When you hear the term "level of care" in addiction and mental health treatment, it’s easy to get lost in clinical jargon. But the concept is actually pretty simple: it’s about matching the intensity of clinical support to what a person needs at a specific point in their recovery. It’s not a single, rigid program but a flexible spectrum of services, ranging from 24/7 medical supervision to a weekly therapy session.
Understanding the Different Levels of Care
Trying to choose the right kind of addiction treatment can feel like trying to navigate a complex map without any directions. The phrase “level of care” might sound intimidating, but it’s a practical framework designed to meet you exactly where you are.
Think of it like any other health issue. If you catch a mild flu, your doctor probably recommends rest and fluids at home. But if you’re dealing with a serious infection, a hospital stay is necessary for your safety. Addiction and mental health care follow the same logic, offering a continuum of support that can adapt as your needs change.
Finding the Right Fit, Not the "Best" Program
The goal is never to find the single “best” program on the market. Instead, it’s about identifying the right fit for your current clinical needs, life circumstances, and recovery goals. To make sure placement is both safe and effective, professionals use standardized guidelines, like the criteria developed by the American Society of Addiction Medicine (ASAM).
This personalized approach ensures you get the precise amount of support you need—not so much that you feel overwhelmed, and not so little that you risk losing progress. It’s all about creating a stable foundation for a lasting recovery.
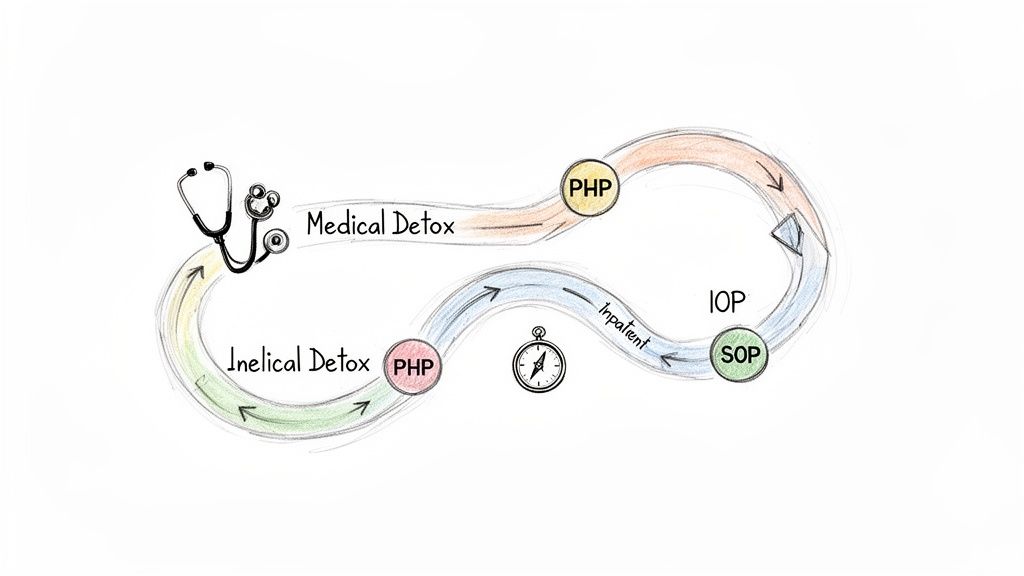
This continuum is a flexible path, not a one-way street. Some people might need to start with intensive inpatient care to get stable, while others—especially young adults juggling school or work—might begin their journey in an outpatient setting. You can learn more about these specific challenges in our guide to young adult drug treatment programs.
The demand for this kind of adaptable care is growing. The global market for drug addiction treatment is expected to jump from USD 18.91 billion in 2025 to USD 31.20 billion by 2032. This surge highlights the increasing need for effective, accessible options. If you'd like a deeper dive into the specifics of different programs, understanding comprehensive treatment options is a great place to start. This growth really underscores the shift toward flexible outpatient services that allow you to build recovery skills while getting back into the rhythm of daily life.
