Let's get straight to the big question: can you take Suboxone while pregnant? Yes, you can. In fact, for women with opioid use disorder, it’s the recommended standard of care. This isn’t about picking a risky option; it's about choosing a medically supervised treatment that protects both you and your baby from the severe dangers of untreated addiction.
The Medical Consensus: Suboxone Is Safer for You and Your Baby

When you’re expecting, every decision feels monumental, especially when it involves medication. The fear and uncertainty around using Suboxone during pregnancy are completely understandable. But the good news is that major medical organizations agree: the benefits of stabilizing opioid use disorder with Suboxone far outweigh the risks of leaving it untreated.
Untreated opioid use throws you and your developing baby into a chaotic cycle of intoxication and withdrawal. This constant instability can lead to serious complications, including poor fetal growth, preterm birth, and even maternal overdose.
Suboxone brings stability. It works by stopping withdrawal symptoms and cravings without causing the dangerous highs and lows of illicit opioid use. This creates a much safer and more predictable environment in the womb, which is exactly what a baby needs for healthy development. Think of it as a protective shield around your pregnancy, guarding it from the volatility of active addiction.
Why Managed Care Is the Safest Path
Opting for medically supervised Suboxone treatment is a proactive step toward a healthier outcome for everyone. It ensures you receive consistent prenatal care, lowers the risk of relapse, and boosts your overall well-being. The alternative—untreated opioid use—is a gamble with unpredictable and significant dangers for both mother and child.
The goal of Suboxone treatment in pregnancy isn't just managing addiction; it's about creating stability. A stable maternal environment gives the baby the best possible chance for healthy growth, free from the stress of withdrawal cycles.
To make the comparison clearer, the table below breaks down the key differences between managed treatment and untreated OUD during pregnancy.
Suboxone Treatment vs. Untreated Opioid Use Disorder in Pregnancy
| Outcome/Risk Factor | Managed with Suboxone | Untreated Opioid Use Disorder |
|---|---|---|
| Maternal Stability | Consistent medication levels prevent withdrawal and cravings, promoting stability. | Cycles of intoxication and withdrawal cause extreme physical and emotional stress. |
| Prenatal Care | Regular medical appointments are part of the treatment plan, ensuring consistent monitoring. | Inconsistent or no prenatal care is common, leading to missed health issues. |
| Risk of Relapse | Significantly reduced due to stabilized brain chemistry and structured support. | High and constant, with an associated risk of overdose. |
| Fetal Growth | Promotes healthier fetal development by providing a stable uterine environment. | Increased risk of poor fetal growth, low birth weight, and placental abruption. |
| Infectious Disease | Reduces risk of exposure to HIV and Hepatitis C from IV drug use. | High risk of contracting and transmitting infectious diseases. |
| Preterm Labor | Lower risk compared to untreated OUD. | Significantly higher risk due to maternal stress and withdrawal. |
| Neonatal Outcome | Neonatal Opioid Withdrawal Syndrome (NOWS) is possible and medically manageable. | Severe and unpredictable NOWS, often complicated by other health issues. |
This side-by-side view helps illustrate why healthcare providers overwhelmingly recommend Suboxone as the safest path forward. It’s a choice for health, for stability, and for a brighter future for you and your baby.
How Suboxone Actually Works to Create Stability
To really get why Suboxone is considered the gold standard of care during pregnancy, it helps to understand what it’s actually doing inside your body and brain. The science is all geared toward one simple goal: creating a safe, stable environment for both you and your baby.
Think of the opioid receptors in your brain as tiny locks. Full opioids like heroin or oxycodone act like master keys—they fit perfectly, turn the lock all the way, and unleash an intense, euphoric rush. This powerful effect is what fuels the chaotic cycle of use and withdrawal, creating enormous stress on your system.
Suboxone works on a whole different principle. Its main ingredient, buprenorphine, is what’s known as a partial opioid agonist. In our lock-and-key analogy, it’s a specially designed key that fits the same lock but only turns it partway. It binds tightly to those receptors, effectively blocking other opioids from getting in and taking over.
This partial activation is the secret to its success. It’s just enough to satisfy the brain’s craving for opioids, which puts a stop to withdrawal symptoms before they can start. But because the key doesn’t turn all the way, it never produces that overwhelming high. This “ceiling effect” discourages misuse and helps break the cycle of intoxication for good.
