When someone is dealing with both a mental health condition and a substance use disorder at the same time, clinicians call it a co-occurring disorder. You might also hear the term "dual diagnosis." It's far more common than most people think, and tackling both issues together is a cornerstone of modern, effective treatment.
What Does a Co-Occurring Disorder Mean?
Think of it like trying to drive a car with two flat tires. One flat tire is the mental health issue—say, anxiety—making the ride bumpy and pulling the car to one side. The other is a substance use disorder, pulling it just as hard in another direction. You can’t fix just one tire and expect the car to drive straight. The problems are connected, and you have to address them both to get back on the road safely.
A co-occurring disorder isn’t just two separate problems happening at once. The conditions are deeply intertwined, each one making the other worse in a feedback loop that can feel impossible to break. This tangled relationship creates a unique set of challenges that one-size-fits-all treatment often misses.
How These Conditions Interact
The interplay between a mental health issue and substance use is rarely a simple, one-way street. Even if one problem shows up first, they quickly start influencing each other.
-
Mental Health Issues Can Lead to Substance Use: It often starts as a way to cope. Someone struggling with crippling social anxiety might use alcohol to feel more relaxed and outgoing in social situations. This is sometimes called "self-medication." While it might seem to help in the short term, over time, the alcohol can actually ramp up the underlying anxiety, creating a dependency that adds a whole new layer to the problem.
-
Substance Use Can Trigger Mental Health Issues: On the flip side, heavy or prolonged use of certain drugs can physically alter brain chemistry. This can trigger mental health symptoms like depression, paranoia, or even psychosis in someone who never had them before.
This is precisely why trying to treat one condition while ignoring the other usually fails. It’s like mopping up a flooded floor without turning off the overflowing sink. You can work hard on the visible problem—the substance use—but if you don’t fix the source—the untreated depression or trauma—the mess will just keep coming back.
This cycle isn't a sign of weakness or a lack of willpower. It's a clinical reality driven by a complex mix of genetics, brain chemistry, trauma, and other life experiences. In fact, the National Institute on Drug Abuse (NIDA) reports that about half of all people who have a mental illness will also experience a substance use disorder at some point, and vice-versa. Understanding this connection is the first real step toward finding a recovery path that actually works.
The Tangled Relationship Between Mental Health and Addiction
It's a question we hear all the time: why do mental health struggles and addiction so often show up together? The short answer is that it's rarely a coincidence. Their relationship is a complex, two-way street where each condition can ignite, worsen, and maintain the other, making it incredibly difficult to treat one without addressing both.
Think of it like trying to untangle a knotted ball of yarn. Pulling on one thread just tightens the knots elsewhere.
One of the most common pathways is self-medication. When someone is battling the relentless noise of anxiety, the crushing weight of depression, or the echoes of trauma, they might reach for a substance just to get a moment of peace. Alcohol can temporarily quiet racing thoughts, and opioids might numb deep emotional pain. In that moment, it feels like a solution.
But it’s a dangerous trap. The relief is always temporary, and over time, substance use almost always makes the original mental health symptoms worse. This creates a vicious cycle that's incredibly hard to break on your own.