Starting with Safety: Medical Detox and Inpatient Treatment
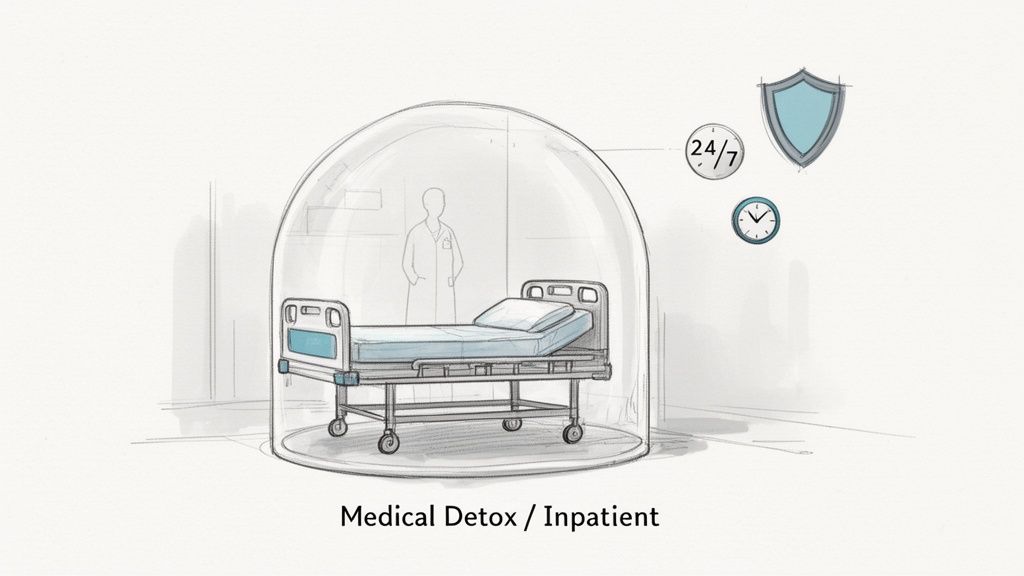
For anyone facing a severe substance use disorder, the first step in recovery has to be about one thing: safety. Before the real work of healing can begin, you need a secure foundation. This is where the highest levels of care come in, designed to manage the acute physical and psychological storm of early sobriety in a medically supervised environment.
The journey for many starts with medical detoxification, or detox. It’s easy to misunderstand this phase, so let’s be clear: detox is not addiction treatment. Think of it as the emergency room visit you make before a scheduled surgery. Its only job is to get your body through the physical crisis of withdrawal safely and as comfortably as possible, all under the watchful eye of a medical team.
This step is non-negotiable for some substances. Withdrawal from things like alcohol or benzodiazepines isn’t just uncomfortable—it can be medically dangerous, even life-threatening. With 24/7 monitoring, medical staff can administer medications to ease symptoms and prevent serious complications. You can learn more about what this process involves in our guide to common withdrawal symptoms.
The Role of Medical Detox
The entire focus of detox is to stabilize the body so the mind can eventually begin to heal. The goals are purely clinical and centered on immediate physical safety.
- Medical Stabilization: The top priority is managing acute intoxication and withdrawal to keep you safe from dangerous health complications like seizures.
- Comfort Management: While no one would call withdrawal easy, medical interventions can dramatically reduce the physical pain and distress, making the process much more bearable.
- Preparation for Treatment: By clearing the substance from your system, detox gives you the physical stability needed to fully show up for the psychological work ahead.
Once a person is no longer in acute withdrawal and is medically stable, they’re ready for the next level of care. For most, that means moving right into an inpatient or residential program.
Building a Foundation with Inpatient and Residential Treatment
After detox, inpatient or residential treatment provides a structured, live-in environment where the real therapeutic journey begins. Imagine this level of care as a protective bubble, completely removing you from the people, places, and daily stressors that trigger substance use. It offers a highly focused setting where recovery is the only thing on the agenda.
This immersive approach allows you to concentrate entirely on understanding your addiction, learning new coping skills, and digging into the underlying issues, like co-occurring mental health disorders. It’s an essential step for anyone who needs a complete environmental reset to get sober.
Inpatient care isn't just about removing someone from a negative situation; it's about immersing them in a positive, healing one. This structured setting provides the time, space, and professional support needed to build the initial framework for a sober life.
