An intensive outpatient program (IOP) for substance abuse is a structured form of treatment that delivers a high level of clinical care without requiring you to live at a facility. It acts as a powerful middle ground, offering far more support than standard weekly therapy but with more real-world flexibility than residential treatment.
This setup allows you to balance your recovery with the demands of daily life.
A Bridge to Sustainable Recovery
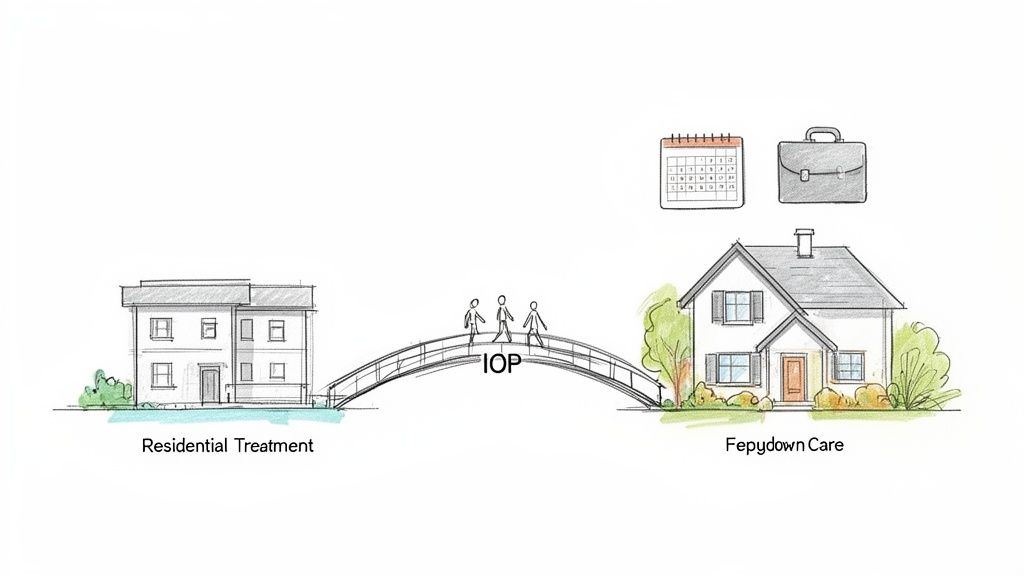
Think of recovery as a journey. On one side, you have the highly controlled environment of inpatient care. On the other, you have the complete independence—and the challenges—of your everyday world. An intensive outpatient program is the bridge that connects the two, giving you the support needed to cross from intensive treatment back into your community safely.
This model is a vital piece of the continuum of care, a framework designed to make sure you get the right level of support at the right time. An IOP accomplishes this by providing several hours of therapy and skill-building sessions multiple days a week, all while you continue to live at home.
Who Benefits Most from an IOP?
This flexible-yet-structured approach is a perfect fit in a few key situations. It creates a therapeutic container for growth and resilience without completely removing you from your real-world responsibilities.
- As a Step-Down: For those finishing a residential or inpatient program, an IOP is the ideal next step. It allows you to gradually reintegrate into daily life with a strong safety net still in place.
- As a Step-Up: Sometimes, weekly therapy just isn't enough. If you find yourself needing more structure and support, you can "step up" into an IOP for more focused and frequent care.
- For Those with Strong Support: People who have a stable, supportive home life and don't need 24/7 medical supervision can often thrive in an IOP setting right from the start.
The core purpose of an IOP is to equip you with the coping skills, emotional regulation techniques, and relapse prevention strategies needed to navigate life's challenges without turning to substances. It’s all about building a practical, real-world foundation for sobriety.
The sheer prevalence of this model highlights its effectiveness. As a cornerstone of outpatient care, IOPs have been a major part of the national treatment landscape for years. Back in 2011, for example, 44% of all addiction treatment facilities in the U.S. offered an intensive outpatient program, serving over 141,000 people. You can dig into these trends yourself in the annual census data on addiction facilities.
