The first step in figuring out how to detox from alcohol is to understand it's a serious medical process. This isn't a test of willpower or something you can just white-knuckle through on your own. Because withdrawal can be life-threatening, the only safe and effective approach involves professional medical supervision. Period.
Why Medical Supervision Is Not Negotiable
When you drink heavily for a long time, your brain's chemistry literally changes to adapt. Alcohol is a depressant, so to keep things balanced, your brain ramps up its own stimulating activity. When you suddenly cut off the alcohol, your brain stays in that overstimulated state, triggering what’s known as alcohol withdrawal syndrome (AWS).
This is much more than a bad hangover—it's a full-blown physiological crisis. Symptoms can escalate shockingly fast, going from tremors and anxiety to life-threatening conditions like seizures or delirium tremens (DTs). DTs are a severe state of confusion and agitation that carries a very real risk of death.
Differentiating Heavy Drinking From Alcohol Dependence
Not everyone who drinks a lot will have severe withdrawal, but it's critical to know the line between heavy use and physical dependence. Dependence isn't about how much you drink; it's about developing a tolerance and experiencing withdrawal symptoms when you stop.
You might be physically dependent if you experience things like:
- Morning Tremors: Waking up with shaking hands or "the shakes."
- Anxiety and Irritability: Feeling agitated or on edge until you have that first drink.
- Insomnia: You can't sleep properly unless you've been drinking.
- Physical Symptoms: Nausea, sweating, or a racing heart when the alcohol wears off.
These aren't just annoying side effects. They are clear signals that your body now requires alcohol to function normally. If this sounds familiar, you can learn more by exploring the common warning signs of alcohol addiction in our detailed guide.
This is a massive global issue. An estimated 400 million adults live with alcohol use disorders worldwide, and about 209 million of them experience physical dependence. Yet, only a tiny fraction—around 7.2%—get the treatment they need. That treatment gap contributes to 2.6 million deaths every single year.
Understanding Your Detox Options
The right detox setting depends entirely on the severity of your dependence and your overall health. It's also worth noting how alcohol significantly impairs sleep quality, which often makes withdrawal even harder to manage and professional support that much more vital.
Choosing the right environment is the single most important decision you'll make at this stage. It really does set the foundation for a safe and successful recovery.
Key Takeaway: Trying to detox from alcohol alone is like trying to navigate a minefield blindfolded. The risks are severe, unpredictable, and entirely preventable with the right professional guidance.
To help you understand the levels of care available, here's a look at the different settings where a medically supervised detox can happen.
Comparing Alcohol Detoxification Settings
This table breaks down the primary settings for alcohol detox. It's designed to help you see which option might be the best fit based on your level of dependence and medical needs.
| Detox Setting | Best For | Level of Supervision | Key Features |
|---|---|---|---|
| Inpatient Hospital | Individuals with severe, long-term dependence, co-occurring medical conditions, or a history of delirium tremens. | 24/7 medical monitoring by doctors and nurses. | Access to emergency medical care, intensive monitoring of vital signs, and immediate intervention for severe complications. |
| Residential Detox Center | Those with moderate to severe dependence who are medically stable but need a structured, supportive environment away from triggers. | 24/7 clinical and emotional support from medical staff and counselors. | A non-hospital setting focused on comfort, with structured therapy, peer support, and medical management of withdrawal symptoms. |
| Outpatient Detox | Individuals with mild to moderate dependence, a strong support system at home, and no history of severe withdrawal symptoms. | Regular check-ins with a medical team (daily or several times a week). | Allows the individual to live at home while receiving medication management, counseling, and medical supervision on a scheduled basis. |
As you can see, there's a level of care designed for every situation. The most important thing is to be honest about your needs and choose the setting that gives you the highest chance of detoxing safely and comfortably.
The Reality of Alcohol Withdrawal Syndrome

When you abruptly stop drinking after a long period of heavy use, your body doesn't just feel bad—it enters a state of shock. This isn't just a brutal hangover. It's a complex and dangerous medical condition known as Alcohol Withdrawal Syndrome (AWS).
It all starts in the brain. After being suppressed by alcohol for so long, your central nervous system has been working in overdrive just to keep you awake and alert. Take the alcohol away, and your brain stays stuck in that hyper-excited state. That’s what unleashes the storm of withdrawal symptoms, turning what seems like a simple decision to quit into a physiological crisis that demands careful, expert navigation.
What feels deeply unsettling one moment can become life-threatening the next with frightening speed.
