High-functioning alcoholism refers to people who meet the clinical criteria for alcohol use disorder yet keep their jobs, handle family duties, and show up for social events without missing a beat. They often rely on well-rehearsed habits and polished routines, which can hide a growing dependence in plain sight.
Beneath that smooth exterior, alcohol’s hold quietly tightens. Recognizing hidden patterns is your first real move toward change.
What Defines a High Functioning Alcoholic
On paper, a high-functioning alcoholic looks like success—meeting deadlines, leading meetings, juggling kids’ schedules. Yet after clocking out, the same person might head home and pour glass after glass, believing they’ve got everything under control.
Take Sarah, for instance. She’s a marketing manager in her early thirties who nails every project by day but pours wine each evening in a ritual that felt harmless at first. That split life—professional confidence paired with private drinking—can cloak a serious disorder.

Below are the main points you’ll explore:
- Why spotting hidden alcoholism matters
- What you’ll learn in each chapter
- How outward success can mask urgent need for help
- The first steps toward recovery
High-functioning alcoholics (HFAs) account for about 20% of those with AUD, or roughly 6.5 million adults over a 12-month period. Learn more about these findings on PMC.
Recognizing Hidden Patterns
Imagine an iceberg: the visible tip is only a fraction of what’s beneath the waterline. That’s how hidden cravings often behave—most of the struggle remains out of sight.
In Sarah’s case, colleagues lauded her dependability while never spotting the vodka bottle tucked into her tote. Outward success can easily mask an internal crisis.
“Success on the surface can hide a serious struggle beneath.”
Why This Guide Matters
Every chapter builds on the last, guiding you from simple awareness to practical action. You’ll follow Sarah’s story to see how routine resilience can give way to genuine recovery.
Here’s what you’ll find next:
- Clinical Signs and Common Myths
- Risks and Progression
- Co-Occurring Disorders and Diagnosis
- Outpatient Treatment Options and Therapies
- Practical Steps With Altura Recovery Model
By the end of this section, you’ll spot hidden cues in yourself or a loved one and feel inspired to dive into clinical insights and recovery strategies.
How Routine Feels Safe
Rituals can cradle us in a false sense of control. For Sarah, grabbing a glass of wine the moment she walked in the door felt as natural as hanging up her coat.
Yet those small daily choices chip away at tolerance and coping skills, setting the stage for serious health risks down the road.
Early awareness can prevent progression from hidden habit to full-blown disorder.
Armed with this understanding, you’re ready to dig into clinical signs and debunk myths around the high-functioning alcoholic label. In the next chapter, we’ll compare real warning signs with common misconceptions so you can spot trouble early and seek help confidently. Let’s begin this journey together.
Clinical Signs And Common Myths

Most people picture a high-functioning alcoholic as someone who only sips champagne at parties. In truth, subtle patterns and midday rituals can hide deeper cravings and mounting tolerance.
Imagine an iceberg: the visible tip is an evening drink, but below the surface lies a vast mass of secret sips and unspoken urges. That hidden half is where trouble often brews.
Tom, a project lead, became a master of disguise. He tucked a small pour of whiskey into his coffee mug during meetings, then aced every deadline with a smile.
“Most of what you’re dealing with lies beneath what people see.”
Yet when stability is mistaken for safety, real warning signs slip through the cracks. Let’s unpack how genuine red flags differ from comforting myths.
Clinical Signs Versus Common Myths
To see the problem clearly, line up the true indicators of high-functioning alcoholism against the stories that let it stay hidden.
| Clinical Signs | Common Myths |
|---|---|
| Secret daytime drinks | Only evening social drinking |
| Increasing tolerance | Stable drinking patterns |
| Mood swings after a few sips | Unwavering emotional balance |
| Concealing cravings | No evidence of dependence |
By comparing facts side by side, you can break through the myths that mask risk.
Recognizing Subtle Cues
Spotting hidden alcoholism means paying attention to small shifts in behavior. These early signals often go unnoticed until they intensify.
- Frequent mood fluctuations
Iritability or low energy soon after a discreet drink can be a warning flag. - Excuses for quick drink breaks
Dismissing a sip as “stress relief” often hides dependence. - Hiding empty bottles or cans
Stashing evidence signals growing anxiety around drinking.
“Surface stability rarely reflects true stability.”
You might be interested in exploring how self-defeating habits can fuel hidden drinking patterns. Learn more in our article on self-defeating behaviors.
Iceberg Metaphor In Action
Think of that iceberg again:
- The visible tip—an after-work glass—draws all the attention
- Below the waterline, secret rituals and internal scripts steer each craving
- Underneath, silent anxiety gnaws at the surface until patterns become impossible to ignore
This simple analogy reveals how most of the struggle stays out of sight—until it’s almost too late.