A Look Inside a Typical IOP Schedule
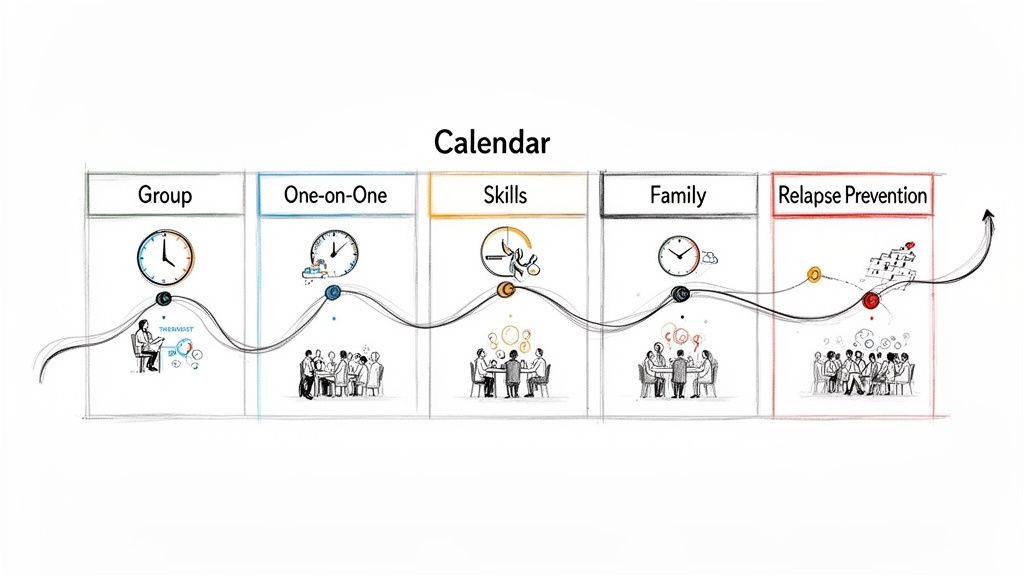
Stepping into an intensive outpatient program for substance abuse might feel like a huge commitment, but seeing how the schedule works can make it far less intimidating. The whole experience is built to be immersive yet flexible, giving you a powerful therapeutic structure that fits right into your existing life.
Most IOPs require a time commitment of 9 to 20 hours per week, usually spread across three to five days. This setup lets you keep up with work, school, or family obligations while getting the high level of clinical care you need. You get the structure that’s so critical in early recovery without having to press pause on your entire world.
The Weekly Rhythm
Imagine your week built around healing and growth. An IOP schedule isn't just one thing; it combines different therapeutic activities to tackle recovery from multiple angles. It’s not just about talking—it’s about learning new skills, practicing them in a safe space, and connecting with others who get it.
A standard week in an intensive outpatient program might look something like this:
- Group Therapy Sessions: These are the heart of the IOP experience and usually make up most of your weekly hours. This is where you connect with peers, share your struggles and wins, and build a real sense of community.
- Individual Counseling: You’ll get dedicated one-on-one time with a therapist each week to work through personal challenges, track your goals, and process things in a completely private setting.
- Family Therapy: Many programs bring family into the fold to help heal relationships, fix broken communication, and create a supportive home environment that helps sobriety stick.
- Skills-Building Workshops: These are practical, hands-on sessions that teach essential life skills, from managing stress and regulating emotions to setting healthy boundaries.
This blended approach makes sure you're building a strong internal foundation and a supportive external network at the same time.
A Sample Daily Structure
So, what does a single treatment day actually feel like? While every program is a bit different, a typical three-hour IOP session follows a clear format designed to keep you engaged and learning.
The goal is to create a predictable and safe environment where you can focus entirely on your recovery. Each part of the session builds on the last, reinforcing new skills and fostering deeper self-awareness.
For example, a morning or evening session could be broken down like this:
- Check-In and Goal Setting (30 minutes): The session kicks off with a group check-in. Everyone gets a chance to share current challenges, recent successes, and what they hope to get out of the day.
- Psychoeducational Group (60 minutes): A therapist leads a deep dive into a specific topic, like understanding addiction triggers, the neuroscience of recovery, or concrete relapse prevention techniques.
- Process Group or Skills Practice (90 minutes): This is where you put what you’ve learned into action. You might join a therapeutic process group to discuss personal issues or jump into a workshop to practice new coping skills through role-playing and other exercises.