What Happens in the First 72 Hours
While the intensity is different for everyone, the timeline for AWS is fairly predictable. Understanding this progression is critical, not just for managing discomfort but for knowing when it's time to get immediate medical help.
The first few hours after that last drink are usually just the calm before the storm.
6-12 Hours: The first signs begin to creep in. You might feel a gnawing anxiety, become irritable, or find it impossible to sit still. Physical symptoms like a racing heart, profuse sweating, and the classic hand tremors—"the shakes"—are common. For most people, this is when the urge to have another drink becomes almost unbearable, if only to make it all stop.
12-24 Hours: Things get more intense. On top of the tremors and anxiety, some people start to experience alcoholic hallucinosis. This is when you see, hear, or even feel things that aren't there. People often describe seeing insects crawling on the walls or hearing faint, menacing voices. While absolutely terrifying, this is different from the much more severe delirium tremens.
24-48 Hours: This is the peak window for withdrawal seizures. These aren't subtle; they're generalized tonic-clonic seizures, and they can happen even if you have no history of epilepsy. Having just one seizure dramatically increases your risk of having more, which makes this a make-or-break period for medical supervision.
Crucial Insight: The withdrawal timeline isn't just a list of symptoms; it's a ladder of escalating risk. What starts with a slight tremor can quickly progress to a full-blown seizure. This is exactly why trying to detox from alcohol at home, without medical support, is playing with fire.
This whole physical ordeal is deeply tied to what's happening in your mind. To get a better handle on this, it helps to understand the key differences between physical vs. psychological dependence. Knowing this helps explain why both parts of you—body and mind—need to be treated during detox.
Delirium Tremens: The Most Severe Stage
The most feared complication of AWS is delirium tremens, or the DTs. It’s a full-blown medical emergency that strikes about 5% of people going through alcohol withdrawal and carries a high risk of death if it isn't treated in a hospital. The DTs usually show up 48-72 hours after the last drink, but in some cases, they can be delayed for up to a week.
Unlike the earlier symptoms, the DTs involve a profound and global state of confusion. A person experiencing them may not know their own name, where they are, or what year it is. This severe mental break is coupled with extreme physical symptoms.
Warning Signs of Delirium Tremens:
- Extreme agitation, sometimes leading to aggression
- Severe confusion and total disorientation
- Vivid, terrifying hallucinations
- Soaking sweats and a dangerously high fever
- Sky-high blood pressure and a racing, erratic heart rate
Someone in this condition isn't just sick; they are critically ill. Their body is losing the ability to regulate its most basic functions—breathing, temperature, and heart rate. This is precisely why a medically supervised detox facility is the only safe place to manage severe alcohol withdrawal.
The broader health impact of chronic alcohol misuse is staggering. It's a contributing factor in over 230 different diseases, from liver failure and cancer to severe cardiovascular conditions. Every year, alcohol abuse is behind up to 3 million deaths worldwide, which is more than 5% of all deaths. You can dig deeper into these numbers in the latest World Health Organization report.
Navigating a Medically Supervised Detox
The idea of checking into a facility for a medically supervised detox can feel pretty overwhelming. It's completely normal to be anxious about what’s going to happen. But every single part of this process is built around one goal: keeping you safe and as comfortable as possible while your body begins to heal.
When you first arrive, the immediate next step is a thorough assessment. This is way more than just filling out forms; it's a deep dive into your specific situation. A clinical team will go over your medical history, ask about your drinking patterns, and get a clear picture of your current physical and mental health. This initial evaluation is absolutely crucial because it’s the blueprint for a detox plan made just for you.
The Role of Medication in Safe Withdrawal
One of the most critical tools for a safe detox is the use of medication to manage withdrawal symptoms. Trying to figure out how to detox from alcohol on your own, without this support, is precisely what makes it so dangerous. For severe alcohol withdrawal, the primary medications used are typically benzodiazepines.
These aren't pills you can just manage by yourself; they demand strict medical supervision. The clinical team administers them on a carefully controlled schedule to help calm your overstimulated nervous system. This is what prevents the most dangerous withdrawal symptoms, like seizures and delirium tremens, from ever taking hold.
Here's what you can generally expect from this part of the process:
- Symptom-Triggered Therapy: Medication isn't just handed out on a rigid schedule. Nurses will be constantly assessing your withdrawal symptoms and giving you medication as needed to keep you stable and comfortable.
- Gradual Tapering: As your body starts to stabilize over a few days, the dosage of these medications is slowly and carefully reduced. This gentle tapering process lets your brain chemistry readjust without the jolt of a sudden stop.
