When you love someone who struggles with anger, your first instinct is to try and fix it. But here’s a truth that took me years to learn: their anger is not your problem to solve. Your role is to be a supportive ally, not a therapist, and a huge part of that is knowing how to keep yourself safe.
Trying to manage someone else’s anger for them is a quick way to burn out and damage your relationship. The real goal is to create a stable, supportive space where they feel safe enough to choose help for themselves.
This guide is built on that foundation of empathy mixed with firm self-preservation. You can support their journey, but you can’t walk it for them. Getting that distinction clear in your own head is the most important first step you can take.
Core Principles for Effective Support
Before we get into specific techniques, we need to talk about mindset. How you approach this will determine whether you calm a situation down or accidentally pour fuel on the fire. Keeping these core principles front and center will help you navigate the toughest moments.
Think of these principles as your compass. They guide your actions in a heated argument just as much as they do during a calm, quiet conversation. They shift your focus away from trying to control their behavior to influencing the environment and protecting your own well-being. This isn’t about giving up; it’s about engaging in a way that’s healthier and more sustainable for everyone involved.
Supporting someone with anger isn’t about absorbing their rage; it’s about modeling calm, enforcing boundaries, and creating a space where they feel safe enough to address their own issues.
Let’s quickly break down the foundational mindset you’ll need. Keeping these ideas in mind is critical for offering support that is both safe and genuinely effective.
Table: Core Principles for Effective Support
| Principle | Why It's Essential | Your First Step |
|---|---|---|
| Safety First | Your physical and emotional safety is non-negotiable. You can't help someone if you're in harm's way. | Identify your personal safety limits and create an exit plan for volatile situations before they happen. |
| Empathy, Not Agreement | Validating their feelings ("I can see you're frustrated") is different from condoning their actions or words. | Practice reflective listening by acknowledging their emotion without judging the behavior attached to it. |
| Maintain Boundaries | Clear boundaries protect your mental health and communicate what behavior is unacceptable to you. | Clearly state your limits during a calm moment, such as, "I cannot continue this conversation if you are yelling." |
| You Are Not Responsible | You cannot control their emotions or choices. Their anger is their responsibility to manage. | Let go of the need to "fix" them. Instead, focus on offering support for the choices they make. |
Internalizing these principles will make every other strategy in this guide far more effective. They give you a solid foundation to stand on, ensuring you can offer help from a place of strength and safety, not fear or obligation.
Navigating an Angry Outburst Safely
When you're face-to-face with someone's anger, your first job isn't to solve the problem that caused it. It's to bring the emotional temperature down and make sure everyone is safe. Going beyond the generic advice to "stay calm" means learning a few specific, in-the-moment techniques that can defuse the tension.
The goal is simple: reduce any sense of threat. An angry brain is essentially in a fight-or-flight state, making it hyper-sensitive to triggers. Your body language and tone of voice can either fuel the fire or start to put it out before you've even said a word.
Mastering Your Non-Verbal Cues
Your physical presence is your first tool. Small, unconscious signals can easily be read as aggression, so you need to consciously adopt a neutral, non-threatening posture.
- Maintain a Safe Distance: Give them physical space. Standing too close can feel confrontational, making them feel cornered and escalating the situation.
- Keep Your Hands Visible and Relaxed: Avoid crossing your arms, clenching your fists, or putting your hands on your hips—all classic signs of defensiveness or aggression. Instead, keep your arms uncrossed with your palms open and relaxed to signal you're not a threat.
- Lower Your Voice and Slow Your Speech: Speak in a low, slow, and even tone. A calm voice can be contagious, subconsciously nudging the other person to match your emotional state. Whatever you do, don't raise your voice, even if they're yelling.
This approach subtly shifts the dynamic. You're no longer in a confrontation; you're just a calm presence in a shared space, ready to listen instead of fighting back. It shows respect for their emotional state without validating any destructive behavior.
Using Reflective Listening to Validate Feelings
During an outburst, the person often feels completely unheard or misunderstood. Reflective listening is an incredibly powerful tool for showing them you're trying to understand, validating their feelings without necessarily agreeing with their actions.
Let's say your partner is yelling about unexpected bills and accusing you of being irresponsible with money. Your instinct might be to jump into defense mode. Don't.
Scenario:
- Their Outburst: "I can't believe this! Another surprise bill! You never think about our budget, and now we're in this mess!"