The Role of Buprenorphine and Naloxone
Suboxone is actually a combination of two different drugs, and each one has a very specific job. Grasping the difference between physical vs psychological dependence can make it clearer why this two-part approach is so effective.
- Buprenorphine: This is the heavy lifter doing all the therapeutic work. It occupies the opioid receptors to keep you stable, stamp out cravings, and prevent withdrawal.
- Naloxone: This ingredient is an opioid antagonist, meaning it’s designed to block opioid effects. It’s added purely as a safety measure to discourage misuse. When you take Suboxone the right way (dissolving it under your tongue), almost none of the naloxone gets into your bloodstream. It just stays inactive.
If someone tried to misuse Suboxone by injecting it, the naloxone would activate immediately. It would kick other opioids off the receptors and trigger sudden, severe withdrawal symptoms. This built-in safety net makes Suboxone a much more secure option for treatment.
This carefully engineered mechanism is what allows Suboxone to build a steady, predictable foundation for recovery. It manages the physical side of opioid use disorder, freeing up the mental and emotional space you need to focus on your health and your pregnancy. By leveling out the dangerous highs and lows of active use, it gives your baby the consistent, stable environment they need to develop healthily from day one.
Weighing the Benefits of Treatment Against the Risks
Deciding on any medication during pregnancy feels like a high-stakes balancing act. When it comes to taking Suboxone, it's not just about looking at the medication's potential risks—it's about weighing them against the very real, very serious dangers of untreated opioid use disorder (OUD).
The single biggest benefit of Suboxone treatment is stability. Think of untreated OUD as a constant, chaotic storm inside the womb, with cycles of intoxication and withdrawal stressing a developing baby. This unrelenting stress significantly increases the chances of devastating outcomes like miscarriage, preterm labor, and poor fetal growth.
Suboxone steps in to calm that storm. By keeping your body in a steady, predictable state, it creates the safe and consistent environment a baby needs to develop healthily.
Understanding the Primary Risk: Neonatal Abstinence Syndrome
The main risk everyone talks about is that your baby may be born with a condition called Neonatal Abstinence Syndrome (NAS), also known as Neonatal Opioid Withdrawal Syndrome (NOWS). This is a set of treatable withdrawal symptoms a newborn can experience after being exposed to opioids in the womb.
It’s so important to reframe how you think about NAS. It is not a sign that something has gone wrong or that you've harmed your baby. Instead, it's an expected and manageable side effect of a life-saving medication. Your medical team will be completely prepared to monitor and care for your baby after delivery with simple, supportive measures, like:
- Swaddling and comforting to help them feel secure.
- Plenty of skin-to-skin contact to regulate their heart rate and temperature.
- A quiet, low-light environment to keep them from feeling overstimulated.
- Small, frequent feedings to help them grow strong.
While some babies might need medication to ease their symptoms, many newborns with NAS get through it with this kind of supportive, loving care alone.
The medical consensus is crystal clear: the benefits of a stable, healthy pregnancy on Suboxone far outweigh the manageable and temporary risk of NAS. You're choosing predictability over chaos.
Data Confirms Better Outcomes with Treatment
The evidence overwhelmingly backs this up. One major U.S. study found that the rate of adverse pregnancy outcomes was 25.4% for mothers treated with buprenorphine. That number was significantly lower than the 30.8% rate among pregnant women with untreated OUD.
Specifically, the group on buprenorphine had fewer severe maternal health problems, fewer preterm births, and fewer babies needing NICU admission. The data points to a clear conclusion: treatment leads to healthier moms and healthier babies.
Of course, beyond Suboxone, expectant mothers have to navigate many other health choices, from managing common aches and pains to choosing other pregnancy-safe remedies. Making every choice with guidance from your healthcare team is key. Ultimately, choosing Suboxone is a powerful, proactive step toward giving both you and your baby the healthiest future possible.
What a Suboxone Treatment Plan Looks Like During Pregnancy
Starting a Suboxone treatment plan while you're pregnant is a powerful, proactive step toward health for both you and your baby. It's a journey built on collaborative care, and you absolutely won't be doing it alone. You'll be supported by a dedicated team every step of the way.
Typically, this team includes your OB-GYN, who looks after your pregnancy, and an addiction specialist who manages your Suboxone treatment. They work hand-in-hand, communicating regularly to make sure both your health and your baby's development are always the top priority. This integrated approach ensures nothing falls through the cracks.
The very first and most important step is finding the right dose of Suboxone. The goal here is simple but critical: stability. Your doctor will work with you to find a dose that completely eliminates withdrawal symptoms and keeps cravings from creeping back in.