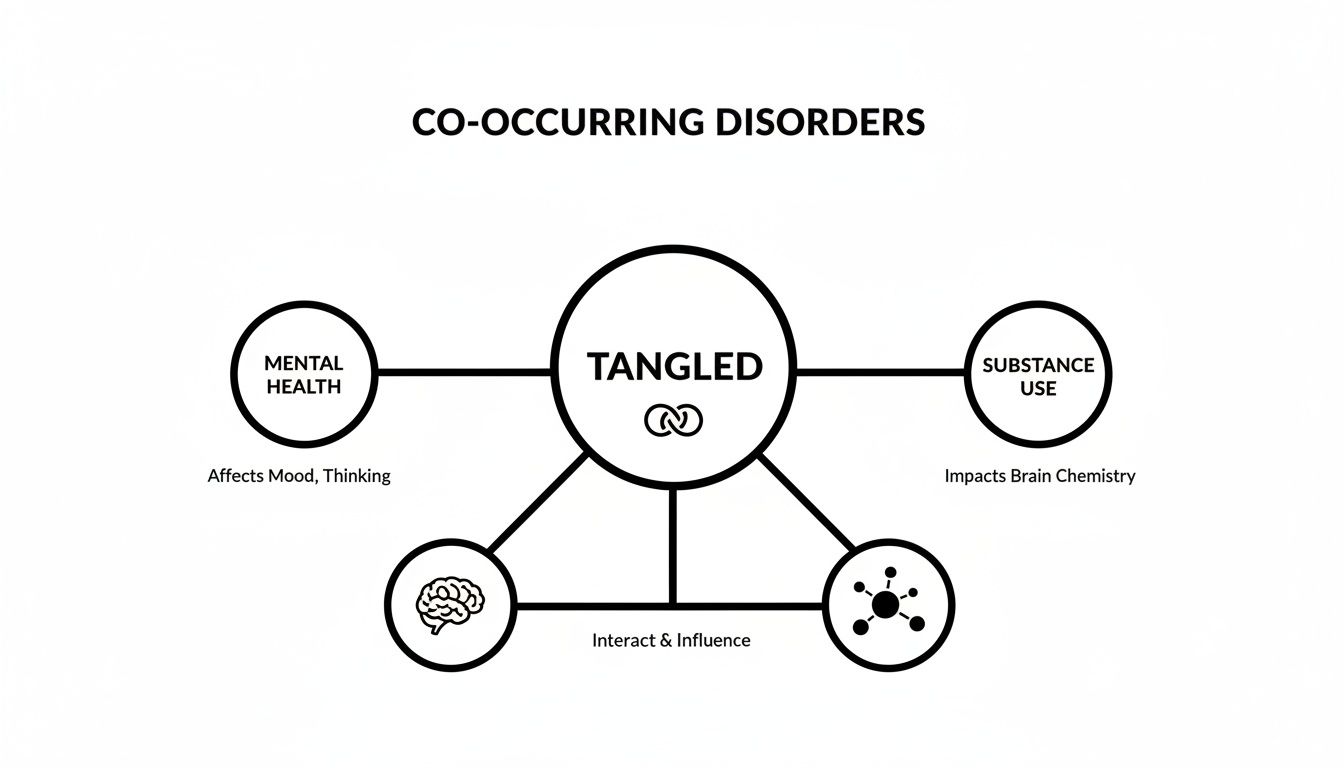
As you can see, these aren't two separate problems happening at the same time. They are a single, intertwined issue that demands a unified approach to heal effectively.
Shared Underlying Causes
Beyond the self-medication cycle, there are often common roots—both biological and environmental—that make a person vulnerable to both conditions at once. Understanding these factors helps clarify why this isn't about a lack of willpower, but a complex mix of circumstances.
-
Genetic Predisposition: Your family history can play a major role. Certain genetic markers can dial up the risk for both mental health disorders and addiction, essentially predisposing someone to both.
-
Brain Chemistry: Both conditions often involve imbalances in the same brain regions and neurotransmitter systems. Chemicals like dopamine and serotonin, which manage our mood, pleasure, and impulse control, are frequently at the center of the storm.
-
Environmental Factors: Life experiences, especially early ones, shape the brain profoundly. Exposure to intense stress, trauma, or neglect during childhood can alter brain development in ways that increase the risk for both disorders down the road.
The intricate nature of these conditions means one disorder can directly influence or even cause another. We see this all the time, for example, in the significant link between OCD and depression. The connection is undeniable and statistically significant.
The numbers tell a stark story. In the U.S., a staggering 48.5 million people aged 12 or older had a substance use disorder in the past year as of 2023. Even more telling is that adults with a serious mental illness (SMI) showed a 51.9% rate of illicit drug use. That's more than double the 21.0% rate for adults without any mental illness.
This data paints a crystal-clear picture: where you find a serious mental health challenge, you very often find a co-occurring substance use issue. It’s why a comprehensive diagnosis that looks at the whole person isn't just helpful—it's the only way to build a real, lasting road to recovery.
Recognizing the Signs of a Dual Diagnosis
Figuring out if you or a loved one is dealing with a dual diagnosis is tricky. It's one thing to understand the concept, but it's another entirely to spot it in the real world. The signs are often a tangled mess because the symptoms of the mental health condition and the substance use disorder can overlap, hide each other, or even mix together to create new behaviors.
This entanglement is what makes it so confusing. What looks like a classic sign of depression—like pulling away from friends and family—might actually be driven by a struggle with alcohol. On the flip side, someone’s erratic behavior might be blamed on substance use when it's really a symptom of an underlying bipolar disorder. The key is to step back and look at the whole picture instead of focusing on isolated incidents.
