An outpatient substance abuse program is a unique approach to addiction treatment that lets you get help while still living at home. It’s designed to weave recovery into your daily life, allowing you to keep up with work, school, and family obligations on a flexible yet structured path to sobriety.
What an Outpatient Program Really Means for Your Life

Think of it like learning any other vital skill, like a new language or a professional trade. Instead of moving away to a dedicated campus, you attend classes and workshops that fit right into your existing schedule. That’s the core idea of an outpatient program—it integrates recovery directly into your real world.
Unlike residential or inpatient treatment, which requires you to live at a facility 24/7, outpatient care provides structured therapy and support for a set number of hours each week. The model is built on a powerful principle: true, lasting recovery happens when you learn to apply new coping skills in the very environment where your triggers and stressors live.
To help clarify the differences, here’s a quick look at how the two models compare.
Outpatient vs Inpatient Treatment at a Glance
| Feature | Outpatient Program | Inpatient (Residential) Program |
|---|---|---|
| Living Situation | Live at home | Live at the treatment facility |
| Time Commitment | 3-20+ hours per week | 24/7 structured environment |
| Daily Life | Continue with work, school, and family | Pause daily responsibilities |
| Ideal Candidate | Stable home, strong support, motivated | Unstable environment, needs medical oversight |
This table offers a snapshot, but choosing the right path involves a lot more nuance. You can explore a more detailed comparison in our article on outpatient vs. inpatient rehab.
Who Is the Ideal Candidate for Outpatient Treatment?
This flexible approach isn't a one-size-fits-all solution; it’s carefully designed for individuals who have a specific set of circumstances in their corner. An ideal candidate for an outpatient substance abuse program typically has:
- A Stable Home Environment: A safe and supportive place to live is absolutely crucial, as it provides a secure foundation outside of treatment hours.
- A Strong Support System: Having encouragement from family, friends, or a partner can make a world of difference when navigating the daily challenges of recovery.
- High Motivation for Change: Because this model offers more freedom, a strong personal commitment to showing up and doing the work is essential.
- No Need for Medical Detox: This is best for individuals who don't require intensive, around-the-clock medical supervision to manage withdrawal symptoms safely.
In short, this model is for those who can manage their day-to-day lives but need professional guidance and structure to overcome substance use for good. It acts as a bridge between highly intensive care and fully independent sober living.
The power of an outpatient program lies in its real-world application. You don't just learn about managing triggers in a classroom—you practice it that same day at home, at work, and in your community.
A Spectrum of Care
It’s important to understand that "outpatient" is not a single, rigid program. It’s actually a spectrum of different care levels, ranging from just a few hours a week to more intensive schedules that feel more like a part-time job.
This flexibility allows treatment plans to be precisely adjusted to your clinical needs, ensuring you get the right amount of support at exactly the right time in your recovery journey.
Understanding the Levels of Outpatient Care
Not all outpatient programs are created equal. The term "outpatient" actually covers a whole spectrum of care, with each level offering a different intensity and time commitment. It’s designed to meet you exactly where you are in your recovery.
Navigating the different acronyms can feel a little confusing at first, but figuring them out is the key to finding the right fit for your life.
Think of it like different types of physical training. Some people need a full-time, immersive camp to get started (that's like a PHP). Others need a consistent, part-time training schedule (IOP), and some just need a weekly check-in with a coach to stay on track (SOP). Each one serves a distinct purpose on the path forward.
Standard Outpatient Programs (SOP)
The most flexible option on the table is the Standard Outpatient Program (SOP). This is the least time-intensive level of care, usually requiring just one or two sessions a week for a few hours total. It’s built for people who already have a solid foundation in recovery but need ongoing support to keep their momentum.
An SOP often works as a "step-down" for someone who has just finished a more structured program, like residential treatment or an IOP. It's also a great fit for individuals with a less severe substance use disorder who have a strong, reliable support system at home. The main focus here is on preventing relapse, managing life’s ongoing stressors, and reinforcing the coping skills you've already learned.
Intensive Outpatient Programs (IOP)
Stepping up the intensity, we have the Intensive Outpatient Program (IOP). An IOP offers a more structured and robust level of care, demanding a bigger time commitment—usually around 9 to 12 hours per week, spread across three or four days. This "part-time" approach lets you get a significant amount of therapy while still keeping up with daily responsibilities like work, school, or family.
IOPs are ideal for anyone who needs more support than a single weekly session can offer but doesn't require 24/7 supervision. Treatment is typically a blend of individual therapy, group counseling, and educational workshops. To get a better feel for how this works, you can learn more about what an intensive outpatient program entails in our detailed guide.
