Medication management is far more than just getting a prescription. Think of it as an active, ongoing partnership between you and your provider, all centered on finding the right medication—at the right dose—to help you feel and function at your best. It’s a dynamic process, not a one-time fix, focused on careful monitoring and smart adjustments to make sure your treatment is both safe and effective.
The whole point is to get the best possible results with the fewest possible side effects.
The Foundation of Your Treatment Plan
Imagine you're on a road trip toward wellness. You're in the driver's seat, but medication management gives you an expert co-pilot. This professional helps read the maps (your symptoms and feedback), navigate tricky turns, and adjust the route whenever needed. It’s a structured, collaborative process designed to take the guesswork out of treatment and put you in control.
This partnership is built on a simple but powerful idea: your treatment plan should evolve with you. Mental health isn't static, so your support shouldn't be either. As your needs change over time, having a responsive medication strategy is key to long-term success.
Core Components of Medication Management
The process isn't a straight line; it's a continuous cycle. It involves a few key phases that work together to support your recovery, ensuring your care is always aligned with your current needs and goals.
The fundamental steps include:
- Initial Assessment: This is a deep dive into your medical history, current symptoms, and what you hope to achieve. It’s where your provider really gets to know you and your unique situation.
- Personalized Prescription: Based on that thorough assessment, a specific medication and dosage are chosen. Your provider will walk you through why this medication was selected and what you can expect.
- Ongoing Monitoring: Regular check-ins are crucial. These appointments are for tracking your progress, discussing any side effects, and simply talking about how you're feeling. Your feedback is the most important part of this step.
- Strategic Adjustments: This is where the partnership really shines. Based on your response and feedback, the dosage might be fine-tuned, or the medication might be changed. It’s a collaborative decision to keep your treatment working for you.
This simple visual shows how assessment, prescription, and monitoring work together in a continuous loop.
Each phase flows directly into the next, creating a cycle of care that adapts to your personal journey toward wellness.
Why This Collaborative Approach Matters
The bedrock of successful medication management is a strong therapeutic alliance—that is, a trusting relationship between you and your prescriber. When you feel heard and respected, you're more likely to give honest feedback, which is absolutely essential for making smart, informed changes to your treatment. Your active participation empowers you and puts you in the driver's seat of your own health.
This model is more important than ever as more people seek help. In fact, the global market for psychotherapeutic drugs hit about US$ 20.85 billion in 2023 and is expected to keep growing. This trend reflects a positive shift toward greater awareness and less stigma, making effective, personalized management strategies vital.
Medication management is not about finding a "magic pill." It's about finding the right support system—a combination of the right medication, the right dose, and the right professional partnership—to help you live a fuller, healthier life.
It's a process that is closely related to but distinct from other forms of care. To better understand how it fits into a broader recovery context, you can learn more about how medication-assisted treatment (MAT) is used. This structured, personalized approach removes uncertainty and helps you feel confident and supported every step of the way.
Working with Your Prescriber and Care Team
Medication management for mental health isn’t something you do alone—it’s a team sport. Your success hinges on a strong, open relationship with the professionals guiding your care. Think of them as a highly skilled pit crew in a race. Each member has a specific role, but they all work in sync to keep you running smoothly and safely.
This team is usually made up of different specialists, each bringing their own expertise to the table. Knowing who does what helps you understand who to turn to for specific needs and how all the pieces of your well-being fit together.
Who Is on Your Care Team
Your support system is built to provide well-rounded care. The key players you'll probably work with include:
- Psychiatrists: These are medical doctors (MDs or DOs) specializing in mental health. They can diagnose conditions, provide therapy, and are licensed to prescribe medication. They’re often the ones leading the medication side of your treatment.
- Psychiatric Nurse Practitioners (PMHNPs): These are advanced practice registered nurses with specialized training in psychiatry. In many states, they can diagnose conditions, offer therapy, and prescribe medications, sometimes working alongside a psychiatrist and sometimes independently.