Common Pairings and Their Warning Signs
Some mental health and substance use disorders show up together far more often than others. This usually happens because the substance offers a temporary—and ultimately harmful—fix for the specific symptoms of the mental health condition.
Think about it: someone crippled by social anxiety might lean on alcohol just to feel normal in a crowd. A person battling the relentless, intrusive thoughts of PTSD may turn to sedatives to quiet their mind. These patterns of self-medication quickly create powerful, destructive feedback loops.
The temporary relief a substance offers often comes at a high cost, creating a rebound effect that makes the original mental health symptoms even more severe. A few drinks might ease anxiety for an evening, but the resulting "hangxiety" the next day can be crippling, prompting the person to drink again.
Learning to spot these pairings is a huge first step. Some of the most common duos involve anxiety and depression co-occurring with substance use. In the U.S., about 19.1% of adults have an anxiety disorder, and it's no surprise that many turn to substances to cope. In fact, research suggests that roughly 8.1% of the population is dealing with both a mental illness and a substance use disorder at the same time. You can learn more about these connections from research published by Frontiers in Psychiatry.

This dynamic can make it incredibly difficult to see the full scope of the problem. A person might appear to be a high-functioning alcoholic, successfully managing work and family life, while internally their drinking is a desperate attempt to keep severe depression at bay. You can read more about the signs of a high-functioning alcoholic in our guide.
To make these connections clearer, let’s look at some common pairings and the signs they produce.
Recognizing Co-Occurring Disorders Common Pairings and Signs
| Mental Health Condition | Commonly Paired Substance | Key Signs and Symptoms to Watch For |
|---|---|---|
| Anxiety Disorders (GAD, Social Anxiety, Panic Disorder) | Alcohol, Benzodiazepines, Cannabis | Using substances before social events; increased isolation to avoid anxiety-provoking situations; panic attacks followed by substance use to "calm down." |
| Depression (Major Depressive Disorder) | Alcohol, Stimulants (Cocaine, Amphetamines) | Drinking alone to numb feelings of sadness or hopelessness; using stimulants for a temporary mood/energy boost, followed by a severe crash; neglecting hygiene and responsibilities. |
| Post-Traumatic Stress Disorder (PTSD) | Opioids, Alcohol, Sedatives | Using substances to suppress traumatic memories or nightmares; avoiding people or places that trigger memories; emotional numbness punctuated by angry outbursts. |
| Bipolar Disorder | Alcohol, Cocaine, Cannabis | Cycles of heavy binge drinking or stimulant use during manic phases, followed by using sedatives or alcohol during depressive episodes; impulsive, risky behaviors while under the influence. |
| Attention-Deficit/Hyperactivity Disorder (ADHD) | Stimulants (misuse of prescription or illicit), Nicotine, Alcohol | Using stimulants in a non-prescribed way to try and focus; chain-smoking or heavy drinking to manage restlessness or impulsivity; chronic disorganization and financial problems. |
Seeing these symptoms together—not just in isolation—is often the first clue that more than one issue is at play.
Connecting the Dots
So, how do you sort through the noise and distinguish the signs? A good strategy is to observe how a person's behaviors, emotions, and social habits change over time, especially in relation to their substance use.
Keep an eye out for these general warning signs:
- Behavioral Changes: Are there sudden shifts in energy, from hyperactive to lethargic? Are they neglecting work, school, or family responsibilities? Have they become secretive or run into legal or financial trouble?
- Emotional Instability: Are mood swings extreme and unpredictable? Is there a noticeable increase in irritability, anger, or apathy? Do they express overwhelming feelings of hopelessness or worthlessness?
- Social Withdrawal: Are they pulling away from friends and family? Have they lost interest in hobbies they once loved? Do they only seem to socialize in situations where alcohol or drugs are easily available?
If you notice these patterns, and especially if you see a clear link where substance use makes mental health symptoms worse (or vice versa), it's a strong indicator of a co-occurring disorder. Recognizing this connection is the first, most critical step toward getting a proper diagnosis and finding a path to integrated treatment that addresses both issues at once.
Why Integrated Treatment Is the Only Way Forward
Trying to treat an addiction without touching the anxiety fueling it is like fixing a leaky pipe but leaving the water damage to rot. You might stop the immediate drip, but the real, lasting destruction continues untouched. For anyone trying to define co-occurring disorders, the how of treatment is just as critical as the what of the diagnosis. Treating these intertwined conditions separately is an outdated model, and frankly, it just doesn’t work.