This structure provides a powerful mix of education, peer support, and hands-on application. And increasingly, programs are offering these structured sessions online. To learn more, you can explore the benefits of telehealth mental health services and see how they make high-quality treatment more accessible than ever.
The Core Therapies That Drive Recovery
An intensive outpatient program isn't just about showing up; it’s about actively rewiring the thoughts, emotions, and behaviors that keep addiction running. This happens through a handful of powerful, evidence-based therapies. These aren’t abstract theories—they’re practical tools designed to help you build a new foundation for your life, one strong enough to handle real-world challenges.
The goal here is to move way beyond simply stopping substance use. We dig into the root causes, helping you understand why you turn to substances in the first place and equipping you with healthier ways to cope with stress, pain, and tough emotions. This is what creates lasting, sustainable change.
Changing Thoughts with Cognitive Behavioral Therapy
Cognitive Behavioral Therapy, or CBT, is a cornerstone of modern recovery for a reason. It’s built on a simple but game-changing idea: our thoughts, feelings, and behaviors are all tangled together. By learning to change negative and inaccurate thought patterns, we can directly change how we feel and what we do.
In an IOP, CBT helps you become a detective of your own mind. You learn to spot the automatic, destructive thoughts that trigger cravings or pave the road to relapse.
For instance, a thought like, "I had a terrible day at work, I deserve a drink," is a classic trigger. CBT teaches you to challenge that idea head-on. Is a drink really a reward, or is it just a temporary escape with serious consequences waiting on the other side? You learn to reframe that thought into something more honest and empowering, like, "I had a terrible day, so I’m going for a run to clear my head and actually feel better tomorrow."
This process involves:
- Identifying Triggers: Pinpointing the specific situations, people, or feelings that kickstart the urge to use.
- Challenging Distorted Thinking: Questioning and correcting the irrational beliefs you hold about yourself and your addiction.
- Developing Coping Skills: Learning practical, real-world strategies to manage cravings and navigate high-risk situations without turning to substances.
Managing Emotions with Dialectical Behavior Therapy
While CBT zooms in on your thoughts, Dialectical Behavior Therapy, or DBT, excels at helping you manage intense, overwhelming emotions. It was originally developed to treat borderline personality disorder, but its skills have proven incredibly effective for substance use disorders, which often go hand-in-hand with emotional chaos.
DBT gives you a toolbox of skills to help you ride out emotional storms without getting swept away. It teaches you how to accept difficult feelings for what they are while also working to change your response to them.
The core idea of DBT is balance—the "dialectic" between acceptance and change. It’s about accepting yourself and your current reality while simultaneously committing to building a better, healthier life.
Imagine feeling a massive wave of anger or shame. Instead of immediately reaching for something to numb it, DBT gives you other options. You might use a mindfulness technique to just observe the emotion without judgment, or a distress tolerance skill to get through that crisis moment safely. As you build these new coping mechanisms, using tools like habit tracking apps can be a huge help in reinforcing all the positive changes you're making.
Healing Wounds with Trauma-Informed Care
It's no secret that many people struggling with substance abuse also have a history of trauma. An effective intensive outpatient program for substance abuse has to recognize this link and build trauma-informed care into its very foundation. This approach makes sure the entire treatment environment feels safe, empowering you to address those underlying wounds without being re-traumatized.
Therapies like Eye Movement Desensitization and Reprocessing (EMDR) are often used to help the brain process traumatic memories that are stuck on a loop. By finally addressing these deep-seated issues, you can defuse the powerful emotional triggers that so often drive addiction. This focus on healing the root cause, not just slapping a bandage on the symptom, is absolutely essential for building a recovery that truly lasts.
How IOP Compares to Other Levels of Care
Choosing the right level of care for substance abuse is one of the most important decisions you'll make on the recovery journey. With options ranging from 24/7 residential facilities to weekly therapy sessions, understanding where an intensive outpatient program for substance abuse fits is key. This model occupies a crucial middle ground, offering a powerful blend of structure and real-world freedom.
Think of it like different types of medical support. Someone with a severe, acute illness needs the constant monitoring of a hospital (inpatient care). Someone with a chronic but stable condition might just need regular check-ups (standard outpatient). An IOP is like a specialized clinic you visit frequently for focused treatment while still living your life—it’s much more than a check-up but less than a full hospital stay.