Key Takeaways
- Covert sipping points to deeper issues
- Rising tolerance marks progression
- Popular myths can blind you to real warning signs
- Early recognition opens the door to timely support
Risks And Progression Of High Functioning Alcoholic
Living a thriving career and family life can feel like armor. Yet, those nightly “harmless” drinks sneak in slowly—like a time-lapse of erosion, they chip away at our health.
Consider a single drop of water wearing down rock over years. That’s exactly how modest, repeated binges undermine our bodies without obvious warning.
For instance, David began with two glasses of wine most evenings. Five years later, his routine quietly pushed his liver enzymes into the danger zone before a routine checkup caught it.
Early Signs Of Damage
Those first warning lights are easy to ignore. A creeping fatigue or mild belly discomfort often seems unrelated.
Spotting subtle clues early, though, can mean the difference between a brief detour and a full-blown crisis.
- Liver Disease: gradual fat buildup and inflammation
- Cardiovascular Events: hypertension, arrhythmias, heart attack
- Cancers: mouth, throat, liver and breast
- Accidental Injuries: impaired coordination causes falls and accidents
Neurological changes also creep in. You might notice forgetfulness or mood swings long before dependence takes hold.
“Small habits over time become the story of our health,” notes Dr. Elena Morris, a hepatology specialist.
According to the World Health Organization, about 800,000 deaths each year in the European Region are tied to alcohol. Learn more about alcohol use impact here.
Progression From Hidden Use To Health Crisis
What starts as secret sips often snowballs into a health spiral. Take Maria, a sales executive who bumped weekend drinks from two to six. By year three, she endured irregular heart rhythms and an emergency fainting spell.
| Stage | Typical Habits | Potential Outcome |
|---|---|---|
| Early Use | 2–3 drinks nightly | Mild liver inflammation |
| Mid Progression | Added midweek drinking | High blood pressure |
| Advanced Stage | Daily heavy consumption | Cirrhosis or heart attack |
Recognizing your phase on this timeline can prompt timely intervention—and even reverse damage in early stages.
- Reduce daily intake by 25% and track with a journal or an app
- Schedule a medical evaluation for liver and cardiac markers
- Join a peer support group or consider IOP at Altura Recovery
Catching the trajectory now can save more than $20,000 in medical costs over a decade. Even cutting back by one drink daily may reduce liver fat by up to 40% within six months.
In the next section, we’ll explore co-occurring disorders like anxiety and depression and how they shape the path to diagnosis and recovery.
Co Occurring Disorders And Diagnosis
High-functioning drinkers often juggle a demanding career, a social life, and secret struggles with alcohol. At the same time, mood issues—like anxiety, depression, or unresolved trauma—can act as hidden currents, quietly pushing someone toward that next drink.
Think of each condition as a layer in a cake: one slice might taste smooth and consistent until you slice deeper and discover unexpected flavors. Skipping over underlying anxiety or depression is like patching a leaky dam without finding the crack—it won’t hold for long.
Consider Laura, a busy graphic designer who met every deadline but only by pairing late-night work sessions with a glass of wine—then two, then three. What looked like simple perfectionism turned out to be a classic case of AUD tangled up with GAD. A focused screening finally revealed the true connection.
During intake, clinicians ask about sleep patterns, energy levels, social routines, and drinking frequency. Layer by layer, these questions uncover overlapping symptoms. They also dive into personal history, family risk factors, and any co-occurring medical issues. In about 20 minutes, a skilled clinician can spot the red flags and suggest more in-depth testing.
Screening For Dual Diagnoses
Structured assessments help untangle symptoms so no disorder slips through the cracks.
- PHQ-9 screens for depression severity and tracks mood over time.
- GAD-7 evaluates generalized anxiety symptoms across seven targeted questions.
- AUDIT flags hazardous drinking patterns and potential dependence.
- SCID delivers a full psychiatric interview covering multiple diagnoses in one protocol.
| Tool | Purpose | Duration |
|---|---|---|
| PHQ-9 | Depression screening | ~5 minutes |
| GAD-7 | Anxiety assessment | ~5 minutes |
| AUDIT | Alcohol use evaluation | ~10 minutes |
| SCID | Full diagnostic review | ~45 minutes |
A case interview often opens with broad, conversational questions before you tally scores. Once the data is in, results guide a treatment plan that addresses both alcohol use and mental health needs. But remember: screening alone won’t untangle deep-seated co-occurring patterns. Moving on to a diagnosis means weaving together tool results with clinical judgment and each client’s unique history—creating a truly integrated roadmap to recovery.