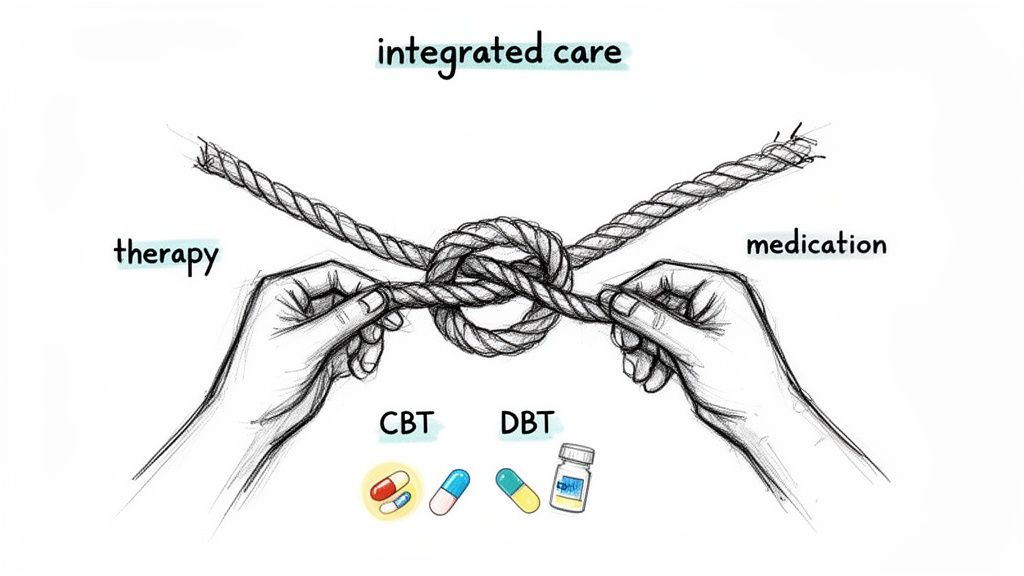
Think about untangling a tightly knotted rope. If you only pull on one strand—say, the substance use—you just make the knots on the other end tighter. The only way to succeed is to work on the entire knot at once, carefully loosening each part in relation to the others. This is the heart of integrated treatment.
What True Integrated Care Looks Like
Integrated care isn't just about having a psychiatrist and an addiction counselor in the same building. It's a philosophy—a single, cohesive team works with you to address both conditions at the same time, under one unified treatment plan. This approach finally treats you as a whole person, not a collection of separate problems.
This unified strategy is so crucial because the symptoms of each disorder are constantly in conversation with the other. A wave of depressive symptoms can easily trigger a relapse, while substance use can crank up the volume on feelings of hopelessness. An integrated team gets this dynamic. They adjust your care in real-time to manage these interactions, implementing evidence-based practice to ensure you're getting the most effective, research-backed strategies.
An integrated approach acknowledges a simple truth: you can't heal one part of yourself while another is still bleeding. Lasting recovery demands a plan that sees the complete picture and provides comprehensive, simultaneous care.
Key pieces of a strong integrated treatment plan usually include:
- Simultaneous Therapy: Using powerful therapeutic models like Cognitive Behavioral Therapy (CBT) or Dialectical Behavior Therapy (DBT) to tackle the thought patterns and behaviors driving both the mental health condition and the substance use.
- Coordinated Medication Management: A psychiatrist oversees all medications to make sure they effectively treat mental health symptoms without creating dependency risks or negative interactions. You can learn more about how medications like naltrexone work as part of a complete plan.
- Trauma-Informed Care: Because trauma is so often a root cause of co-occurring disorders, therapies like Eye Movement Desensitization and Reprocessing (EMDR) are frequently woven in to heal those underlying wounds.
- Holistic Support: Building a strong foundation for long-term well-being by incorporating life skills training, family therapy, and detailed relapse prevention planning.
Why This Approach Has Better Outcomes
When treatment is fragmented—sending someone to one clinic for addiction and another for depression—progress stalls out. Clinicians end up working in silos, communication breaks down, and the patient is stuck in the middle, often getting conflicting advice. It's a recipe for failure.
Integrated care solves this by creating a seamless, coordinated experience. It dramatically improves outcomes by lowering the risk of relapse, boosting engagement in treatment, and empowering people with a unified set of coping skills.