- Therapists and Counselors: Professionals like Licensed Professional Counselors (LPCs) or Licensed Clinical Social Workers (LCSWs) provide psychotherapy, or "talk therapy." While they don't prescribe medication, their insights into your emotional state and coping skills are absolutely vital for your prescriber.
This team doesn't work in silos; they communicate and coordinate your care. For instance, your therapist might notice a subtle shift in your mood that helps your prescriber make a smart decision about a dosage adjustment. This kind of collaboration also relies on the practice of writing clear and quick patient notes, which ensures every member of your team has accurate, up-to-date information for your journey.
Your Role as an Active Partner
While your care team brings the clinical expertise, you bring the most critical information of all: your own lived experience. Your active participation isn't just helpful—it is absolutely essential for your treatment to succeed.
You are the expert on you.
This means your voice is the most important one in the room. Being an active partner means being open, honest, and engaged in every conversation and decision.
Your prescriber can see your chart, but only you can share how you truly feel. Open communication transforms a standard treatment plan into a personalized one.
Being a real partner in your care means showing up prepared for appointments, keeping track of how you’re doing, and never being afraid to speak up.
How to Communicate Effectively
To get the most out of your appointments, focus on clear and direct communication. Your input is what drives the decisions that affect your health, so it’s worth being prepared.
Here are a few practical tips to make collaboration easier:
- Track Your Symptoms: Keep a simple daily log of your mood, energy levels, sleep patterns, and any side effects. Note what time you take your medication and when you notice any changes.
- Prepare Your Questions: Before each appointment, jot down any questions or concerns you have. This way, you won’t forget something important in the moment.
- Be Honest About Everything: Don’t hold back. Discuss all aspects of your life, including sleep, diet, stress levels, and any substance use. It's all connected, and this information helps your prescriber see the complete picture.
- Speak Up About Side Effects: Never downplay or hide side effects. Even things that seem minor are important, as they can often be fixed with a simple adjustment.
Understanding Common Psychiatric Medications
Trying to make sense of psychiatric medications can feel like learning a whole new language. With so many classes, brand names, and scientific terms, it’s easy to get overwhelmed. The goal here is to give you a clear, straightforward map of the main types of medications used in mental health, minus the confusing jargon.
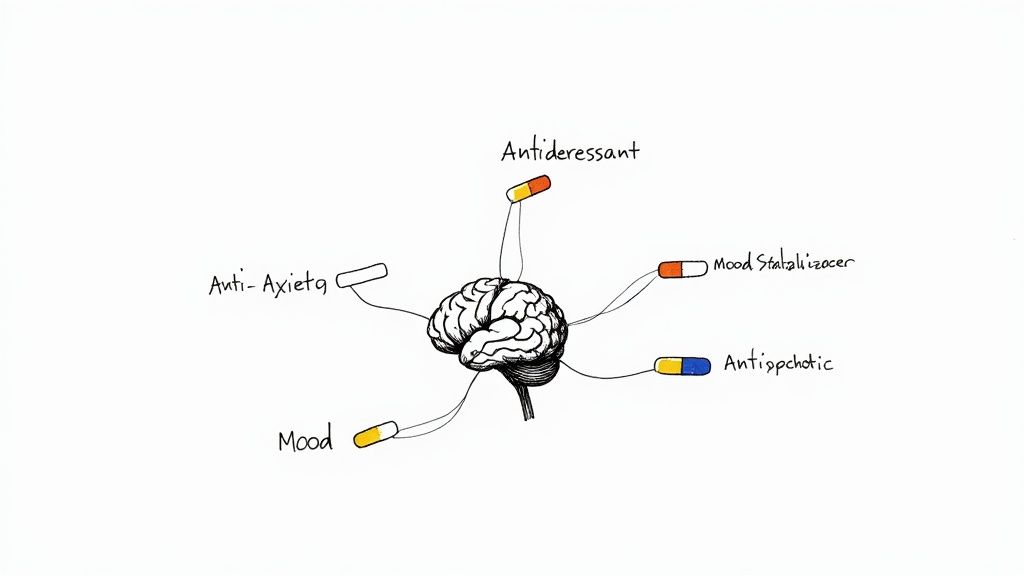
Think of these medications as highly specialized tools for rebalancing the communication pathways in your brain. Just like an electrician might adjust the wiring in a house to fix flickering lights, these medications help fine-tune the brain's chemical messengers, known as neurotransmitters. This adjustment can lead to major improvements in mood, thinking, and behavior.