An IOP strikes a crucial balance. It provides the structure and accountability needed to build momentum in early recovery without completely removing you from the real-world environment where you'll ultimately apply your new skills.
The accessibility of these programs is a huge reason they're so common. The infographic below shows the core therapeutic elements that form the foundation of most outpatient services.
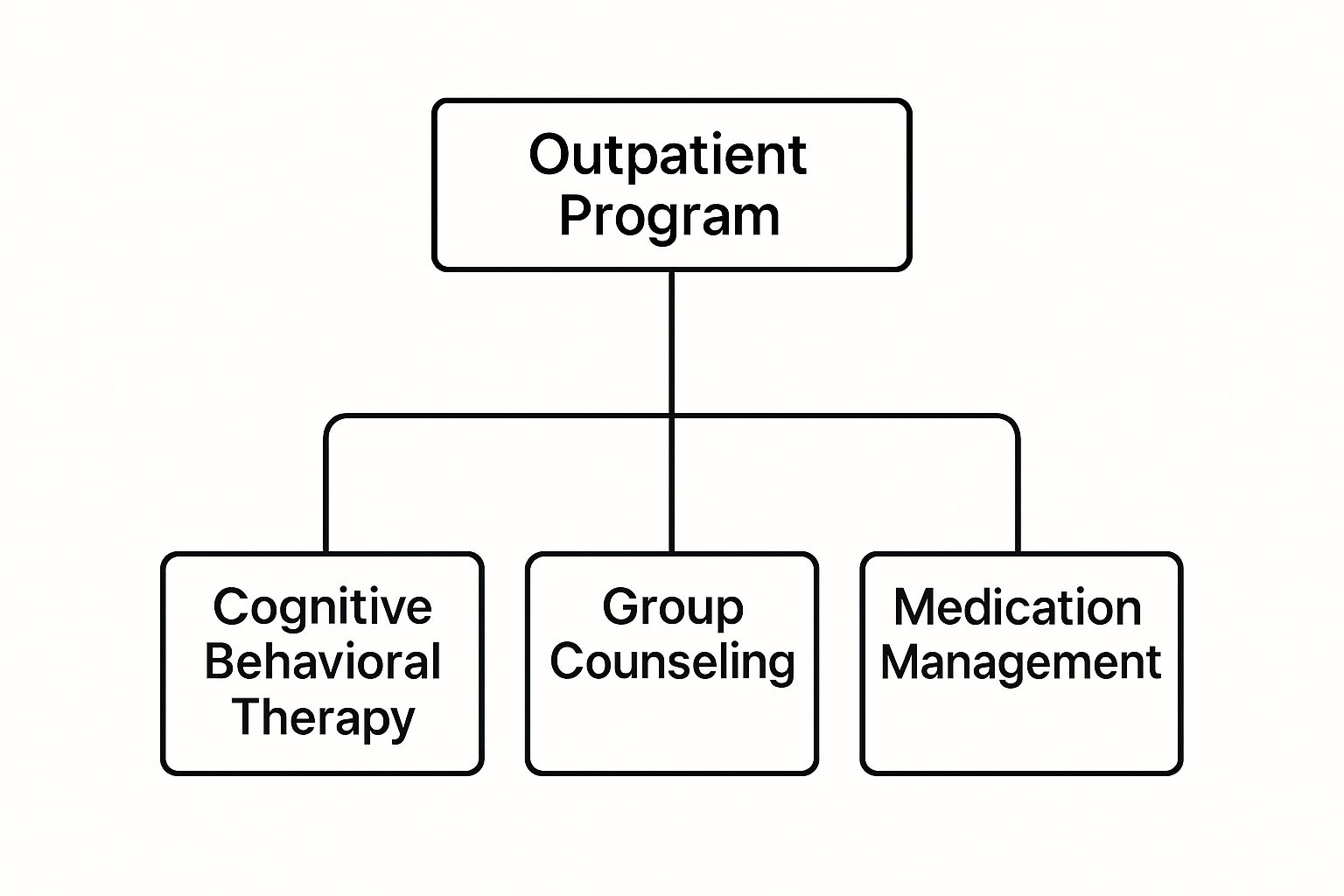
This visual breaks down how different evidence-based methods come together to create a well-rounded treatment plan, tackling both the psychological and behavioral sides of addiction.