Why Treating Both Disorders Matters
Addressing anxiety or depression alongside alcohol use dramatically increases the odds of lasting recovery. An integrated approach digs into root causes rather than slapping on separate band-aids.
- Improves emotional regulation by tackling mood swings and cravings together
- Reduces relapse risk through coordinated therapy sessions blending coping skills
- Enhances medication matching for psychiatric symptoms and alcohol dependence
- Fosters peer support networks that understand both social anxiety and drinking triggers
Integrated care reduces treatment gaps and boosts engagement.
Global estimates show about 1% of the world’s population has an AUD, with men accounting for roughly three-quarters of those affected—proof that hidden high-functioning alcoholism crosses borders wherever drinking is common. Discover more insights about global alcoholism rates on WorldPopulationReview.com
If you suspect you or a loved one may have a co-occurring disorder, don’t wait. Reach out for a professional evaluation today.
Check out our guide to medication management for mental health to learn how Altura clinicians support dual-diagnosis prescribing.
Integrated care models weave therapy, medication review, and peer coaching into one program. This unified path offers a clear route out of hidden drinking and untreated mental health layers. Next, we’ll explore outpatient options that wrap care around your daily responsibilities.
Next Steps For Integrated Care
Begin by booking a dual-diagnosis assessment with a licensed clinician.
- Prepare intake details: current medications, symptom history, and drinking patterns.
- Attend screening sessions at Altura Recovery to review assessment results and set personal goals.
- Collaborate on a combined care plan that fits your work, family, and treatment needs.
Taking these steps ensures you harness integrated care to overcome hidden challenges—and move toward genuine, lasting recovery.
Outpatient Treatment Options And Therapies
Stepping back from work or family duties can feel like an impossible choice for a high-functioning alcoholic. Outpatient programs weave recovery into your daily routine, so you can keep moving forward without pausing life.
Standard Outpatient Program
Standard Outpatient Programs (SOP) typically meet 1–3 times weekly over 6–12 weeks. Sessions blend relapse-prevention strategies, practical life skills, and peer support.
- Session Frequency: 1–3 meetings a week with a licensed clinician
- Group Size: Intimate gatherings of 6–10 peers sharing real-world tips
- Focus Areas: Stress management, coping techniques, and education
For example, Mark juggled his career as a corporate attorney with evening SOP meetings. Within eight weeks, he cut his alcohol intake by 50%, using those sessions as a safety net for lasting change.
Intensive Outpatient Program
When you need more structure, Intensive Outpatient Programs (IOP) deliver 9–15 hours of therapy per week. They combine group work, one-on-one counseling, and family coaching to tackle moderate to severe AUD or co-occurring disorders.
- Monday/Wednesday/Friday evenings: 3-hour group therapy
- Tuesday: Individual counseling for tailored progress
- Saturday: Peer-led mindfulness workshop in a small cohort
In practice, IOP feels like stepping stones across a river of cravings. Many clients report 70% fewer heavy-drinking days by the end.
Partial Hospitalization Program
Partial Hospitalization Programs (PHP) offer a day-time schedule akin to inpatient care—with the freedom to go home each night. Expect 20+ hours of treatment Monday through Friday.
- Medical Check-Ins: Regular vitals, lab monitoring, and medication management
- Therapy Mix: Individual, group, and family sessions led by a multi-disciplinary team
- Ideal For: Those leaving inpatient detox or facing a high risk of relapse
Outpatient Program Comparison
Below is a side-by-side look at how SOP, IOP, and PHP differ in intensity, duration, setting, and focus.
Introduction: Understanding these distinctions helps you pick the plan that fits your life.
| Program Type | Intensity | Typical Duration | Settings | Key Focus |
|---|---|---|---|---|
| SOP | Low | 6–12 weeks | Evenings | Education, coping skills |
| IOP | Medium | 8–16 weeks | Day/Evening | Group therapy, individual counseling |
| PHP | High | 4–8 weeks | Weekdays | Medical supervision, stabilization |
Conclusion: Whether you need a light touch or an immersive experience, there’s an outpatient path designed to meet you where you are.
Evidence Based Therapies
Not every person responds the same way to treatment. That’s why programs often include:
- Cognitive Behavioral Therapy (CBT) to reframe thought patterns
- Dialectical Behavior Therapy (DBT) for stress tolerance and emotional regulation
- Eye Movement Desensitization and Reprocessing (EMDR) to process trauma
- Mindfulness practices that interrupt automatic urges
“Matching therapy style to an individual’s life story boosts lasting recovery,” says one licensed therapist.