This level of care is a lifeline for people who have:
- A severe substance use disorder that requires intensive, round-the-clock support.
- A history of relapse after trying less structured forms of treatment.
- An unstable or unsupportive home life that makes sobriety nearly impossible.
- Co-occurring medical or psychiatric conditions that need integrated, 24/7 attention.
A typical day in residential care is carefully planned out, weaving together different therapies to promote healing. Your schedule might include individual counseling, group therapy, workshops on the science of addiction, and holistic practices like mindfulness or fitness. The goal is to arm you with the insights and tools you’ll need to navigate life before stepping down to a less restrictive program.
Bridging Inpatient Care and Real-World Recovery
Leaving the protected space of inpatient treatment can feel like stepping off a cliff. The sudden return to daily life is a huge shock, and this is exactly where the next level of care steps in: the Partial Hospitalization Program (PHP). It acts as a vital bridge, connecting the intensive, 24/7 support of residential care with the freedom and responsibilities of the outside world.
Think of PHP as a "day job for recovery." You commit to a full schedule of therapy and skill-building during the day—typically five to six days a week—and then head home or to a sober living residence in the evening. This structure gives you the high level of clinical support needed to make early recovery skills stick while letting you dip your toes back into real-world situations.
Who Is the Right Fit for a PHP?
A Partial Hospitalization Program isn't for someone in acute medical withdrawal, but it offers far more structure than a few weekly therapy appointments. It’s built for individuals at a key transition point: stable enough to leave a residential setting but still needing daily reinforcement to stay on track.
You might be a strong candidate for PHP if you:
- Are medically stable but still feel shaky when faced with triggers in your normal environment.
- Need more structure and accountability than a standard outpatient program can offer.
- Have a safe, supportive place to return to each evening.
- Are ready to practice new coping skills in real time while still having the safety net of daily clinical backup.
What to Expect in a Partial Hospitalization Program
A PHP schedule is immersive and designed to build practical, real-world skills for staying sober. The whole point is to arm you with the tools needed to manage triggers, regulate emotions, and start rebuilding a life you value. While every program has its own flavor, the core components usually involve a potent mix of evidence-based therapies and hands-on workshops.
PHP is where the theory of recovery meets real-world practice. It lets you face daily challenges—seeing an old friend, driving past a familiar bar—and immediately process those experiences with a clinical team the very next day.
This setup provides a crucial safety net. The routine helps you build a solid foundation, and the daily therapeutic contact ensures you're never left to figure things out alone. This is especially critical for people managing co-occurring mental health conditions like anxiety or depression alongside substance use, as the integrated care model addresses both at the same time.
The power of structured outpatient models like PHP is no secret. North America holds a huge piece of the global addiction treatment market, largely because its evidence-based outpatient programs are so effective at meeting people where they are. This flexibility is a game-changer for working professionals and young adults. In fact, outpatient completion rates can be up to 70% higher when programs are integrated with life skills and sober living support, compared to inpatient care alone. You can find more insights in the addiction treatment market report from Coherent Market Insights. This data just confirms what clinicians see every day: a step-down model that blends intensive therapy with practical life application works.
Bridging Treatment and Real Life: Outpatient Programs
Once you've built a solid foundation in a highly structured setting like residential or PHP, the next step is to start weaving recovery directly into the fabric of your daily life. This is where outpatient care comes in, marking a crucial shift from full-time treatment to part-time, focused support. Think of it as moving from the classroom to the real world, but with your teachers and mentors still on call.
This phase is all about application. You're not just learning coping skills anymore; you're actively using them to navigate rush hour traffic, tough conversations at work, and family dinners. It's where the theory of recovery becomes your lived experience.
