-intensive option, created to provide ongoing support as you fully dive back into your life. The focus shifts from intensive skill-building to maintenance and relapse prevention.
An SOP acts as a vital long-term anchor. It helps you navigate the inevitable challenges that pop up long after your initial treatment is over, keeping you connected to a positive community and giving you a place to tackle issues before they become crises.
Most SOPs involve meeting just once or twice a week for group therapy. This ensures you stay tethered to your recovery foundation while living a full, independent life—a key ingredient for successful, lasting wellness.
Building a Lasting Support System for Recovery
Walking out the door after completing a treatment program is a massive win, but the real work is just beginning. Long-term recovery isn't built in a clinical setting; it's forged in the day-to-day grind of real life, supported by a strong foundation that extends far beyond therapy sessions.
Think of it this way: formal treatment is like learning to fly in a high-tech simulator. You master the controls in a safe environment. Aftercare and family support are the real-world conditions—the crosswinds and turbulence—where you actually apply those skills to stay airborne.
This next phase rests on two core pillars: a healthy family system and a rock-solid aftercare plan. Together, they form a critical bridge from the structure of a program to a life of genuine, sustainable wellness.
The need for these support networks is more urgent than ever. The global mental health crisis has reached a staggering scale, with over one billion people now living with a mental health condition. This isn't just a statistic; it's a clear signal that accessible, effective, and lasting support systems are essential. You can dive deeper into these global insights from the World Health Organization.
Transforming the Family Dynamic
Addiction and mental health struggles never happen in a vacuum—they send shockwaves through the entire family. Relationships get tangled in mistrust, codependency, and broken communication, leaving everyone exhausted and hurt. Family therapy and education are designed to start healing those wounds.
These programs aren't about pointing fingers. They help everyone understand the science behind addiction and mental health, which helps strip away the blame and shame that keep families stuck. Loved ones learn how to set healthy boundaries, communicate their needs without conflict, and stop enabling behaviors that—despite good intentions—actually fuel the problem.
The goal is to transform the family from a source of stress into a cornerstone of support.
A healthy family system acts as a safety net, providing both encouragement and loving accountability. It turns the home into a safe space for healing, not a minefield of triggers—and that’s absolutely vital for long-term recovery.
Crafting a Proactive Aftercare Plan
An aftercare plan is your personal roadmap for staying sober and mentally well after leaving a structured program. This isn't just a list of vague intentions; it's a concrete, actionable strategy for navigating life's curveballs without falling back on old coping mechanisms.
A strong plan anticipates potential roadblocks and lays out exactly what you'll do when they show up. It's a living document, tailored to your specific needs and designed to evolve as you grow.
Key pieces of an effective aftercare plan usually include:
- Ongoing Therapy: Regular sessions with a therapist give you a dedicated space to process challenges, sharpen your coping skills, and tackle any new issues that pop up. This continued professional guidance is a key part of staying on track.
- Peer Support Groups: There's incredible power in connecting with people who just get it. Groups like Alcoholics Anonymous (AA), Narcotics Anonymous (NA), or SMART Recovery offer a built-in community of understanding, accountability, and shared hope.
- Relapse Prevention Strategies: This means getting brutally honest about your personal triggers—the people, places, and feelings that spark cravings. From there, you develop specific, healthy ways to respond to them. It’s about playing offense, not defense.
Ultimately, aftercare isn't some optional add-on. It's an integral part of successful mental health and addiction treatment. It provides the structure, community, and accountability needed to turn short-term wins into a lifetime of real, sustainable freedom.
How to Find the Right Treatment Program for You
Picking the right partner for your recovery is one of the biggest decisions you’ll make. Not every program is built the same, and finding a center that actually gets the complexities of co-occurring disorders is non-negotiable. Your goal is to find high-quality, proven care that fits your specific situation.
The search can feel overwhelming, but asking the right questions changes everything. Think of it like you’re interviewing a critical business partner—you need to make sure their skills, values, and methods line up with your goals. Getting this part right lays the foundation for a recovery that lasts.
Your Vetting Checklist: Essential Questions to Ask
Before you commit to anything, you need to do your homework. A good provider will be transparent and happy to answer your questions. While resources from local health authorities can be a good starting point for Texans, you still need to vet each center on its own merits.
Here’s a checklist of make-or-break questions to guide your search:
- Do you offer true integrated treatment? Ask them point-blank: Is there a dedicated, in-house team that treats both mental health and substance use at the same time? Steer clear of programs that refer psychiatric care out or make you tackle one issue before the other.