Antidepressants For Mood and More
When most people hear "antidepressants," they immediately think of depression. And while they are a primary treatment for major depressive disorder, their use is much broader. Many are also prescribed to treat anxiety disorders, obsessive-compulsive disorder (OCD), and even some forms of chronic pain.
These medications primarily work on neurotransmitters like serotonin and norepinephrine, which are key players in regulating our mood and emotions. The most common type you'll hear about are Selective Serotonin Reuptake Inhibitors (SSRIs).
- How SSRIs Work: Imagine serotonin is a message being passed between two brain cells. Normally, after the message is sent, the sending cell quickly reabsorbs it. SSRIs block that reabsorption process, leaving more serotonin available in the gap between the cells. This helps strengthen the signal and improve communication.
It’s crucial to know that antidepressants often take four to six weeks to reach their full effect. This isn't a sign that something is wrong; it's a normal part of the process, and sticking with it consistently is key.
Anti-Anxiety Medications For Calm and Relief
Anti-anxiety medications, also called anxiolytics, are designed to reduce the intense, overwhelming feelings that come with anxiety disorders. They can help quiet physical symptoms like a racing heart and shakiness, along with the mental chatter of constant worry and fear.
A well-known class is benzodiazepines. These are powerful and fast-acting, often used for short-term relief during panic attacks or periods of extreme anxiety. Because they carry a risk of dependence, they are prescribed with great care and are not typically meant for long-term daily use.
For ongoing anxiety management, other medications like certain antidepressants (SSRIs are a go-to here) and drugs like buspirone are often the first choice. They effectively manage anxiety without carrying the same dependence risk.
The goal of medication management isn't to find a single "magic bullet" drug. It's about finding the right key for the right lock—the specific medication that fits your unique brain chemistry and life circumstances. Treatment is highly personal, and what works wonders for one person might not be the right fit for another.
Mood Stabilizers For Emotional Equilibrium
For conditions like bipolar disorder, mood stabilizers are the foundation of treatment. As the name suggests, their main job is to prevent moods from swinging to extreme highs (mania or hypomania) or crushing lows (depression).
Think of a mood stabilizer like a ballast on a ship. It doesn't stop the waves—life’s normal ups and downs—but it keeps the ship steady and prevents it from capsizing in a storm.
Lithium is one of the oldest and most effective mood stabilizers available. Other options include certain anticonvulsant medications, which were first created to treat seizures but were found to be incredibly effective at evening out mood as well.
Antipsychotics For Clarity of Thought
Antipsychotic medications were originally developed to treat psychosis—a condition involving a break from reality, with symptoms like hallucinations or delusions, which is a hallmark of schizophrenia. Over the years, however, their use has expanded quite a bit.
Today, antipsychotics are also used to treat bipolar disorder (often with a mood stabilizer) and sometimes in lower doses to boost the effectiveness of other medications for severe depression or anxiety that haven't responded to first-line treatments.
They fall into two main camps:
- First-generation (typical) antipsychotics: These are the older medications in the class.
- Second-generation (atypical) antipsychotics: These newer drugs often have a different side-effect profile, making them a better choice in many situations.
Getting familiar with these basic categories can help you feel more prepared and confident when you talk about options with your provider. It empowers you to ask smarter questions and become an active partner in your own care.