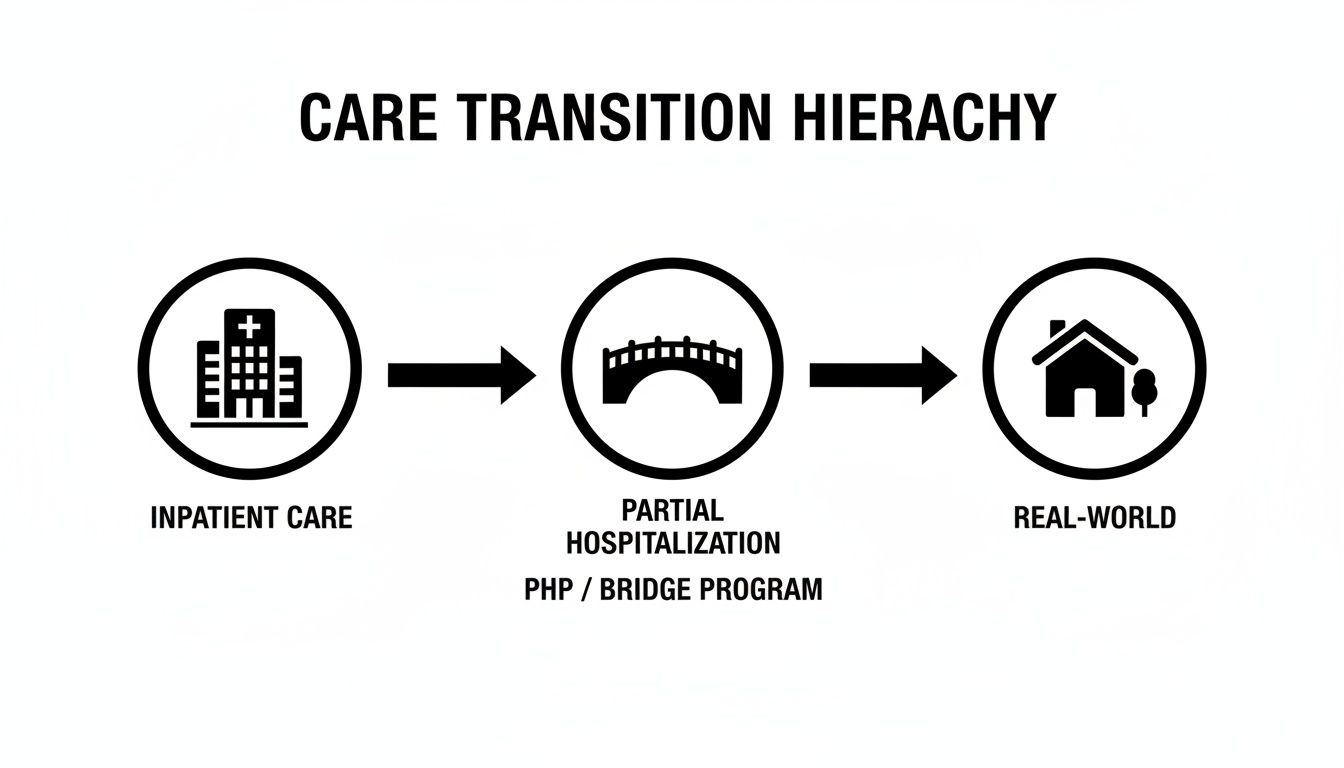
This gradual return to independence is by design. Each level provides just the right amount of support to help you succeed in the next phase, building confidence and resilience along the way.
Your Therapeutic Toolkit for Real-World Challenges
In an outpatient program, the focus is squarely on practical application. You're learning how to handle daily triggers and stressors as they happen, armed with a powerful set of evidence-based tools.
- Cognitive Behavioral Therapy (CBT): This is where you learn to spot and challenge the automatic negative thoughts that fuel substance use. It's about changing the script in your head from "I can't handle this without a drink" to "I have other ways to cope."
- Dialectical Behavior Therapy (DBT): DBT gives you concrete skills in four key areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. It’s the practical guide to managing intense feelings without turning to substances.
- Trauma-Informed Care: For many, unresolved trauma is a root cause of addiction. Therapies like Eye Movement Desensitization and Reprocessing (EMDR) help process traumatic memories so they lose their power over your daily life.
- Relapse Prevention Planning: This isn't a one-and-done lecture; it's an ongoing strategy session. You'll create a personalized playbook to identify your high-risk situations and map out specific escape routes, like how to curb alcohol cravings at a company happy hour.