- 24/7 Monitoring: Your vital signs—like heart rate, blood pressure, and temperature—are monitored around the clock. This ensures you remain stable and allows the team to catch any potential complications long before they become serious problems.
Expert Insight: Medication-assisted treatment (MAT) is considered the gold standard for managing severe alcohol withdrawal. It dramatically increases safety, reduces the worst symptoms, and gives you a stable foundation to start the real psychological work of recovery.
Unfortunately, getting access to this kind of care is still a major hurdle for many. In the United States, only 2.4% of the estimated 27.1 million adults with a past-year alcohol use disorder actually received medication-assisted treatment. To get a better handle on this highly effective approach, you can read our guide on what medication-assisted treatment is and how it works.
Essential Supportive Care During Detox
Medication is a huge piece of the puzzle, but it’s not the whole thing. A quality detox program also provides comprehensive supportive care to address the toll that heavy drinking has taken on your entire body. This holistic support is what makes the process not just survivable, but truly effective.
Think of your body as a system that's been running on the wrong kind of fuel for a long time. It’s depleted, dehydrated, and completely out of balance. Supportive care is all about restoring that balance.
This often includes:
- IV Fluids and Hydration: Chronic alcohol use causes severe dehydration and throws your electrolytes way out of whack. Intravenous (IV) fluids are often used to quickly rehydrate your body and replenish essential minerals like potassium and magnesium, which are vital for proper heart and nerve function.
- Nutritional Therapy: Many people who come into detox are seriously malnourished. You'll get a diet packed with vitamins and nutrients—especially B vitamins like thiamine—which are essential for healing your brain and nerves. Expect balanced meals and supplements designed to help your body repair itself.
- A Calm and Secure Environment: A professional detox center offers a quiet, trigger-free space where your only job is to heal. This removes you from the stresses and temptations of your home environment, giving you the peace you need to rest and recover without distraction.
The Substance Abuse and Mental Health Services Administration (SAMHSA) provides a National Helpline for individuals and families facing mental and/or substance use disorders.
This screenshot shows the confidential, free, 24/7 support available, underscoring that professional help is always within reach. The key insight here is the emphasis on immediate, accessible support, which is the first step toward finding a reputable facility for a safe detox.
Building Your Support System for Lasting Sobriety

Making it through the physical gauntlet of alcohol detox is a massive win. Seriously, take a moment and feel proud of that. But it's the starting line, not the finish. The real journey—building a life where sobriety sticks—begins right now.
Lasting sobriety is rarely a solo mission. It’s built on a solid foundation of psychological and social support that helps you handle life’s curveballs without reaching for a drink. This next phase is all about healing your mind, rewiring old habits, and surrounding yourself with people who have your back. Without that structure, it's incredibly easy to slide back into old patterns.
Finding the Right Therapeutic Fit
Professional therapy is a non-negotiable part of long-term recovery for most people. It’s a completely safe and confidential space to dig into the why behind your drinking, learn new ways to cope with stress, and start healing from underlying issues like trauma or anxiety.
One of the most effective tools in the therapist's toolbox is Cognitive Behavioral Therapy (CBT). It’s a very practical, hands-on approach that helps you pinpoint the negative thoughts and behaviors that fueled your drinking. For example, your therapist might help you see the connection between social anxiety and your urge to drink, then work with you to build real-world skills to manage that anxiety in healthier ways.
Other powerful therapies include:
- Dialectical Behavior Therapy (DBT): Fantastic for learning how to manage intense emotions and improve relationships.
- Eye Movement Desensitization and Reprocessing (EMDR): A specialized therapy that is incredibly effective for processing past trauma that might be tangled up with substance use.
The Power of Peer Support Groups
There is something uniquely powerful about connecting with people who just get it. Peer support groups offer a sense of community and shared experience that you can't find anywhere else. They’re a living reminder that you are not alone in this fight.
You've got options, each with a slightly different flavor:
- Alcoholics Anonymous (AA): As the most well-known program, AA is a 12-step fellowship that has helped millions find and maintain sobriety.
- SMART Recovery: This is a secular, science-backed alternative that uses tools from CBT to help you manage your thoughts, feelings, and behaviors.
- Women for Sobriety or LifeRing Secular Recovery: These are other great alternatives that provide different frameworks for building a fulfilling, sober life.