By addressing the root causes and the symptoms at the exact same time, it provides the strongest possible foundation for real, sustainable recovery.
How to Start Your Recovery Journey
Taking that first step toward getting help can feel like the hardest part of the entire process. The path forward might seem blurry or even a little intimidating, but modern outpatient care is built to be as simple and supportive as possible.
It all starts with a confidential phone call—a judgment-free conversation to understand what’s going on in your life. This is your chance to ask questions and share your concerns with a compassionate admissions coordinator who will listen and gather just enough information to schedule a comprehensive clinical assessment. This evaluation isn’t a test; it’s a collaborative process.
Demystifying the Assessment Process
During your assessment, a licensed clinician will talk with you about your mental health history, any patterns of substance use, and your overall life circumstances. The goal is to get a complete, 360-degree view of your experience so we can create a treatment plan that’s truly personalized. This is where we figure out the right level of support you need.
Based on what you’re going through, clinicians might recommend one of several outpatient options:
- Partial Hospitalization Program (PHP): This is the most structured level of outpatient care, offering intensive therapy for several hours a day, five days a week, while you continue to live at home.
- Intensive Outpatient Program (IOP): Offering a bit more flexibility, an IOP typically involves several hours of therapy, three to five days a week. We often have both day and evening sessions available to fit your schedule.
- Supportive Outpatient Program (SOP): This is a step-down level of care with fewer weekly hours, designed to help you transition back to daily life while keeping a strong support system firmly in place.
The core principle of modern outpatient treatment is integration, not disruption. The right program is designed to fit into your life—allowing you to keep up with work, school, or family responsibilities—not force you to put everything on hold.
Building Your Personalized Treatment Plan
Once we’ve identified the right level of care, you’ll work directly with your clinical team to build a roadmap for your recovery. This isn’t a one-size-fits-all plan. It’s tailored specifically to you, combining powerful therapeutic methods like CBT or EMDR with individual counseling, group therapy, and medication management if needed.
For busy professionals, students, and parents, this kind of flexibility is a game-changer. You can find out more about how these programs work by exploring our guide on the intensive outpatient program for substance abuse.
Ultimately, starting your journey is about finding a program that meets you exactly where you are. It’s about getting the integrated support needed to heal both the mental health and substance use conditions together, creating a solid foundation for lasting freedom.
Your Questions About Co-Occurring Disorders, Answered
When you or someone you care about is facing a dual diagnosis, a lot of questions come up. It's completely normal. Below are some straightforward answers to the things people most often wonder about.
Which Disorder Should Be Treated First?
This is probably the most common—and most critical—question we hear. The answer, backed by years of clinical evidence, is that you don't treat one and then the other. The gold standard is integrated treatment.
Integrated treatment means the substance use disorder and the mental health condition are addressed at the same time, by the same team. Trying to treat them separately is like trying to fix a leaky boat one hole at a time; as soon as you patch one, the other gets worse. The symptoms are tangled together, so the healing has to be, too. This approach treats the whole person, not just isolated problems, which is the only way to build a recovery that truly lasts.
Can I Get Treatment While Still Working or Going to School?
Absolutely. In fact, that's what modern outpatient programs are specifically designed for. The entire model is built around flexibility so you can weave recovery into your real life instead of having to press pause on everything.
The goal is to build skills and resilience that you can apply in your real-world environment immediately. Treatment shouldn’t be a pause button on your life; it should be a support system that runs alongside it.
This is why programs like Intensive Outpatient (IOP) and Supportive Outpatient (SOP) offer day, evening, and even virtual sessions. You can keep up with your job, your classes, and your family commitments while getting the deep, effective care you need to get better.
How Can Family Best Support Someone with a Dual Diagnosis?
Family support is a game-changer in recovery. The most powerful things you can do are to educate yourself about both conditions, practice a ton of patience, and lead with compassion. It’s essential to let go of blame and remember that recovery is a journey with ups and downs, not a straight line.
Getting involved in specialized programs can make a huge difference. Learning through family therapy for substance abuse gives everyone practical tools for setting healthy boundaries, communicating more effectively, and creating a stable home environment. Honestly, one of the most important roles you can play is simply encouraging your loved one to stick with their integrated treatment plan. That steady support is priceless.
At Altura Recovery, we specialize in creating personalized, integrated treatment plans that fit your life. If you or a loved one are ready to start the journey toward real healing, reach out to our compassionate team today by visiting https://www.alturarecovery.com.