Maintaining Stability Throughout Pregnancy
There's a common misconception that you should try to taper off Suboxone during pregnancy. This is not the recommended approach and can be risky.
Suddenly stopping or lowering your dose can throw your body into withdrawal, creating a high-stress situation that could lead to relapse and cause significant harm to the fetus. The primary goal is to maintain a stable, therapeutic dose throughout your entire pregnancy.
Your treatment roadmap is designed to be predictable and supportive, reducing any anxiety about what comes next. It will involve:
- Regular Prenatal Visits: These appointments are essential for monitoring your health and tracking your baby's growth.
- Coordinated Addiction Care: You’ll have consistent check-ins with your addiction specialist to manage your dose and provide ongoing counseling. Many women find an outpatient substance abuse program offers the flexibility needed to balance treatment with the demands of life.
- Delivery Planning: Well before your due date, your care team will coordinate with the hospital staff. This ensures a smooth, prepared, and supportive delivery experience for both you and your baby.
A well-structured treatment plan does more than just manage OUD; it provides a predictable and supportive framework that empowers you to focus on what matters most—having a healthy pregnancy.
Comprehensive care also means focusing on your overall well-being. Many expectant mothers find huge value in weaving self-care into their routine. For instance, exploring things like nurturing spa treatments tailored for pregnancy can be a wonderful way to manage stress and promote relaxation.
This kind of holistic approach perfectly complements your medical treatment, supports your mental health, and helps set you and your baby up for the best possible outcome.
Life After Delivery for You and Your Newborn

The postpartum period is an incredible, and incredibly demanding, chapter. After working so hard for a stable pregnancy on Suboxone, the game plan now shifts to making sure both you and your new baby get the focused care you need to thrive. For your little one, that means being monitored for Neonatal Abstinence Syndrome (NAS).
It’s important to know that NAS is a treatable and expected withdrawal condition that hospital staff are completely prepared to manage. It's a known side effect of the very medication that kept you and your baby safe—not a setback or a sign of failure. The medical team will simply watch for common signs, which usually show up within 72 hours of birth.
Caring for Your Newborn with NAS
The first and most powerful response to NAS is supportive, non-pharmacological care. The whole idea is to create a calm, soothing bubble that minimizes your baby's stress and helps them gently adjust to the world.
These supportive measures are surprisingly simple but effective:
- A Quiet Environment: Keeping the lights low and the noise down helps prevent a sensitive newborn from becoming overstimulated.
- Frequent Swaddling: Being wrapped up snugly feels a lot like the security of the womb, which can work wonders for an irritable baby.
- Skin-to-Skin Contact: Holding your baby directly on your chest is a powerhouse move. It helps regulate their temperature, heart rate, and breathing like nothing else.
- Small, Frequent Feedings: This approach keeps their nutrition steady and can make feeding much easier if they're having difficulties.
If these gentle methods aren't quite enough to manage more severe symptoms, doctors may use medication to help. But the starting point is always these nurturing, hands-on techniques.
The postpartum period is a time of massive change and high stress, a combination that can be a major trigger for relapse. Sticking with your Suboxone treatment is the single most important thing you can do to protect your recovery and be fully present for your new baby.
Continuing Your Treatment and the Role of Breastfeeding
For you, the new mom, continuing your Suboxone dose after delivery is non-negotiable. The whirlwind of hormonal shifts, sleep deprivation, and the new weight of responsibility can create a perfect storm for relapse. Your medication is the anchor that provides the stability you need to navigate this beautiful but challenging time. To fully grasp this risk, it’s helpful to understand what relapse means in mental health and how to safeguard your hard-won progress.
On top of that, breastfeeding is strongly encouraged for mothers on a stable dose of Suboxone. The science is clear: only tiny, clinically insignificant amounts of the medication find their way into breast milk. The benefits of bonding, nutrition, and comfort for the baby—especially one working through NAS symptoms—are seen as far more valuable than any minimal risks. It’s a powerful tool for connecting with and soothing your newborn while you continue to support your own recovery journey.
Comparing Suboxone to Other Treatment Options
When it comes to treating opioid use disorder in pregnancy, Suboxone and methadone are the two leading, evidence-backed options. While both are considered the gold standard, they aren't interchangeable. Understanding the key differences is crucial for making an informed decision with a healthcare provider, and often, one is a better fit than the other depending on the individual's needs.