Medication Management And Family Support
Medications like naltrexone, acamprosate, or disulfiram can ease cravings and reduce relapse risk. A psychiatrist will monitor interactions and adjust doses safely. Family coaching sessions teach relatives how to support recovery and improve communication.
- Set up daily medication reminders on your phone or calendar
- Invite loved ones to attend scheduled coaching calls
- Use a shared tracking sheet for mood changes and medication effects
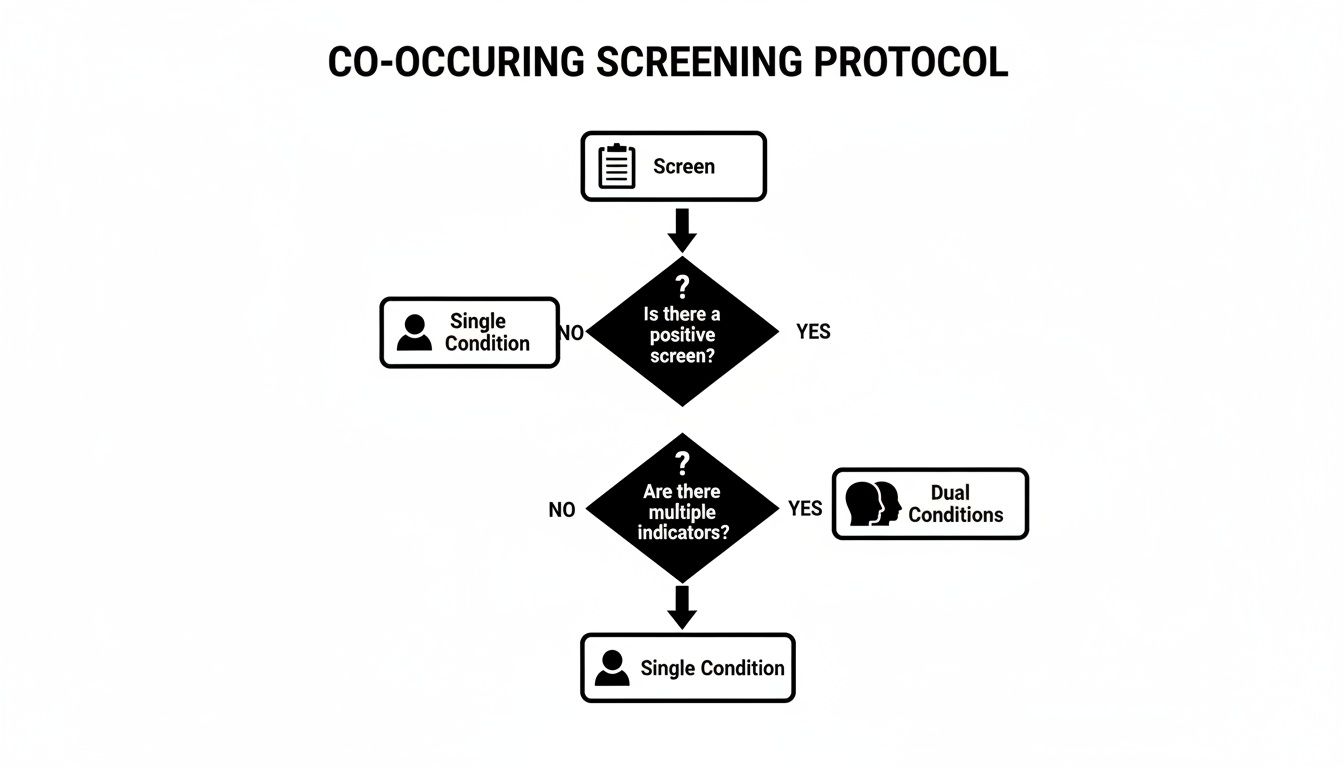
This decision tree shows how an initial screen routes you to single-disorder care or a dual-diagnosis pathway.
Choosing The Right Path
Picking between SOP, IOP, or PHP comes down to symptom severity, daily responsibilities, and insurance coverage. Consider these next steps:
- Review your insurance policy for outpatient benefits and copays
- Ask about telehealth options to fit therapy into a busy schedule
- Verify provider credentials and read client reviews for peace of mind
For ongoing community support, explore peer-led topics and meeting ideas in our guide on recovery group topics.
Next Steps With Altura Recovery Model
At Altura Recovery, we start with an in-depth consultation to map out your unique needs. Your intake includes a medical review, psychological screening, and goal-setting session.