- Defensive Response (What to Avoid): "That's not fair! I'm not the only one who spends money!"
- Reflective Response (What to Use): "I can hear how stressed and overwhelmed you are about our finances right now. It sounds like this bill was a complete shock."
Notice how the second response doesn't accept blame. It simply acknowledges the core emotion behind the anger—stress and fear. This can instantly lower their defenses because it shows you're on the same team, trying to understand what they're feeling.
The flowchart below gives you a simple decision tree for choosing the right approach, whether you're in the middle of an outburst or talking during a calm moment.
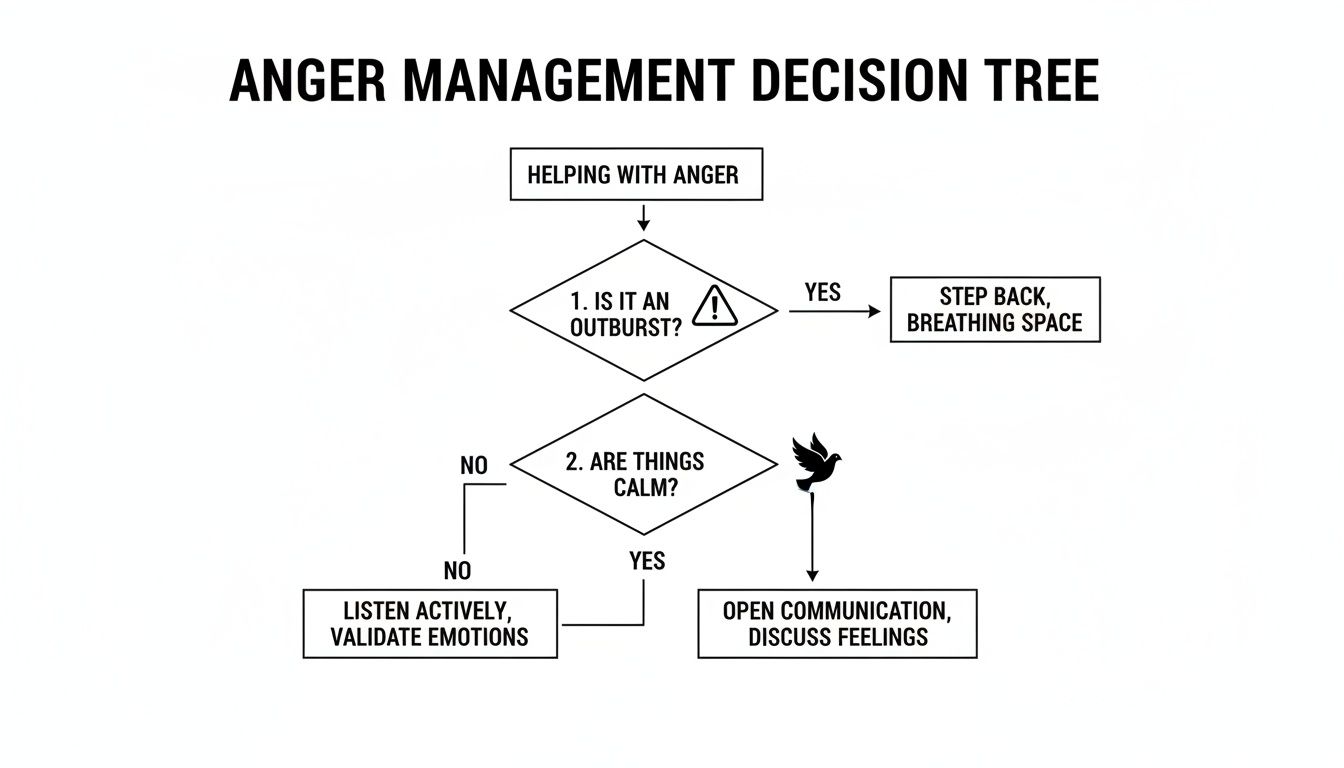
This visual guide drives home a critical point: your strategy has to adapt. De-escalating a crisis is a totally different skill from having a constructive conversation when things are stable.
Knowing When to Disengage for Safety
Your safety is the absolute priority. De-escalation techniques are effective, but they aren't magic. You have to be able to recognize when a situation is tipping into dangerous territory and have a plan to get yourself out.