Walking into your first meeting can feel intimidating, but the non-judgmental support and sense of belonging you find there can become a true lifeline. It’s one of the few places you can be completely honest without fearing shame.
Rebuilding Connections with Family and Loved Ones
Addiction doesn't just affect one person; it sends ripples through the entire family. As you begin to heal, it’s crucial to start rebuilding trust and learning new, healthier ways to communicate with the people you love. This takes patience, honesty, and a willingness to set firm boundaries.
For instance, you might need to tell your friends you can't meet at the bar anymore, suggesting a coffee shop or a walk in the park instead. These boundaries aren't about pushing people away. They're about protecting your sobriety so you can show up as the best, healthiest version of yourself. When your family is ready to heal together, our guide on family therapy for substance abuse offers practical steps for mending those vital connections.
Nourishing Your Body and Mind After Detox
Chronic alcohol use robs your body of essential nutrients and throws your physical health out of whack. A huge part of your new support system is actively caring for your physical well-being. This creates a positive feedback loop: when your body feels better, your mind becomes clearer and more resilient.
Start with simple but powerful habits. Focus on a balanced diet packed with whole foods to restore those depleted vitamins and minerals. As you work on building a healthier lifestyle, supporting your gut health with things like natural prebiotics and probiotics can make a significant difference in your overall well-being.
Regular physical activity is another game-changer. Exercise releases endorphins, which are natural mood-boosters that also help dial down stress. You don't have to crush it at the gym, either. A daily walk, a bike ride, or a yoga class can work wonders for managing cravings and improving your mental state. When you combine these physical habits with your therapeutic and social supports, you create a holistic and incredibly strong framework for a sober life.
Creating Your Relapse Prevention Plan
Getting through alcohol detox is a huge win. Seriously. It's the moment you break the physical hold alcohol has on you. But the work doesn't stop there. Now comes the part that's just as critical: building a life that actually supports staying sober for the long haul. This is where a relapse prevention plan comes in—it’s your personal roadmap for navigating recovery.
A solid plan isn’t just a list of things not to do. It’s a proactive strategy for creating a life so fulfilling that alcohol becomes irrelevant. You design it yourself, loading it with tools, resources, and people who have your back when things get tough. Think of it as the scaffolding that holds everything together while you rebuild.
This infographic gives a great visual snapshot of the core pieces you'll want to include.