- Define measurable objectives, such as tracking sober days or mood improvements
- Align session times with your work or school commitments
- Engage in peer mentoring and group workshops that reinforce your new skills
Our balanced step-down approach moves you smoothly from PHP to IOP to SOP—much like pacing for a marathon, each stage builds the endurance you need for the next. With Altura’s outpatient model, you keep life on track while making real, sustainable progress.
Practical Steps With Altura Recovery Model
I know firsthand how tough it can be to turn knowledge into action. Altura Recovery’s outpatient model lays out a six-step path—think of it as piecing together a puzzle where every move sets you up for the next.
First, Step 1 invites honest self-reflection. You’ll work through guided exercises that highlight both your strengths and the stress points you need to address.
Next, Step 2 is choosing the right intensity—SOP, IOP, or PHP. It’s like finding boots for a hike: pick the pair that fits your terrain and keeps you moving forward.
- Step 1: Self-reflection exercises to map your starting line
- Step 2: Program selection tailored to your life
- Step 3: Intake coordination and that first welcome call
- Step 4: Insurance checklist so nothing catches you off guard
- Step 5: Scheduling sessions around work, school, or family
- Step 6: Bringing in peer support and celebrating each win
Mapping Your Intake Journey
Organizing your intake feels a bit like planning a trip—there are dates, documents, and a clear itinerary. Altura guides you every step of the way to remove the guesswork.
“Preparation reduces anxiety and speeds intake.”
- Gather personal details and insurance information.
- Schedule your intake call within 48 hours.
- Lock in session times that fit your job or classes.
- Complete online forms and share your recovery goals.
Building Ongoing Support
Steps 4 through 6 lock in your benefits and build a support network. The insurance checklist spells out copays, deductibles, and out-of-pocket limits so you can plan ahead.
By booking therapy early in the week, you avoid conflicts with work and family. Leaning on friends, alumni mentors, or a sponsor makes this less of a solo climb. A simple weekly check-in table helps you track moods, goals, and progress.
Learn more about nurturing connections in our guide to relationships in recovery.
Customizing Treatment Flow
Picture Altura’s step-down approach as your morning routine: you start with full immersion and gradually dial things back as you find your stride.
- Clinical assessments match program intensity to your needs
- Transition plans outline session frequency over time
- Regular goal reviews keep you on track
Alumni report that a structured calendar cuts missed sessions by 40%. Try color-coding blocks for therapy, work, and self-care; set reminders 30 minutes before each session; and review weekly goals with a coach.
Take Jenny, for example. She carved out her lunch hour for IOP sessions at her marketing job and saw a 60% drop in cravings.
With this roadmap, you’re never guessing at the next move. Recovery shifts from a daunting leap into a series of clear, achievable steps—so you feel empowered at every turn.
FAQ
What Defines Someone As A High Functioning Alcoholic
A high functioning alcoholic may juggle deadlines and dinner plans effortlessly. Yet beneath the surface, they meet the clinical criteria for alcohol use disorder. They’re experts at keeping up appearances—nailing presentations in the morning and hiding their evening drinks in the garage. This dual life makes early detection a real challenge.
How Can I Approach A Loved One Who May Be A High Functioning Alcoholic
Finding the right moment is key. Pick a quiet time, away from interruptions, and speak from the heart. Instead of accusing, mention specific observations—missed workouts, secret stashes—and then listen. Closing with an invitation to explore outpatient support together can shift the conversation from confrontation to collaboration.
Recognizing Hidden Warning Signs
- Increasing tolerance, needing more to achieve the same effect
- Sudden secrecy around drinking routines, like texted errands at odd hours
- Noticeable mood swings or spikes in irritability when alcohol wears off
- Unexplained sleep problems, headaches, or stomach issues
“Maintaining a spotless calendar can hide a brewing storm.”
Balancing Work And Recovery
Can Outpatient Treatment Work For Someone With A Full Time Job
Absolutely. Tracks like SOP (Standard Outpatient Program) and IOP (Intensive Outpatient Program) were designed for busy schedules. You’ll often find evening or weekend group sessions, and individual check-ins can fit between morning meetings. Many people even use lunch breaks to meet with their therapist.
What Are Early Warning Signs Of Hidden Alcoholism
Watch for creative excuses to drink at strange times. Empty bottles that vanish overnight. A sudden shift in priorities—work deadlines slide, family dinners get canceled. When alcohol starts cutting in on your goals or relationships, it’s time to seek help.
Every answer here aims to bring clarity and point you toward action. You don’t have to navigate this alone—support that respects your commitments is just a call away.
Ready to explore flexible recovery pathways? Visit Altura Recovery and discover how our outpatient model supports sustainable change.