Your responsibility is to offer support, not to absorb abuse or place yourself in harm's way. Having a safety plan isn't a sign of failure; it's a critical act of self-preservation that enables you to continue offering support in the future.
Trust your gut. If the anger twists into threats, property destruction, or physical intimidation, it's time to leave.
Warning Signs That Require Disengagement:
- Threats of physical harm—to you, themselves, or anyone else.
- Blocking your exit or physically cornering you.
- Throwing, breaking, or punching objects.
- Any history of physical violence during past arguments.
It's best to create a safety plan before an outburst happens. This could mean identifying a safe room in the house, having a friend on standby to call, or agreeing on a simple phrase you'll use to end the conversation, like, "I need to take a break from this now." This kind of preparation lets you act decisively when you feel unsafe, instead of freezing in the heat of the moment.
Communicating Constructively During Calm Moments
The moments right after an outburst are fragile, but it's the quiet days in between where the real work gets done. This is your window to build a foundation for lasting change through constructive communication. It’s a chance to share how you feel and set boundaries without the immediate pressure of an escalating situation.
These conversations aren't about pointing fingers or replaying old arguments. Instead, the goal is to build a shared understanding of what makes the environment feel unsafe and what you both need to feel respected. Think of it as proactive work that can chip away at the frequency and intensity of future blow-ups.
Timing Your Conversation Is Everything
Choosing the right moment for these talks is half the battle. Bringing up heavy topics when someone is tired, stressed from work, or distracted is a surefire way to trigger defensiveness. You have to find a time when you’re both relaxed, rested, and can give the conversation your full attention.
This could be a quiet weekend morning over coffee or a specific time you both agree to set aside. The key is creating a neutral, non-confrontational atmosphere. By intentionally picking a calm moment, you're sending a clear signal: "I want to solve this with you, not attack you."
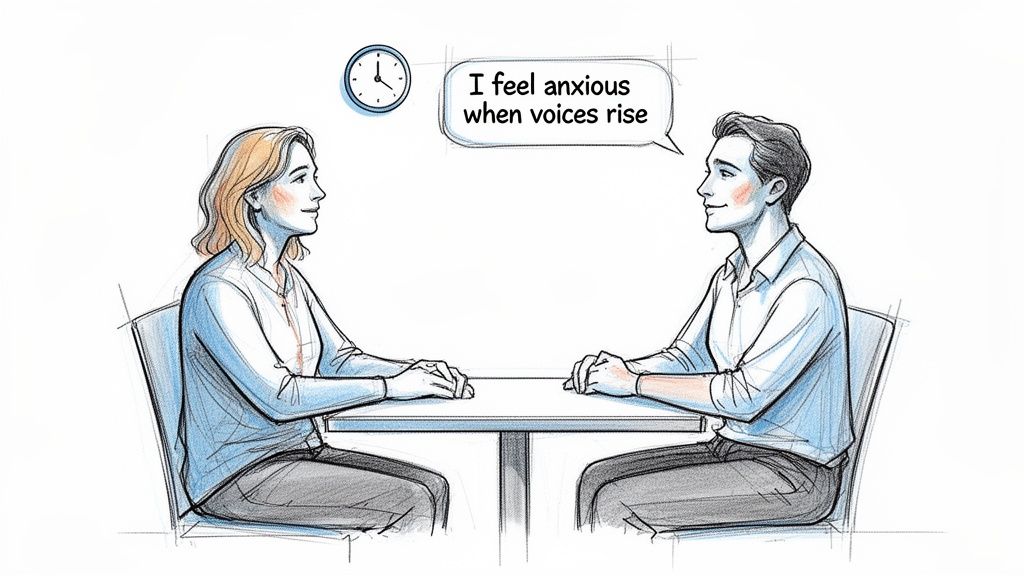
Using "I" Statements to Share Your Experience
One of the most powerful tools in your communication kit is the "I" statement. It lets you express your feelings without making accusatory "you" statements, which almost always put the other person on the defensive. It frames the issue around your experience—which is undeniable—rather than their behavior, which they might try to dispute.
It’s a simple shift in language that can completely change the tone of the conversation.
- Instead of saying: "You always yell, and it’s terrifying." (This is an accusation).
- Try saying: "I feel scared and anxious when voices are raised in our home." (This expresses your feeling).
This isn't about being passive; it's about being clear and strategic. It opens the door for empathy because you’re sharing your vulnerability instead of pointing a finger. The focus moves from their "bad" behavior to its impact on the relationship.