This isn't about which option is "best," but about which one is the right fit for your specific needs at this point in your recovery.
Inpatient or Residential Treatment
This is the highest and most immersive level of care available. In an inpatient or residential program, you live at the treatment facility 24/7 for a set period—usually 30, 60, or 90 days, though sometimes longer. It's a completely controlled, substance-free environment designed for individuals who need constant medical supervision or are in a living situation that's unsafe or unsupportive of recovery.
The main difference from an IOP is the living arrangement. While inpatient care removes you from all external triggers and responsibilities, an IOP teaches you to manage those same triggers in real time. Inpatient is about stabilization and total immersion; IOP is about integration and applying skills in your actual life.
Partial Hospitalization Programs
A Partial Hospitalization Program, or PHP, is the level of care directly above an IOP. It’s often used as a step-down from residential treatment. A PHP offers a very high degree of structure, with clients attending treatment for about 20 to 30 hours per week—often five days a week for most of the day.
Like IOP participants, people in a PHP live at home. However, the time commitment is significantly greater, mirroring a full-time job. This makes PHP ideal for individuals who don't require 24/7 supervision but need more daily structure and clinical support than an IOP provides. In contrast, an IOP typically requires 9 to 20 hours per week, offering more flexibility to accommodate work or school schedules.
This diagram shows some of the core therapies that are foundational across different treatment levels, including IOP.
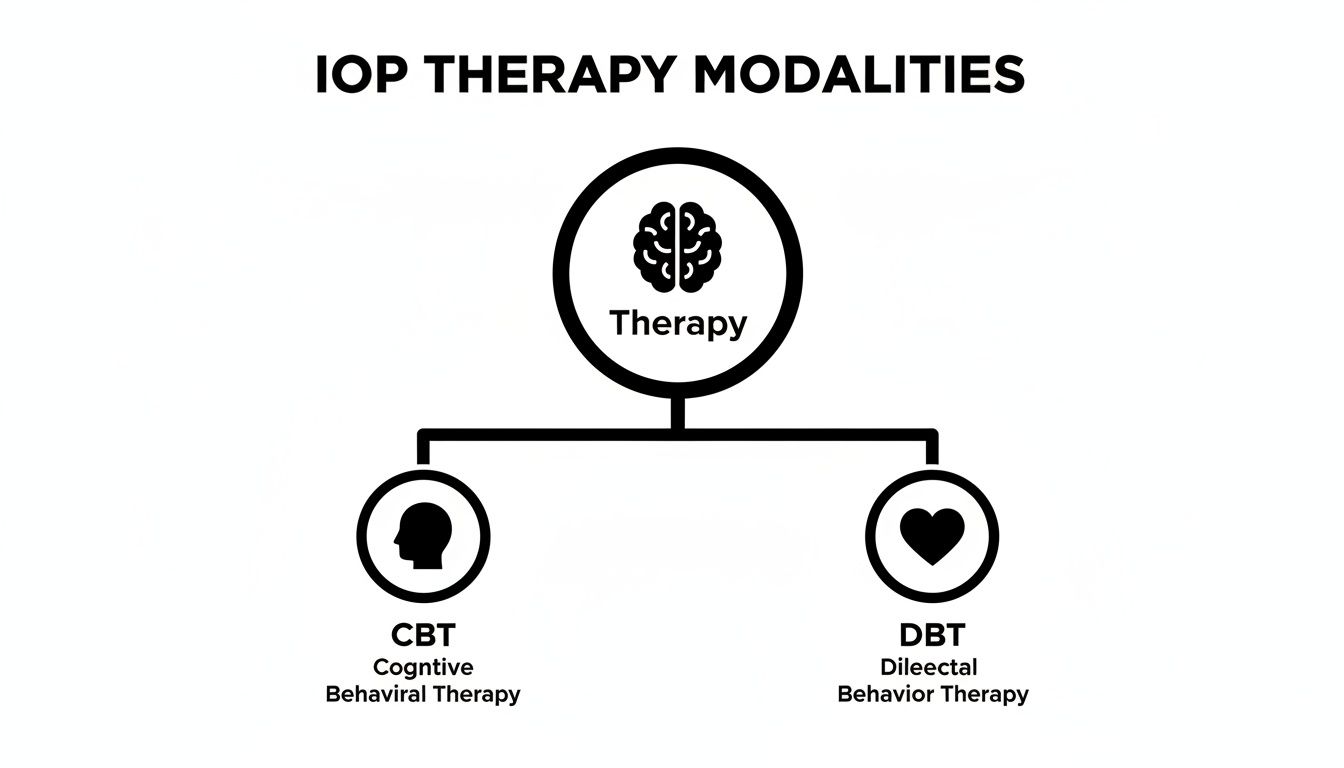
As you can see, central modalities like CBT and DBT are core to the therapeutic process within a well-structured intensive outpatient program.