Finding the Right Fit: PHP vs. IOP vs. SOP
Outpatient care isn't one-size-fits-all. The main differences between Partial Hospitalization (PHP), Intensive Outpatient (IOP), and Supportive Outpatient (SOP) come down to the time commitment and intensity of services. Understanding these distinctions helps you and your clinical team choose the level that provides enough support without overwhelming your schedule.
Here’s a quick comparison to make the differences clear:
Comparing Outpatient Levels of Care: PHP vs. IOP vs. SOP
| Feature | Partial Hospitalization (PHP) | Intensive Outpatient (IOP) | Supportive Outpatient (SOP) |
|---|---|---|---|
| Time Commitment | 20-30 hours per week (5 days/week) | 9-15 hours per week (3-5 days/week) | 1-3 hours per week (1-2 days/week) |
| Typical Schedule | Daytime program, like a full-time job | Morning or evening sessions | Flexible, often weekly check-ins |
| Clinical Focus | Intense stabilization and skill-building | Integrating skills into daily life | Long-term maintenance and support |
| Ideal For | Stepping down from inpatient; high need for structure | Balancing work/school with robust treatment | Maintaining recovery after IOP; milder cases |
| Medical Oversight | Regular access to medical/psychiatric staff | As-needed medical and psychiatric check-ins | Primarily therapeutic and peer support |
| Structure Level | High | Moderate | Low |
Essentially, as you move from PHP to IOP and then to SOP, you are gradually taking back more control and independence over your daily schedule. Each step is designed to ensure you feel confident and equipped before moving to the next, less intensive phase of your recovery journey.
Building a Life Where Sobriety Feels Natural
Ultimately, the goal of outpatient care is to help you build a life where sobriety feels sustainable, not forced. You attend group and individual therapy, check in with your clinical team, and then immediately apply what you've learned at your job, in your classes, or at the dinner table.
An outpatient program is the training ground where you prove to yourself that you can live a full, meaningful life without substances. It provides the perfect balance of structure and freedom, empowering you to take ownership of your recovery.
This approach recognizes that recovery is a dynamic, real-world process. It's a principle seen across many types of care; for example, resources like a guide to home care services for seniors also show how support can be effectively integrated into a person’s daily environment. By practicing sobriety in the real world with a safety net still in place, you build the confidence and resilience needed for long-term success. You’re not just learning skills—you’re turning them into lasting habits.
Building a Foundation for Lifelong Sobriety
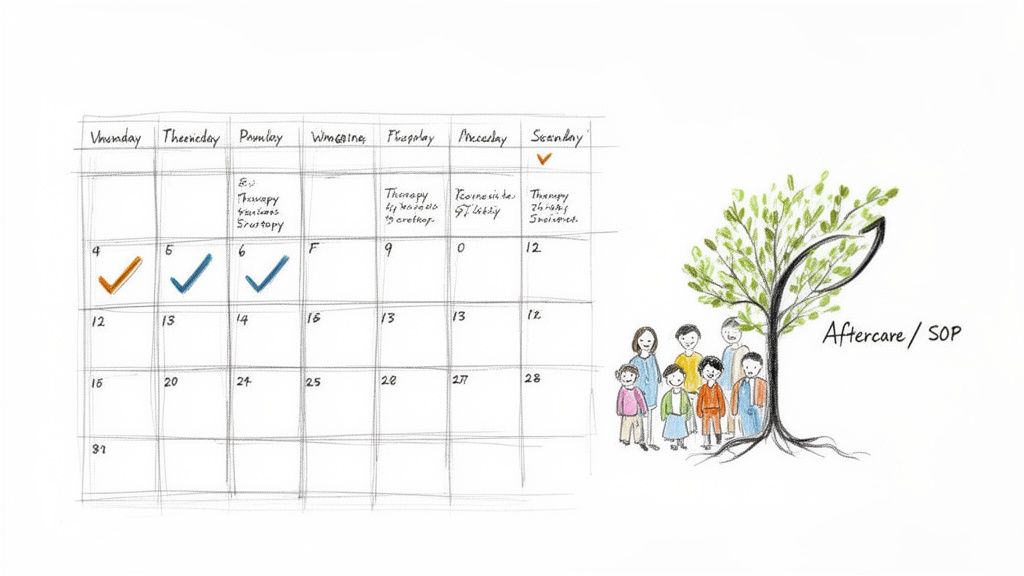
Recovery doesn’t have a finish line. The day a structured treatment program ends isn't a graduation from sobriety—it's the first day of putting everything you’ve learned into practice. Think of it like physical therapy: finishing your sessions doesn’t mean you stop doing the exercises. You have to keep them up to maintain your strength. The same is true for sobriety.