Mastering Medication Adherence and Safety
Getting a prescription filled is the easy part. The real work—and where the healing truly begins—is taking it consistently. This is what we call medication adherence: sticking to the plan your doctor laid out for you, day in and day out.
Think of it like watering a plant. One splash of water won't make it grow. But consistent, regular care allows it to put down roots and flourish. In the same way, psychiatric medications need to build up in your system to work effectively.
Of course, life gets in the way. It's easy to forget a dose on a chaotic morning, struggle with a side effect, or feel overwhelmed by the cost of a refill. Mastering adherence isn't about being perfect; it's about creating a simple, reliable system that makes taking your medication a seamless part of your daily rhythm.
This is an incredibly empowering part of recovery. You're taking direct, daily action to support your own progress.
Practical Strategies for Staying on Track
Building a solid routine around your medication is the single most effective way to stay consistent. This isn’t about raw willpower; it's about creating smart habits that do the heavy lifting for you.
Here are a few simple but powerful strategies our clients use to build consistency:
- Get a Pill Organizer: This is a game-changer. Setting up a weekly organizer takes five minutes on a Sunday night, but it removes the daily guesswork and "did I or didn't I?" anxiety.
- Set Digital Reminders: Use your phone or smartwatch to set recurring daily alarms. Label the alarm with the medication's name so you know exactly what it’s for.
- Anchor It to a Daily Habit: Tie your medication time to something you already do without thinking, like brewing your morning coffee or brushing your teeth before bed. This is called "habit stacking," and it's incredibly effective.
- Keep It Visible: Store your medication somewhere you’ll see it every day, like on your nightstand or next to the coffee maker (as long as it’s safely out of reach of children and pets).
These small steps remove the mental load of remembering, making adherence feel automatic instead of like another chore on your to-do list.
Navigating Medication Safety
Adherence and safety are two sides of the same coin. Proper medication management for mental health is about more than just taking your pills on time; it’s about understanding how to use them safely to avoid complications or dangerous interactions.
One of the most important rules is to never stop taking your medication abruptly without talking to your provider first. Many psychiatric medications need to be tapered down gradually to prevent uncomfortable or even dangerous withdrawal symptoms. Stopping suddenly can undo all your progress and leave you feeling much worse than before.
It’s also crucial to be open with your prescriber about everything else you’re taking. This includes:
- Over-the-counter drugs like allergy pills or pain relievers
- Herbal supplements, vitamins, and teas
- Alcohol and any recreational drugs
Certain combinations can be risky. For example, knowing the dangers of mixing stimulants and alcohol is vital for anyone in recovery. Making sure you understand questions like whether you can you drink alcohol on Adderall is a key part of making informed, safe choices for your health.
The Power of Consistency
Sticking to your medication plan unlocks significant benefits, while inconsistency can actively set your recovery back. Seeing the two side-by-side makes the importance of adherence incredibly clear.
| Benefits of Adherence | Risks of Non-Adherence |
|---|---|
| Stable Progress: Allows medication to reach and maintain effective levels, leading to sustained relief from symptoms. | Treatment Failure: Symptoms may return or worsen, making it seem like the medication isn't working at all. |
| Accurate Monitoring: Helps your provider see if the medication and dosage are truly right for you, allowing for smart adjustments. | Withdrawal Symptoms: Can cause physical and psychological distress, like nausea, dizziness, brain zaps, or a spike in anxiety. |
| Reduced Relapse Risk: Consistent use is one of the strongest predictors of long-term stability and a lower risk of relapse. | Delayed Recovery: Inconsistent use can drag out the process of finding an effective treatment plan, adding months of frustration. |
Taking control of your medication adherence is one of the most direct ways to invest in your own well-being. It’s a daily commitment to your mental health that pays off in stability, progress, and lasting recovery.
How Medication Management Fits into Holistic Care
Medication can be an incredibly powerful tool for mental health, but it’s almost never the whole story. For real, lasting wellness, medication management has to be part of a much bigger picture—one crucial piece of a puzzle that also includes therapy, lifestyle changes, and a strong support system.