Standard Outpatient and Aftercare
Standard outpatient treatment is the least intensive option on the spectrum. It usually involves just one or two therapy sessions per week, either individually or in a group setting. This level of care is best suited for individuals with a mild substance use disorder or as a step-down for someone who has already completed a more intensive program like an IOP or PHP.
An IOP provides a structured, supportive bridge between the high intensity of PHP or residential care and the relative autonomy of standard outpatient therapy. It is specifically designed to prevent a sudden drop-off in support that can often lead to relapse.
The key to a successful start in recovery is a careful assessment of your needs. The table below breaks down the key differences to help you see where an intensive outpatient program fits into the broader landscape of substance abuse treatment.
Addiction Treatment Levels: A Side-by-Side Comparison
This table compares the key features of different levels of substance abuse treatment to help you understand which option may be the best fit.
| Level of Care | Time Commitment | Living Arrangement | Ideal Candidate |
|---|---|---|---|
| Inpatient/Residential | 24/7, for 30-90+ days | Live at the facility | Needs medical stabilization; has an unsafe home environment. |
| Partial Hospitalization (PHP) | 20-30 hours/week (5-6 days) | Live at home or sober living | Needs significant daily structure but not 24/7 supervision. |
| Intensive Outpatient (IOP) | 9-20 hours/week (3-5 days) | Live at home or sober living | Ready to practice skills in real-world settings; needs flexibility. |
| Standard Outpatient (SOP) | 1-3 hours/week (1-2 days) | Live at home | Has mild SUD or is stepping down from a higher level of care. |
Ultimately, it’s all about finding the program that offers the right amount of support to help you build a strong, lasting foundation for recovery.
The Vital Role of Family in IOP Success
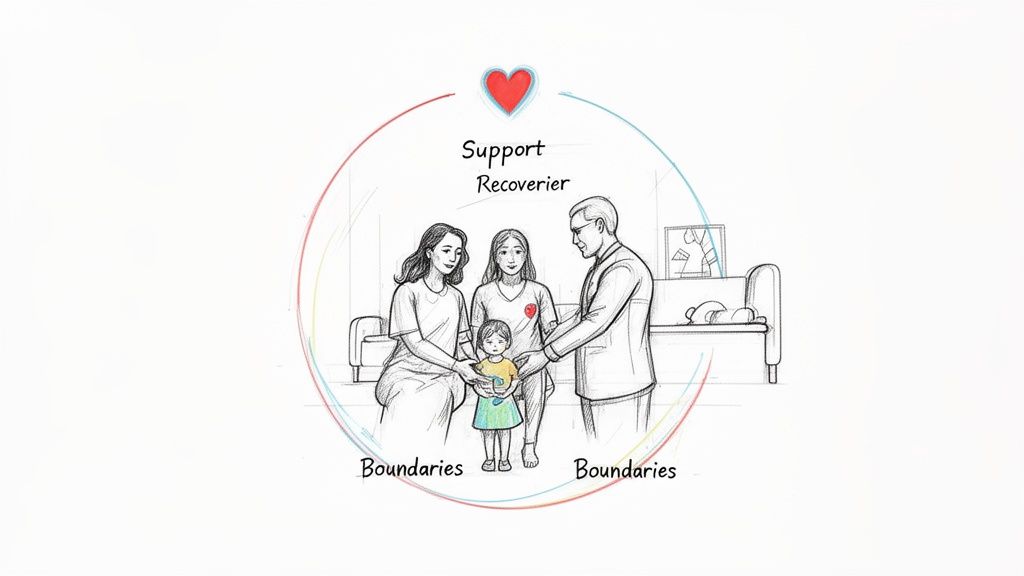
We tend to see recovery as a solo fight, but that's rarely the full picture. Addiction doesn’t just impact one person; it sends shockwaves through the entire family, twisting dynamics, shattering trust, and creating deeply ingrained patterns of dysfunction.