Learning how to stop arguing in relationships can provide additional frameworks for these crucial conversations, helping you foster connection over conflict.
Setting and Respectfully Upholding Boundaries
Boundaries aren’t punishments; they are the rules of engagement you set for your own well-being. When you're supporting someone with anger issues, clear boundaries are non-negotiable for protecting your emotional and physical safety. These limits need to be communicated clearly and firmly during a quiet moment, not shouted in the heat of an argument.
A well-defined boundary is about what you will do, not what you will force them to do. It puts the control over your own safety back in your hands.
A boundary isn't a wall you build to keep people out; it's a line you draw to define what behavior you will accept in your space. It's an act of self-respect that teaches others how to treat you.
Here are a few practical examples of what setting a verbal boundary looks like:
- Boundary on Communication: "I love you and I want to resolve this, but I can't continue the conversation if there's yelling. If that starts, I will calmly leave the room to give us both space."
- Boundary on Language: "It’s really important to me that we speak to each other with respect. I will have to end our talk if name-calling or insults are used."
- Boundary on Physical Space: "When things get intense, I feel overwhelmed and need some space. If I say I need a moment, please respect that, and we can try talking again in 20 minutes."
The most critical part? You have to follow through. A boundary that isn't enforced is just a suggestion. Consistently and calmly upholding your limits shows you are serious about protecting yourself, which is a vital part of helping someone manage anger for the long haul.
Encouraging Professional Anger Management Support
Guiding someone you care about toward professional help for their anger is easily one of the most powerful—and delicate—steps you can take. It’s a conversation that demands a careful mix of empathy, strategy, and timing. The goal isn't to force them through a door, but to gently show them it’s there.
How you approach this conversation can make all the difference. It can either feel like an accusation or an act of genuine care. Forget saying, "You need to fix your anger." Instead, frame it as a shared concern for their well-being and for your relationship. This positions seeking help as a sign of profound strength, not weakness.
Broaching the Subject with Care
Finding the right words to suggest therapy can feel like walking on eggshells. The key is to lead with vulnerability and focus on how the anger impacts you and them, not on judging the person. This conversation must happen during a calm moment, when defenses are down and you're both able to listen.
Use "I" statements to share how you feel. Instead of, "Your outbursts are completely out of control," try something like, "I feel so worried for you when you seem overwhelmed by anger, and I want us to find a way through this together."
Talking about professional help should feel like a collaborative effort to improve their life, not a judgment on their character. The message is, "We're a team, and this is a challenge we can face with the right support."
Before you even start the conversation, do a little research. Being able to gently explain what anger management therapy actually involves can strip away much of the fear and stigma. It shows you're invested in finding a solution, not just pointing out a problem.
Demystifying Effective Anger Management Therapy
A lot of people think anger management is just about counting to ten or punching a pillow. The reality is that modern, evidence-based therapies are far more sophisticated and effective. They give people practical skills to understand and manage their emotional responses at the root.
Two of the heavy hitters in this field are Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT).
- Cognitive Behavioral Therapy (CBT): This is really the foundation of modern anger management. It works on a simple principle: our thoughts, feelings, and actions are all linked. CBT helps people pinpoint the automatic negative thought patterns that trigger anger and teaches them how to challenge and reframe those thoughts before they escalate into an outburst.
- Dialectical Behavior Therapy (DBT): Originally developed for other conditions, DBT has proven incredibly useful for anger. It focuses on building skills in four key areas: mindfulness (staying present), distress tolerance (handling painful emotions without making things worse), emotion regulation (managing intense feelings), and interpersonal effectiveness (communicating needs respectfully).
These therapies aren't about bottling up anger. They're about understanding where it comes from and finding healthier ways to deal with it. The skills learned are practical tools for life, not just temporary fixes.
The Power of Evidence-Based Treatment
The effectiveness of these approaches is backed by solid research. For example, helping someone with anger issues through Cognitive Behavioral Therapy (CBT) has shown remarkable success. Meta-analyses reveal a 23% reduction in general recidivism risk and a 28% reduction in violent recidivism risk for people in CBT-informed anger management programs.
For those who completed the full treatment, the results were even more profound: a 42% risk reduction for general recidivism and a stunning 56% for violent recidivism. You can dig into the detailed findings on the effectiveness of CBT-informed anger management to see just how significant the impact can be.