The biggest distinction lies in how they work inside the body. Methadone is what's known as a full opioid agonist, while buprenorphine (the active ingredient in Suboxone) is a partial agonist. This might sound like a minor detail, but it has major implications for safety, risk of overdose, and potential drug interactions, often giving Suboxone a more favorable profile.
Suboxone vs. Methadone
One of the most compelling reasons clinicians often prefer Suboxone during pregnancy relates directly to the newborn's health. A large body of research consistently shows that babies exposed to buprenorphine in the womb tend to have a much milder form of Neonatal Abstinence Syndrome (NAS) compared to those exposed to methadone.
This means less severe withdrawal symptoms and, crucially, a shorter hospital stay for the baby.
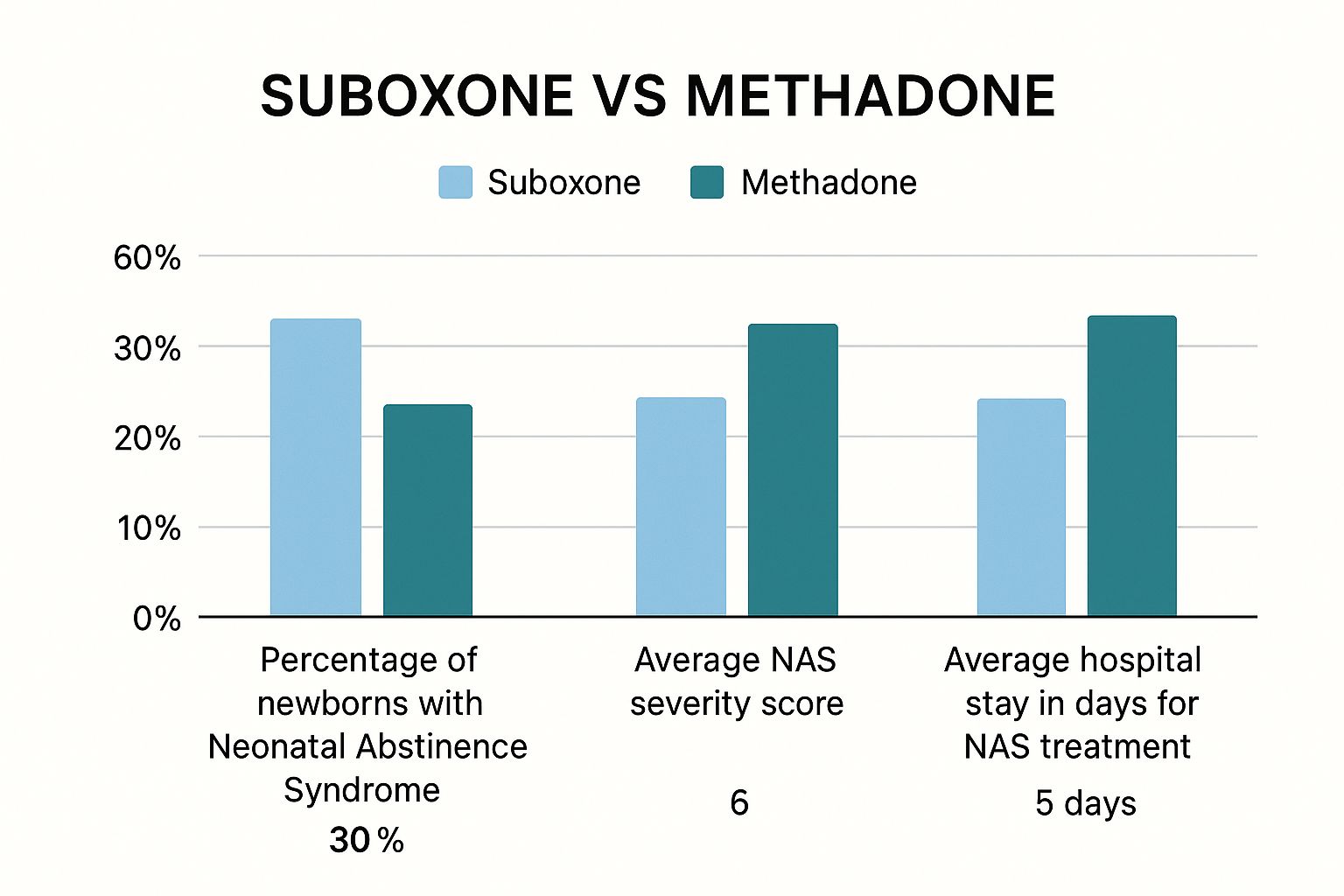
As the data shows, a shorter, less intense withdrawal period is a significant benefit for both the infant and the new parents, allowing families to get home and start their lives together sooner.