That’s why family involvement isn't just a nice add-on to an intensive outpatient program for substance abuse—it’s a cornerstone of lasting change.
When a loved one starts treatment, the whole family is stepping into a new chapter. Years of walking on eggshells, enabling behaviors, or constant conflict have likely taken a serious toll. Real healing means tackling these issues head-on, so the home can transform from a source of stress into a sanctuary of support. This is where family-focused care makes all the difference.
Rebuilding the Family System
A quality IOP knows that the family unit has to heal right alongside the individual. This isn’t about sending an occasional progress report. It means actively pulling family members into the recovery process with structured, therapeutic guidance.
The goal is to give everyone the tools they need to build a healthier dynamic. This often includes:
- Family Therapy Sessions: A trained clinician facilitates these meetings to help repair broken communication, rebuild trust, and give everyone a safe space to share their side of the story.
- Educational Workshops: Families learn the science of addiction, finally understanding it as a disease, not a moral failure. This knowledge is powerful, often replacing anger and blame with empathy and real-world support strategies.
- Communication Coaching: Loved ones learn how to express their needs and set boundaries in a way that’s supportive, not controlling. This is key to dismantling the codependent patterns that may have been fueling the addiction.
By treating the family as a whole, an intensive outpatient program gets to the root environmental factors that can either cement sobriety or tear it down. It’s about creating a shared recovery where everyone is moving forward, together.
Practical Steps for Family Members
If your loved one is in an IOP, your participation is one of the most powerful ways to show your support. It proves they aren't alone and that you're committed to building a better future with them. Being a true ally in their recovery means learning to balance support with self-care.
To make the most of this opportunity, family members should focus on a few key actions.
- Participate Actively: Show up for all offered family sessions and workshops. Your presence and willingness to learn and change are invaluable.
- Set Healthy Boundaries: Recovery is also about learning to say "no" to enabling behaviors. Setting clear, respectful boundaries protects your own well-being and supports your loved one’s journey toward autonomy.
- Practice Self-Care: You can't pour from an empty cup. The stress of loving someone through addiction is immense. Seeking your own support through therapy or groups like Al-Anon is absolutely crucial.
In the end, family involvement provides the missing piece that helps sustain progress long after the formal treatment program wraps up. It ensures the skills learned in an intensive outpatient program substance abuse are practiced and reinforced at home, creating a strong, resilient foundation for a lifetime of recovery.
Navigating Insurance and Costs for IOP
Let's talk about the financial side of things. Concerns about cost should never be a barrier to getting help, but we know the thought of paying for treatment can feel overwhelming. The good news is that an intensive outpatient program for substance abuse is often a much more financially accessible path to recovery than inpatient care.
We'll break down how insurance works, what key terms mean, and how you can get clarity on your specific plan so you can move forward with confidence.
One of the biggest advantages of IOP is its affordability. Because you live at home and continue with your daily responsibilities, you avoid the significant costs that come with 24/7 residential housing and supervision. It's a key reason why outpatient treatments are projected to hold the largest market share in the treatment industry by 2025—it’s an effective model that works for real life. You can explore more about these market trends in substance abuse treatment to see how care is evolving.
Your Insurance Is a Powerful Tool
Thanks to some landmark legislation, most health insurance plans are now required to provide solid coverage for mental health and substance use disorders. This has been a complete game-changer for people needing quality care.
Two key laws protect your right to treatment:
- The Affordable Care Act (ACA): This law classifies mental and behavioral health services as essential health benefits. That means most marketplace and employer-sponsored plans have to cover them, just like they cover a broken arm or a heart condition.
- The Mental Health Parity and Addiction Equity Act (MHPAEA): This act is just as important. It requires insurance companies to make sure their coverage for mental health and substance use disorders is no more restrictive than their coverage for medical or surgical care. They can't create unfair hurdles.