This final phase of care, known as aftercare, is less about intensive intervention and more about sustainable maintenance. It's about building a framework around your new life to protect the hard-won progress you’ve made.
Fine-Tuning Your Recovery with Supportive Outpatient Programs
One of the first steps in a solid aftercare plan is often a Supportive Outpatient Program (SOP). Think of an SOP as a regular tune-up for your recovery. After moving on from a more demanding program like IOP, an SOP offers a consistent, low-commitment touchpoint to keep you anchored.
Typically, this just means a few hours of therapy each week. The goal is to reinforce your coping skills and give you a safe space to troubleshoot the new challenges that real life inevitably throws your way. It’s the perfect blend of accountability and growing autonomy.
Aftercare isn't a sign that treatment failed; it's the strategy that makes treatment last. It’s the ongoing commitment to wellness that turns short-term sobriety into a lifetime of recovery.
By staying connected to a clinical team, you make sure that small bumps in the road don't turn into major threats to your sobriety. This proactive approach is exactly how you build a resilient, long-term recovery.
The Broader World of Aftercare
Beyond the structure of an SOP, aftercare blossoms into a rich ecosystem of ongoing support. It’s about weaving a strong social and emotional safety net that can catch you when life gets tough. This is what truly makes recovery a journey, not a destination.
A robust aftercare plan usually includes a few key components:
- Support Groups: Peer-led groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) offer something priceless: community and shared experience. They provide a sense of belonging and 24/7 encouragement from people who genuinely get what you're going through.
- Ongoing Individual Therapy: Continuing to meet with a therapist allows you to work through deeper personal issues, manage any co-occurring mental health conditions, and refine your life goals in sobriety.
- Alumni Networks: Many treatment centers, including Altura Recovery, have active alumni programs. These networks offer social events, mentorship opportunities, and a powerful reminder that you are part of a community that is rooting for your success.
The core message couldn't be simpler: staying connected is everything. A strong support system provides the encouragement and accountability needed to navigate life's inevitable ups and downs without falling back on old habits. Exploring different relapse prevention activities for groups is a fantastic way to strengthen these connections.
This final level of care ensures the foundation you’ve built is not just stable, but strong enough to support a fulfilling life for years to come.
How to Navigate Your Recovery Journey with Confidence
Choosing the right level of care is the first critical decision, but understanding how all the pieces fit together is what makes recovery stick. The journey isn’t about finishing one program and getting a graduation certificate. It's a living, breathing process of moving from intensive support toward greater independence, always with a trusted safety net in place.
This is often called the "step-down" model, and it's the backbone of a solid recovery path. You start with the high structure needed to get stable, then gradually transition to levels of care that weave more naturally into your daily life. It’s how you build confidence and test-drive your new coping skills in the real world while still anchored to a clinical team.
Think of it as moving from stabilization to self-sufficiency, one supported step at a time.
Finding a Partner for Your Recovery
Trying to navigate this path alone isn't just hard—it's unnecessary. The right treatment provider doesn’t just enroll you in a program; they become your partner and guide, helping you draw a personalized roadmap that adapts as you get stronger and your needs evolve. This partnership is built on trust, open communication, and one shared goal: your long-term well-being.
A truly comprehensive provider offers a connected continuum of care, not just a single, isolated service. At Altura Recovery, this means we’re with you at each transition, ensuring you see familiar faces and feel the consistency of a team that knows your story.
This isn't just about finding a program; it's about finding a clinical partner who listens, adapts, and is committed to helping you build a life of purpose and freedom.