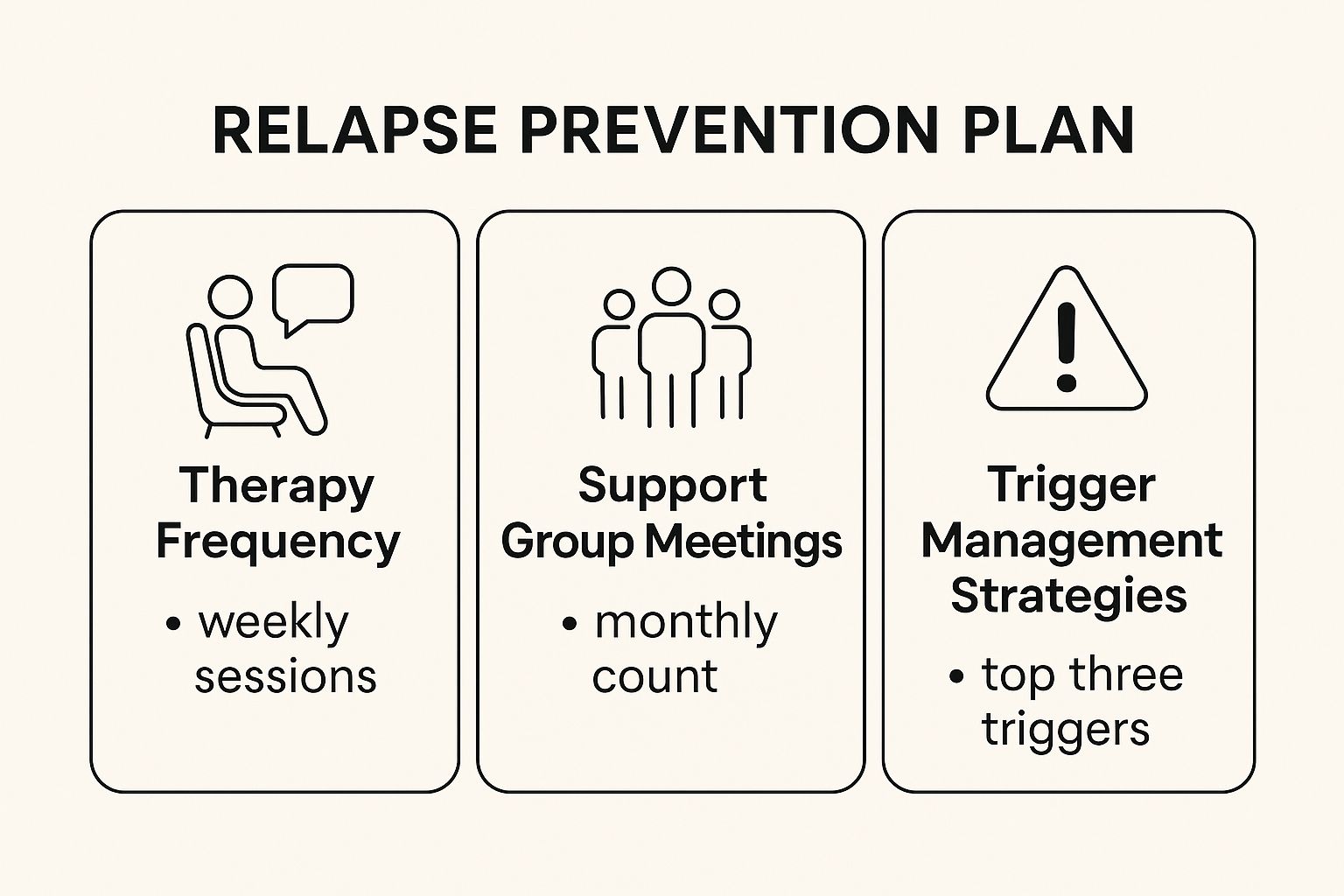
As you can see, it’s not just one thing. It's the combination of consistent therapy, active support groups, and smart trigger management that creates a powerful safety net for your sobriety.
Identify Your Personal Triggers
First things first, you have to become a detective in your own life. Triggers are the specific people, places, feelings, or situations that spark that urge to drink. Getting brutally honest about what yours are is fundamental to learning how to detox from alcohol and make it stick.
Triggers are unique to everyone and can be surprisingly subtle.
- Emotional Triggers: This could be stress after a brutal day at work, the quiet loneliness of a weekend, or even just plain boredom.
- Social Triggers: Maybe it’s seeing old drinking buddies, going to a wedding where the champagne is flowing, or even just driving past your old go-to bar.
- Environmental Triggers: Simple cues in your surroundings can be powerful. It could be the clock hitting 5 p.m., the specific chair you always drank in, or the sound of a bottle opening on TV.
Take the time to actually write these down. The more specific you get, the better you can prepare. Self-awareness is your first line of defense.
Develop Healthy Coping Strategies
Once you know what sets you off, you need a new toolkit of healthy responses to pull from instead of reaching for a drink. Cravings feel overwhelming, but they are temporary. Having a go-to plan to ride out those few intense minutes changes everything.
For instance, if you know work stress is a big one for you, your coping plan might be a mandatory 15-minute walk the second you log off. Or maybe it’s calling a supportive friend to vent. If holiday parties feel like a minefield, you can decide ahead of time to bring your own non-alcoholic drinks and have an exit strategy ready to go.
Key Takeaway: A relapse prevention plan shifts you from reacting to cravings to proactively managing them. Instead of being caught off guard, you have a pre-planned, healthy action to take. It puts you back in the driver's seat.
A few strategies that work for many people include:
- Mindfulness and Meditation: Apps like Calm or Headspace are great for learning how to observe a craving without having to act on it.
- Physical Activity: Even a quick burst of exercise can release feel-good endorphins and totally short-circuit a stress response.
- Creative Outlets: Getting lost in a hobby—playing guitar, painting, or trying a new recipe—is a fantastic way to distract yourself and get a real sense of accomplishment.
Build Your Recovery Circle
Recovery doesn't happen in a vacuum. Your plan must include people. Sobriety thrives in community, not in isolation. This means making ongoing therapy a non-negotiable, consistently showing up for support group meetings, and having a short list of people you can call when you’re having a rough time.