To give you a clearer picture, let's break down the main considerations for each medication when used during pregnancy.
Treatment Options for Opioid Use Disorder in Pregnancy
| Feature | Suboxone (Buprenorphine-Naloxone) | Methadone |
|---|---|---|
| Mechanism | Partial opioid agonist; provides a "ceiling effect" for safety. | Full opioid agonist; fully activates opioid receptors. |
| Newborn Outcome (NAS) | Associated with less severe NAS and shorter hospital stays. | Associated with more severe NAS and longer treatment times. |
| Safety Profile | Lower overdose risk due to the ceiling effect. | Higher overdose risk if not managed carefully; requires daily visits. |
| Dosing Flexibility | More flexible; can be prescribed for take-home doses (monthly). | Highly structured; typically requires daily visits to a clinic. |
| Drug Interactions | Fewer significant drug interactions. | More potential interactions with other medications. |
| Best For | Patients who are stable and can manage take-home prescriptions. | Patients who need more structure or have not succeeded with Suboxone. |
Ultimately, the choice is a clinical one made between a patient and their doctor. But because of the gentler impact on the newborn and the greater flexibility it offers the mother, Suboxone is frequently recommended as the first-line treatment for pregnant patients.
Suboxone vs. Subutex in Pregnancy
For years, many doctors gravitated toward Subutex, the buprenorphine-only formula, for pregnant women. The thinking was that the naloxone in Suboxone might pose an unnecessary risk to the fetus. However, newer and more extensive research has completely flipped that old assumption on its head.
We now know that when Suboxone is taken as directed (dissolved under the tongue), the naloxone component has almost zero absorption into the bloodstream. It doesn't cross the placenta and doesn't harm the baby.
In fact, the latest evidence suggests the buprenorphine-naloxone combo in Suboxone might actually lead to better outcomes. A recent landmark study of over 8,000 pregnancies found that newborns exposed to the Suboxone formula had a NAS rate of just 37.4%. That’s significantly lower than the 55.8% rate seen in babies exposed to buprenorphine alone.
This data provides strong reassurance that the combination formula is not only safe but potentially more beneficial. If you want to dive deeper into how these two medications compare, you can learn more about the difference between Suboxone and Subutex in our detailed guide.
Answering Your Biggest Questions About Suboxone and Pregnancy
Even with all the facts laid out, it's completely normal to have lingering questions and worries. Let's walk through some of the most common concerns to get you the clear, straightforward answers you need.
Will Taking Suboxone Harm My Unborn Baby?
This is the number one question on every expecting mother's mind. The simple truth is that the risks from untreated opioid use—like miscarriage, poor fetal growth, or a fatal maternal overdose—are far more dangerous than the risks of taking Suboxone exactly as prescribed.
While your baby will be exposed to the medication and may have a manageable withdrawal condition (called NAS) after birth, Suboxone provides the stable, calm uterine environment they need to develop healthily.
Leading medical organizations are all in agreement: for both you and your baby, Suboxone is the safer and healthier choice. It breaks the chaotic and dangerous cycle of active addiction.
Can I Breastfeed if I Am on Suboxone?
Yes, breastfeeding is generally considered safe and is highly encouraged for mothers who are on a stable dose of Suboxone. Only a very tiny amount of the medication gets into breast milk, and experts agree that the powerful benefits of breastfeeding far outweigh any minimal risks.
For babies experiencing NAS symptoms, breastfeeding can be incredibly comforting and helpful. Just be sure to talk through your plans with your healthcare team so everyone is on the same page.
Will My Doctor Make Me Stop Taking Suboxone?
Absolutely not. Stopping Suboxone suddenly while pregnant is dangerous and is never medically advised. Doing so can trigger severe withdrawal, which creates a high risk of relapse and puts incredible stress on the fetus.
The standard of care is to keep you on a stable, therapeutic dose throughout your pregnancy and well into the postpartum period to ensure both you and your baby stay safe and healthy.
At Altura Recovery, we get how challenging it is to navigate pregnancy while also staying committed to your recovery. We provide the compassionate, expert care you need to build a healthy future for yourself and your baby. Learn more about our supportive outpatient programs.