Think of it like building a sturdy chair. Medication can be a strong leg, providing essential stability. But without the other legs—therapy for skills, healthy habits for resilience, and relationships for support—the chair is going to be wobbly and unreliable. A good treatment plan integrates all of these elements to create a solid foundation for recovery.
At Altura Recovery, this integrated approach is the core of our philosophy. We don’t see medication as a standalone fix. We see it as a support that makes every other part of recovery more effective.
The Synergy of Medication and Therapy
Medication and therapy aren't an either-or choice; they're a powerful combination where each one enhances the other. Medication can help stabilize your mood and dial down overwhelming symptoms, which in turn clears up the mental space you need to fully engage in therapy. When you’re not fighting intense anxiety or deep depression just to get through the day, you can actually focus on learning new coping skills and processing difficult experiences.
For example, someone with severe social anxiety might find it nearly impossible to even walk into a group therapy session. A carefully prescribed anti-anxiety medication can lower their physiological stress just enough to get them through the door, participate, and start building connections. The medication makes the therapy accessible, and the therapy provides the long-term skills to manage anxiety without relying solely on a pill. This dynamic relationship is a core part of effective care, and you can learn more about how therapy and medication work together in recovery.
Medication can turn down the volume on your symptoms, allowing you to hear the lessons of therapy more clearly.
This collaborative model ensures your treatment is working on multiple levels. It addresses brain chemistry while you're simultaneously building the emotional and behavioral skills needed for a fulfilling life.
Integrating Care for Co-Occurring Disorders
Many people who come to us for mental health support are also dealing with a substance use disorder. When these two conditions exist together, we call them co-occurring disorders or a dual diagnosis. Trying to treat them separately is a recipe for frustration, as one condition almost always makes the other one worse.
This is where a unified treatment plan becomes absolutely vital. At Altura Recovery, our psychiatrists work side-by-side with therapists and addiction counselors to create a seamless strategy. The medical team makes sure any prescribed psychiatric medication is safe, non-addictive, and won't interfere with your sobriety.
At the same time, the therapy team is addressing the underlying issues that often fuel both conditions, like trauma or chronic stress. This ensures the medication plan supports, rather than complicates, your journey to sobriety.
By treating the whole person—not just a set of isolated symptoms—we create a path to a more sustainable and meaningful recovery. It’s all about building a life where you feel balanced, supported, and fully in control of your well-being.
The Future of Personalized Mental Health Treatment
The world of mental health care is moving faster than ever, shifting toward a future where treatment is more precise, accessible, and deeply personal. Technology is at the heart of this change—not to replace the vital connection you have with your provider, but to enhance it with smarter tools and clearer insights.
This shift promises a new chapter for medication management for mental health. Imagine a system where the guesswork is dialed down and your care is fine-tuned to your unique biology. That’s exactly where we're headed, thanks to scientific breakthroughs and digital tools designed to support you every step of the way.
The Rise of Digital Tools
Technology is already breaking down old barriers to care. Telehealth platforms connect you with specialists from the comfort of your home, making it easier than ever to stay consistent with your appointments. You can learn more about how this works in our guide to virtual therapy for addiction and mental health.
Beyond virtual visits, a whole new class of tools is taking shape. Digital therapeutics (DTx) are essentially software-based treatments that can complement or even offer an alternative to traditional medications. These tools are helping people stick to their treatment plans and providing scalable solutions to meet growing mental health needs, especially in high-income countries.
Of course, challenges like regulatory hurdles and infrastructure gaps are slowing down adoption in some areas. But the potential is undeniable.
A Glimpse into Genetic Insights
One of the most exciting frontiers in personalized care is pharmacogenomic testing. This field uses your genetic information to help predict how your body might react to certain medications.