Finding the Right Treatment Format
Professional support isn't a one-size-fits-all deal. There are different levels of care available, which means treatment can be woven into someone's life without causing a massive disruption. Knowing these options can make the idea of getting help feel much less overwhelming.
Different Levels of Care:
- Individual Therapy: One-on-one sessions with a therapist offer a private, focused space to dig into the underlying causes of anger. This is often the first step.
- Group Therapy: Small group sessions create a powerful sense of community. Hearing from others with similar struggles can dismantle feelings of shame and isolation, and it provides a safe space to practice new communication skills.
- Intensive Outpatient Programs (IOP): For someone who needs more than a weekly session, an IOP offers structured therapy for several hours a day, a few days a week. This allows the person to keep up with work, school, or family life while getting substantial therapeutic support. At programs like Altura Recovery, an IOP provides a robust framework that includes individual counseling, group sessions, and skills training to build a strong foundation for managing anger and any co-occurring issues.
- Partial Hospitalization Programs (PHP): This is a more immersive level of care, with treatment for most of the day, five days a week, while the person still lives at home. It’s a great fit for individuals who need a high level of support to stabilize their emotions and behaviors.
By laying out these varied options, you can show your loved one that "getting help" can be adapted to their life. It reframes the process from a scary, all-or-nothing commitment to a flexible, step-by-step journey toward feeling better. Your role is simply to plant the seed, offer the information with compassion, and be there to support them if they decide to take that brave first step.
Prioritizing Your Own Well-Being and Boundaries
When you're constantly focused on helping someone else navigate their anger, it's incredibly easy to let your own needs fall by the wayside. But supporting someone through their emotional struggles is exhausting work. If you aren't careful, you can quickly find yourself emotionally depleted, anxious, or even resentful.
Putting your own well-being first isn’t selfish; it’s a non-negotiable part of providing stable, sustainable support. Think of it this way: you can't pour from an empty cup. Once your mental and emotional reserves are gone, you lose the patience and clarity needed to de-escalate a tense situation or have a productive conversation. Self-care is your primary tool for building resilience.
Protecting Your Own Mental Health
You have to actively protect your mental health. This means carving out dedicated space for your own emotional processing, completely separate from the person you’re trying to support. You need an outlet to vent, get perspective, and simply recharge.
Here are a few practical ways to do that:
- Find Your Own Therapist: Speaking with a professional gives you a confidential space to explore your own feelings and develop coping strategies without judgment.
- Join a Support Group: Connecting with others in similar situations is validating in a way nothing else is. Groups like Al-Anon or other family support programs create a community that truly gets it.
- Reconnect with Hobbies: Make a real effort to schedule activities that bring you joy and remind you of who you are outside of this supporter role. It could be anything from hiking to painting to just getting lost in a good book.
- Lean on Your Social Network: Don't let yourself become isolated. Make regular time for trusted friends and family who can offer a listening ear or a much-needed reality check.
Your well-being is not a luxury—it is the foundation upon which effective, long-term support is built. Neglecting it doesn't help your loved one; it only increases the likelihood of burnout for you.
The Mechanics of Setting Healthy Boundaries
Let's be clear: boundaries are not about controlling the other person's behavior. They are about defining what you will and will not accept to protect your own peace and safety. They’re a calm, clear expression of your limits.
Learning how to set healthy boundaries is absolutely essential for protecting your emotional space and preventing burnout. The key is to communicate these limits kindly but firmly, and always during a moment of calm—not in the heat of an argument.
Practical Examples of Boundaries
Think of boundaries as the guardrails that keep your relationship on a safe road. To be effective, they have to be specific, communicated ahead of time, and consistently enforced. Here’s what this can look like in the real world:
Communication Boundaries
- "I want to hear what you have to say, but I won't participate in a conversation that involves shouting or insults. If that starts, I'm going to step away until we can both speak calmly."
Personal Space Boundaries
- "When I feel overwhelmed by the tension, I need to take some space for myself. I’ll go to another room for about 30 minutes, and we can try talking again after that."
Behavioral Boundaries
- "I will not tolerate things being thrown or broken in our home. If that happens, I will leave the house for my own safety until you've calmed down."
Enforcing these boundaries is the hardest part, especially at first. You might face resistance or pushback. But consistently holding these lines is how you teach others how you expect to be treated and create a safer emotional environment for everyone. It's a powerful act of self-respect.