These protections mean your insurance plan can't just ignore your need for IOP care. Your policy is a vital asset on your recovery journey.
How to Verify Your Benefits
Understanding your specific coverage is the first step. While it might seem complicated, any good treatment center’s admissions team can handle this process for you from start to finish. Still, knowing the key terms will empower you to understand the conversation.
Here are the essentials you'll hear about:
- Verification of Benefits (VOB): This is simply the process where our admissions team contacts your insurance provider to confirm exactly what your plan covers for an intensive outpatient program.
- Deductible: Think of this as the amount you must pay out-of-pocket for covered health services before your insurance plan starts chipping in.
- Copayment (Copay): This is a fixed, flat amount you pay for a covered service once you've met your deductible. For example, you might have a $30 copay for each therapy session.
- Coinsurance: This is your share of the costs, expressed as a percentage. If your coinsurance is 20%, you pay 20% of the bill after your deductible is met, and the insurance company pays the other 80%.
Don’t let these terms intimidate you. A compassionate admissions coordinator, like the team here at Altura Recovery, can walk you through every detail. We'll explain your financial responsibility in plain English and work to maximize your benefits, ensuring there are no surprises down the road.
Working with an experienced team makes this process simple. They will verify your insurance, translate your coverage into a clear financial plan, and handle the paperwork. This lets you focus on what truly matters—your healing and recovery—without being overwhelmed by the financial details. The path to recovery is more accessible than you might think.
Common Questions About IOPs
Stepping into an intensive outpatient program for substance abuse is a big decision, and it’s completely normal to have questions swirling around. Getting clear, straightforward answers is the best way to feel confident you're making the right choice. Here, we’ll tackle some of the most common things people ask, hopefully clearing up the confusion so you can see the path forward.
From how long it takes to what life looks like after, knowing these details can make the whole idea of recovery feel a lot more real and less overwhelming. Our goal is to give you the clarity you need to take that next step.
How Long Does an IOP Typically Last?
This is probably the number one question we get, and the honest answer is: it really depends on you. There’s no magic number or one-size-fits-all timeline for recovery. That said, most intensive outpatient programs run for about 8 to 12 weeks. Some people might move through it a bit faster, while others benefit from taking a little more time to really lock in their new skills.
Your clinical team will work with you to figure out the right duration based on a few key things:
- How you’re progressing toward your personal treatment goals.
- The severity of the substance use disorder.
- Whether you’re also managing any co-occurring mental health conditions.
- Your level of engagement and active participation in therapy.
The focus is always on quality, not speed. The program is designed to wrap up when you’ve built a strong enough foundation to confidently step down to a less intensive level of care, like weekly therapy, without putting your sobriety at risk.
Can I Still Work or Go to School During an IOP?
Absolutely. In fact, this flexibility is one of the biggest benefits of the IOP model. These programs are built to fit into your life, not pull you out of it. Most centers, including Altura Recovery, offer both daytime and evening sessions to work around all kinds of schedules.
This setup is powerful because it lets you immediately apply the coping skills you learn in therapy to real-world challenges at your job, in class, or at home. It’s like practicing recovery in real time, all while keeping up with the responsibilities that matter to you.
What Happens After I Graduate from the Program?
Finishing an intensive outpatient program for substance abuse is a huge accomplishment, but it isn't the final chapter of your recovery story. A good program will never just send you on your way without a solid plan. Graduation is all about creating a detailed aftercare or "step-down" plan to make sure you have support for the long haul.
This continuing care plan usually involves a few key pieces:
- Transitioning to Standard Outpatient Therapy: This typically means moving to weekly individual or group therapy sessions to keep the momentum going.
- Joining Support Groups: Getting active in community-based groups like Alcoholics Anonymous (AA), Narcotics Anonymous (NA), or SMART Recovery can provide incredible fellowship and accountability.
- Alumni Programs: Staying connected with your treatment center and the peers who graduated alongside you creates a powerful, lasting support network.
Finding the right support system is a huge part of long-term success. If you're looking at different options, our guide to finding addiction recovery programs near me can help you figure out how to build a strong local network. The whole point is to create a sustainable lifestyle in recovery, and aftercare is the framework that helps you do just that.