Think of it like getting a personalized user manual for your own body. A simple saliva or blood test can reveal genetic markers that influence how you break down specific drugs. This information can help your prescriber make a more informed choice from the very beginning, potentially cutting down on the trial-and-error process of finding the right fit for you.
While it's not a crystal ball, pharmacogenomic testing adds another layer of data to personalize your care. It helps steer treatment decisions toward what’s most likely to work for you.
This genetic insight doesn't replace a provider’s clinical judgment, but it adds a powerful tool to their toolkit. It can help tailor medication choices, anticipate potential side effects, and get you on the path to feeling better, faster.
As we look ahead, innovations like AI voice recognition in healthcare are also set to improve how providers manage patient data, which can further streamline documentation and sharpen decision-making.
All these advancements point toward the same goal: a future where your mental health treatment is as unique as you are. By combining expert human care with powerful new technologies, we can create more effective, responsive, and empowering paths to wellness.
Frequently Asked Questions
Navigating the world of mental health treatment can kick up a lot of questions. Getting clear, straightforward answers is a huge part of feeling confident and empowered in your own care. This section tackles some of the most common things people ask about the medication management process.
Our goal here is to give you direct answers to help you know what to expect on your journey.
How Long Will I Need Mental Health Medication?
This is one of the most personal aspects of treatment, and honestly, there’s no single answer. The timeline is different for everyone. It really depends on your specific condition, how you respond to the medication, and what your long-term wellness goals are.
For some, medication is a short-term tool to get through a crisis. For others, it provides long-term stability for a chronic condition. Think of it less like a one-time prescription and more like an ongoing conversation between you and your provider. You’ll constantly evaluate your progress together and decide on the best path forward, making adjustments as your needs change. This partnership is at the heart of effective medication management for mental health.
What Is the Difference Between a Psychiatrist and a Therapist?
Understanding the roles on your care team helps you know who to turn to for what. The main difference comes down to their medical training and what they're licensed to do.
- A psychiatrist is a medical doctor (an MD or DO) who specialized in mental health. Because of their medical background, they can diagnose conditions, provide therapy, and—most importantly—prescribe and manage medications.
- A therapist or counselor, like an LPC or LCSW, provides psychotherapy, which most of us know as talk therapy. They are the experts in helping you build coping skills, process tough emotions, and change behavioral patterns.
They often work together as a team. The insights your therapist gathers about your weekly progress can be incredibly valuable for your psychiatrist, helping them make well-informed decisions about your medication plan. It creates a truly well-rounded system of support.
Can I Improve My Mental Health Without Medication?
Absolutely. Medication is just one of many effective tools in the toolbox, and it isn’t the right fit for everyone. For many people, a combination of therapy, lifestyle changes, and building a solid support network is more than enough to see profound improvement.
Things like Cognitive Behavioral Therapy (CBT), consistent exercise, mindfulness practices, and even nutritional adjustments can make a huge difference. The best way to figure out what’s right for you is to have a professional evaluation with a qualified provider. They can help you explore all the options and map out the most effective strategy for your unique situation.
Medication can be a helpful support, but it doesn't replace the foundational work of therapy and healthy living. The most powerful treatment plans often integrate multiple strategies to support the whole person.
How Should I Talk to My Doctor About Side Effects?
Just be open and direct. Never worry that you're complaining or being difficult—reporting side effects is crucial information your provider needs to keep you safe and comfortable.
To make that conversation as productive as possible, try to be specific. It can be really helpful to keep a simple log of what you're feeling, when it happens, and how intense it is. This kind of data helps your doctor pinpoint the problem and find a solution, whether that means adjusting your dose, changing the time you take it, or trying a different medication altogether. Your feedback is what drives the entire process.
At Altura Recovery, we believe that asking questions is a sign of strength. Our integrated team of clinicians is here to provide clear answers and guide you through every step of your recovery. If you're ready for a personalized approach that combines expert medication management with compassionate therapy, contact us today to learn how our outpatient programs can support you.