Common Questions About Anger Issues
When you're trying to figure out how to support someone with anger issues, a lot of specific, thorny questions come up. The advice is rarely one-size-fits-all, and what helps in one situation might backfire in another. Let's tackle some of the most common and complex questions people face, so you can navigate these challenging moments with more clarity.
These questions get right to the heart of the confusion and frustration you’re likely feeling. Getting clear on them can reinforce the strategies we've discussed and give you more confidence in your approach, whether you're setting a boundary or suggesting they talk to a professional.
Is Their Anger My Fault?
It’s a natural question, especially when the anger is pointed directly at you. But the answer is a clear, resounding no.
While your actions might trigger their outburst, the disproportionate or destructive reaction is a reflection of their own internal struggles with emotional regulation. It is not a measure of your behavior.
Think of it like this: spilling a glass of water on someone might be annoying (the trigger), but if that person responds by flipping the table over, their reaction is about much more than the spilled water. Their inability to manage that initial flash of frustration is the core issue. Accepting that you are not responsible for their emotional state is a critical step in protecting your own mental health.
Can Anger Be a Symptom of Something Else?
Absolutely. Chronic anger and irritability are often just the tip of the iceberg, signaling a deeper issue that hasn't been addressed. It's almost never just about a "bad temper."
Several conditions can show up as anger:
- Depression: Many people, especially men, don't experience depression as sadness. Instead, it manifests as persistent irritability and anger.
- Anxiety: When someone feels constantly on edge or overwhelmed, their fight-or-flight response is already dialed up, making them prone to angry outbursts over minor stressors.
- Trauma or PTSD: Unresolved trauma can leave a person in a state of hypervigilance, where even a perceived threat can trigger an intense, aggressive response.
- Substance Use Issues: Alcohol and certain drugs lower inhibitions and impair judgment, a combination that often leads to increased aggression and anger.
- Medical Conditions: In some cases, issues like traumatic brain injuries, hormonal imbalances, or chronic pain can cause significant mood changes, including heightened irritability.
Recognizing that anger might just be a signpost for a deeper problem can shift your perspective from frustration to compassion. It also highlights why it’s so important to encourage them to get a professional evaluation to find the root cause.
Does Anger Management Therapy Actually Work?
This is a crucial question, and the data is incredibly hopeful. Yes, evidence-based anger management programs are highly effective. The myth that people with anger issues can't change is just that—a myth.
The goal of anger management isn't to get rid of anger, which is a normal human emotion. It's about teaching people how to spot their triggers, manage the physical rush, and express their feelings in a healthy, non-destructive way.
Research consistently shows positive outcomes. In fact, large-scale analyses confirm that 75% of people who participate in anger management therapy show significant improvement. Effective programs, often lasting 8 to 12 weeks, successfully reduce hostile outbursts and the tendency to ruminate on negative thoughts. You can dig into the details in this 2022 systematic review on anger management effectiveness. This high success rate proves that with the right tools and commitment, real change is entirely possible.
What If They Refuse to Get Help?
This is one of the toughest and most painful situations you can face. You've offered support, tried to communicate constructively, and gently suggested professional help, but they flat-out refuse. You cannot force an adult to go to therapy.
At this point, your focus has to pivot entirely to your own well-being and the boundaries you need to enforce for your own safety.
Here’s what that looks like in practice:
- Reinforce Your Boundaries: Consistently enforce the limits you've set. If you said you would leave the room during yelling, do it. Every single time.
- Protect Yourself: Prioritize your emotional and physical safety above all else. This might mean creating more distance in the relationship or, in some cases, deciding you can no longer be in it.
- Seek Your Own Support: This is the time to lean heavily on your own therapist, a support group, or trusted friends. You need a safe space to process your own feelings of helplessness, sadness, and frustration.
Sometimes, the most powerful motivator for someone to change is finally experiencing the natural consequences of their actions. When you stop shielding them from the impact of their anger by upholding your boundaries, they may finally see the need to get help for themselves.
Navigating these challenges is incredibly difficult, but you don't have to do it alone. If you or your loved one are struggling, professional outpatient programs can provide the structured support needed for lasting change. At Altura Recovery, we offer evidence-based therapies and personalized care plans that address anger, addiction, and co-occurring mental health conditions, helping individuals build the skills for a healthier future. Learn more about our approach at https://www.alturarecovery.com.