This partnership becomes even more critical when you're facing co-occurring disorders. Juggling a substance use disorder alongside anxiety, depression, or trauma requires a truly integrated approach. Your treatment plan has to address both issues at the same time, with clinicians who get how they feed off each other.
A Personalized Path to Lasting Freedom
Your story is unique. Your recovery plan should be, too. The old one-size-fits-all model just doesn't cut it. Effective care is built around your specific history, challenges, and goals, combining key elements for success.
- Personalized Treatment Plans: Your care plan is a living document. It changes as you change, adapting to your progress and setbacks.
- Integrated Dual Diagnosis Care: You get specialized support for both substance use and mental health right from the start, because they are two sides of the same coin.
- Flexible Scheduling: With day, evening, and virtual options, treatment can actually fit into your life—not force you to abandon work, school, or family.
This flexible, person-first model is designed to remove the barriers that stop people from getting help. It empowers you to build real momentum and achieve genuine growth without having to blow up your daily responsibilities.
Choosing to ask for help is a huge act of courage. The next step is finding a team that can give you a professional assessment to figure out the right starting point. This isn’t about slotting you into a box; it’s about discovering the support system that will help you build a foundation for a life defined not by addiction, but by real healing and lasting freedom.
Got Questions? Let's Get You Some Answers
When you’re looking into addiction treatment, a lot of practical questions pop up. It’s completely normal. Figuring out how the right level of care gets chosen, how it’s paid for, and how it fits into your life can make the whole idea feel less overwhelming. Let’s walk through some of the most common questions with clear, straightforward answers.
How Is the Right Level of Care Determined for Me?
Finding your starting point isn’t a guessing game—it's a clinical process. The right level of care for you is figured out during a comprehensive assessment with an addiction professional. This isn't a test you can pass or fail; think of it more like an in-depth, confidential conversation about what's going on.
A clinician will look at several factors to get the full picture of your needs:
- The specific substances you've been using and for how long.
- Your current physical and mental health.
- Whether your home environment feels stable and supportive.
- Your experience with previous treatment attempts, if you've had any.
Using established guidelines, like the criteria from the American Society of Addiction Medicine (ASAM), they’ll recommend the setting that offers just the right amount of structure and support—enough to keep you safe and give you the best shot at success.
Will My Insurance Cover Different Levels of Treatment?
Yes, in most cases. The majority of major health insurance plans provide coverage for various levels of care, including medical detox, PHP, and IOP. That said, the specifics of what’s covered can vary quite a bit from one plan to another.
Key Takeaway: Coverage is common, but the details are what matter. Your plan's rules on co-pays, deductibles, whether you need pre-authorization, and the number of sessions they'll approve are crucial pieces of the puzzle.
The best first step is always to verify your benefits. Most treatment centers have dedicated admissions coordinators who are experts at this. They can call your insurance provider for you, clarify exactly what your plan covers, and help you understand any potential out-of-pocket costs. It’s a simple step that makes quality care much more accessible.
Can I Still Work or Go to School During Treatment?
Absolutely—and this is one of the biggest advantages of outpatient programs. Levels of care like IOP and SOP are designed specifically for people who need to balance their recovery with ongoing responsibilities like a job, school, or family commitments.
Flexible scheduling, including evening sessions and telehealth options, means you can weave treatment directly into your existing life instead of hitting pause on everything. This model is powerful because it lets you immediately apply the new coping skills you’re learning to real-world situations, reinforcing your progress day by day.
What if I Need to Change My Level of Care?
Moving between different levels of care is not just normal; it’s often a great sign of progress. Treatment isn't static because your needs aren't static. As you build new skills and find more stability, it’s natural that you’ll need less intensive support over time.
A good clinical team is constantly checking in on your progress. If you’re doing great in an IOP, they’ll work with you to create a plan to "step down" to a less structured SOP. On the flip side, if you hit a rough patch and need more support, you might temporarily "step up" from IOP to PHP. This dynamic approach makes sure you are always in the most effective setting for where you are in that moment.
At Altura Recovery, we know that every recovery journey looks a little different. Our team is here to help you find the right level of care to meet your specific needs and goals. You can learn more about our flexible outpatient programs by visiting us at https://www.alturarecovery.com.