- What are your licenses and accreditations? Look for state licensing plus accreditation from respected organizations like The Joint Commission or CARF. These certifications aren't just fancy plaques; they are a baseline for quality and safety.
- Which evidence-based therapies do you use? A solid program will offer a blend of proven methods like CBT, DBT, and EMDR. Follow up by asking how they personalize therapy plans for each client.
- What are your staff's qualifications? Dig into the credentials of the clinical team. You want to see licensed professionals like LPCs (Licensed Professional Counselors), LCSWs (Licensed Clinical Social Workers), and medical doctors or psychiatrists actively overseeing the care.
A truly integrated program doesn't just have a psychiatrist on call. It has a collaborative team where therapists and medical staff talk daily about your progress. That unified approach is the secret sauce of effective mental health and addiction treatment.
Considering the Practical Details
Beyond the clinical side, the program has to actually work for your life. The best treatment in the world is useless if you can't stick with it. Logistics like insurance, location, and scheduling are just as important as the therapy itself.
Your first step should be calling the admissions team to check your insurance benefits. They are pros at this and can break down your coverage in plain English, saving you hours of frustration. Don’t let financial questions stop you from making that call.
Next, look at the program's structure and location. For Houston locals who need outpatient care, a center like Altura Recovery can offer the flexibility to fit treatment around work or family. Whether you need an intensive Partial Hospitalization Program (PHP) or a more adaptable Intensive Outpatient Program (IOP), finding the right structure makes all the difference in building a sustainable recovery.
Frequently Asked Questions About Treatment
Stepping into treatment for mental health and addiction can feel like navigating in the dark. It’s totally normal to have a ton of questions about what the process actually looks like day-to-day. We’ve put together some straightforward answers to the most common questions we hear, hoping to clear things up and give you the confidence to move forward.
Think of knowledge as the first tool in your recovery toolkit. Just understanding the practical side of things can dial down the anxiety for you and your family in a big way.
How Long Does Treatment Last?
This is probably the number one question we get, and the honest answer is: there’s no magic number. A high-quality program doesn’t run on a rigid calendar; it builds a timeline around your personal progress and specific needs.
For instance, a Partial Hospitalization Program (PHP) might last several weeks, giving you intensive daily support, while an Intensive Outpatient Program (IOP) typically runs for 8-12 weeks. The real focus is always on helping you find stability and build the coping skills you need for the long haul. Your clinical team will be with you every step of the way, adjusting the plan as you hit your goals and making sure you only step down to a lower level of care when you’re truly ready.
Will Insurance Cover My Treatment?
Worries about cost should never stop you from getting the help you deserve. The good news is that under federal law, most major insurance plans are required to provide coverage for both mental health and substance use disorder treatment.
That said, the exact details of what your plan covers can get a little tricky. Here’s what you need to look out for:
- In-Network vs. Out-of-Network: Your plan will have a list of preferred providers where you’ll get the best coverage.
- Deductibles and Copays: You’ll likely be responsible for a portion of the cost before your insurance kicks in fully.
- Approved Length of Stay: The insurance company might pre-authorize a specific number of days or weeks for a certain level of care.
The best first move you can make is to call a treatment center’s admissions team. They’re pros at navigating the insurance maze and can verify your benefits—usually for free—and explain exactly what your plan covers in plain English.
What Is the Difference Between a Psychiatrist and a Therapist?
When you’re in an integrated care program, you’ll have both a psychiatrist and a therapist on your team. They work hand-in-hand, but they each have a very distinct and important role to play in your recovery.
Think of them as a coordinated crew for your mind and body. The psychiatrist is like the medical expert who diagnoses conditions and manages any necessary medication. Meanwhile, the therapist is your guide in talk therapy, helping you change behaviors and heal the underlying issues that drive them.
A psychiatrist is a medical doctor (an M.D. or D.O.) who can prescribe and manage medications to help stabilize your brain chemistry, which is often a critical piece of the puzzle. Your therapist, who might be a Licensed Professional Counselor (LPC) or a similar professional, is the one who leads your individual and group therapy sessions. They’re the ones teaching you the practical, hands-on skills you’ll use to navigate recovery every single day. This team approach makes sure your healing plan is complete from every angle.
At Altura Recovery, we know that taking this first step can feel overwhelming. Our compassionate admissions team is here to walk you through it, answer all your questions, verify your insurance, and help you find the right level of care. Visit us at https://www.alturarecovery.com to begin your journey toward lasting wellness.