A well-rounded plan will have multiple layers of support. Here's a table outlining the key components to build into your own strategy.
| Key Components of a Relapse Prevention Plan |
| :— | :— | :— |
| Component | Actionable Steps | Why It's Important |
| Trigger Identification | List specific people, places, feelings, and times that cause cravings. | Awareness is the first step. You can't avoid or manage what you don't acknowledge. |
| Healthy Coping Skills | Create a "menu" of activities: exercise, meditation, hobbies, calling a friend. | Replaces the unhealthy habit of drinking with constructive actions that relieve stress. |
| Support Network | Schedule therapy, attend meetings (AA, SMART Recovery), and list emergency contacts. | Provides professional guidance, peer understanding, and immediate help during a crisis. |
| Lifestyle Changes | Plan sober social activities, improve nutrition, and establish a consistent sleep routine. | Creates a new life where sobriety is enjoyable and sustainable, not just a struggle. |
| Emergency Plan | Write down "if-then" steps for a slip (e.g., "If I drink, I will call my sponsor immediately"). | Turns a potential relapse into a learning opportunity and prevents a single mistake from spiraling. |
This isn't just a checklist; it's a framework for building resilience.
Beyond formal support, think about reconnecting with hobbies you dropped, whether that’s joining a hiking group, a book club, or a local sports league. These activities do more than just fill time—they connect you with new people who share your interests, not your old habits. This powerful mix of professional help, peer support, and genuine fun is what a strong, lasting recovery is built on.
Common Questions About Alcohol Detox
When you're considering detox, the big picture can feel overwhelming. It helps to break it down into the practical, day-to-day questions that pop up. Getting straight answers builds confidence and helps you prepare for what’s really involved in getting sober safely.
Let's tackle some of the most pressing concerns people have.
The most intense, physical part of alcohol withdrawal usually lasts between five to seven days. Symptoms tend to show up within hours of the last drink, hit their peak around the 24 to 72-hour mark, and then start to fade. That said, some things like trouble sleeping or a lingering sense of anxiety can stick around for a few weeks.
Can You Ever Detox at Home?
This is a big one, and the answer needs to be crystal clear. When clinicians talk about "outpatient detox," they are referring to a medically supervised process for people with mild dependence and a rock-solid, sober support system at home. This is completely different from trying to quit "cold turkey" on your own.
Going it alone without professional oversight is never a safe bet. The risks of severe withdrawal, including seizures or delirium tremens, are just too unpredictable and dangerous.
A true, professionally managed outpatient detox always includes:
- Regular check-ins with a medical team, often daily at the start.
- Prescriptions for medications that manage withdrawal symptoms and keep you safe.
- A clear, pre-arranged emergency plan in case complications pop up.
This route only works if you have a stable, trigger-free home and you're fully committed to the process. For anyone with a history of heavy, long-term drinking or who has had a rough withdrawal experience before, an inpatient facility is the only safe place to start.
The non-negotiable element here is medical supervision. Whether it's inpatient or outpatient, a safe detox is always guided by healthcare professionals who can step in immediately if things get complicated. Attempting to manage it yourself is a serious gamble with your health.
What to Expect with Costs and Insurance
The cost of alcohol detox can vary quite a bit, depending on the level of care (inpatient is generally more expensive than outpatient), the facility’s location, and how long you need support. The good news is that most private and employer-based health insurance plans cover treatment for substance use disorder, including detox, because it's considered an essential health benefit.
Your first step should be to call your insurance provider directly to verify your coverage. You'll want to ask about specific numbers—your deductible, co-pays, and which facilities are in your network to avoid surprise bills. Most treatment centers have admissions staff who are experts at this and can help you sort through the financial side of things.
How to Support a Loved One Through Detox
Supporting someone in detox is a tricky balance of showing compassion while holding firm boundaries. Your job isn't to be their nurse or their counselor, but to be a steady source of encouragement.
Here are a few practical ways you can help:
- Learn About Withdrawal: Take some time to read up on alcohol withdrawal syndrome. Understanding what they're physically and emotionally going through makes a world of difference.
- Handle Practical Things: Offer to help with real-world logistics, like driving them to the facility, feeding their pet, or making sure their bills are paid. This frees them up to focus entirely on getting well.
- Just Listen: Be a safe person they can talk to without fear of judgment. Let them share their fears and frustrations.
- Get Involved in Family Programs: Many treatment centers offer workshops or family therapy sessions. Showing up demonstrates that you're all in on their recovery journey.
Your support can be a powerful force for their recovery, but don't forget to look after your own mental and emotional health during this stressful time.
At Altura Recovery, we understand that every recovery journey is unique. Our evidence-based outpatient programs provide the expert medical care and compassionate support needed to build a sustainable foundation for sobriety while you maintain your daily life. If you're ready to take the next step, visit us at https://www.alturarecovery.com to learn how we can help.