Partial Hospitalization Programs (PHP)
At the highest and most intensive level of outpatient care is the Partial Hospitalization Program (PHP). Outside of a residential facility, this is the most structured option you can find. A PHP is basically a full-time job, requiring clients to be in treatment for 20 or more hours per week, usually five days a week.
PHPs are often the next step for people leaving inpatient care, or for those who need a high level of support to prevent relapse but have a safe, stable home to return to each night. This level provides a highly structured environment with daily access to medical and clinical staff, extensive therapy, and a full suite of support services. It’s a powerful way to build an incredibly strong foundation for long-term sobriety.
The good news is that these different levels of care are widely available, making treatment more accessible than ever. According to the 2020 National Survey of Substance Abuse Treatment Services, a remarkable 82% of treatment facilities offered some form of outpatient care.
Digging into the numbers, 76% of facilities provided standard outpatient services, while 45% offered IOPs. This makes these programs the most common form of addiction therapy out there. This data just underscores how an outpatient substance abuse program has become a mainstream, effective, and accessible solution for countless people seeking recovery.
The Core Components of Modern Outpatient Treatment
So, what actually happens inside an outpatient substance abuse program? Once you get past the different schedules and levels of care, you find the real engine of recovery: evidence-based therapies designed to tackle addiction from every possible angle. A modern program isn’t just about putting a stop to substance use; it’s about rebuilding the entire foundation for a healthier life.
Think of it like renovating an old house. You can't just slap a coat of paint over a cracked foundation and call it a day. You have to fix the underlying structure (your psychological health), rewire the electrical system (biological factors), and make sure the house fits into its neighborhood (your social environment). Effective outpatient treatment uses a whole toolbox of methods to repair each of these critical areas.
These programs are built on a multi-faceted approach, blending different therapeutic models to create a plan that fits the individual. The goal is to give you a complete toolkit of coping strategies, emotional regulation skills, and a strong support network. Let's break down the essential components that make this possible.
Individual Counseling: The Personal Blueprint for Recovery
Individual therapy is the cornerstone of personalized care. In these one-on-one sessions, you work directly with a licensed clinician to dig deep into the personal roots of your substance use. It's a completely confidential, safe space to explore sensitive topics that might be too tough to bring up in a group setting.
A huge focus here is on identifying your personal triggers—the specific people, places, emotions, or situations that kick off cravings. For example, a stressful work deadline or a fight with a family member might be a major trigger. Your therapist helps you develop concrete, healthy coping mechanisms to navigate these moments without turning back to old habits.
These sessions also provide a crucial space to address co-occurring mental health conditions like anxiety, depression, or PTSD. When substance use and mental health issues are tangled together, treating both at the same time is essential for a recovery that actually lasts. You can learn more about how outpatient programs support clients by exploring a dual diagnosis outpatient treatment plan.
Group Therapy: The Power of Shared Experience
While individual therapy helps you build self-awareness, group therapy builds community and perspective. In a professionally facilitated group, you connect with peers who genuinely get what you're going through because they’re walking a similar path. That shared experience is incredibly powerful, breaking down the profound isolation that so often comes with addiction.
But group sessions are more than just sharing stories; they're structured workshops focused on building specific skills.
- Relapse Prevention: Groups work together to brainstorm strategies for handling high-risk situations, from a holiday party to an unexpected life crisis.
- Communication Skills: You'll practice healthy ways to express your needs and set boundaries, which can be a game-changer for repairing relationships damaged by addiction.
- Emotional Regulation: You learn practical techniques like mindfulness and distress tolerance to manage difficult feelings constructively.
Hearing others' successes and setbacks provides validation and hope. It’s a powerful reminder that you are not alone and that recovery is a collective journey, not a solitary battle.
"In group therapy, you realize your story is not unique in its pain, but your recovery can be unique in its strength. It’s where you borrow hope from others until you can generate your own."
Medication-Assisted Treatment: The Biological Support System
For many people, addiction has a strong biological component that therapy alone can't fully solve. Medication-Assisted Treatment (MAT) is a science-backed approach that combines behavioral therapy with specific medications to treat substance use disorders. It's especially effective for opioid and alcohol use disorders.
MAT isn't about trading one drug for another. Instead, these FDA-approved medications work to normalize brain chemistry, block the euphoric effects of substances, relieve cravings, and manage withdrawal symptoms. This biological stability is what allows you to engage more fully in therapy and focus on the psychological work of recovery.
The Substance Abuse and Mental Health Services Administration (SAMHSA) makes it clear how these medications support the recovery process.
This graphic highlights that medications are a key part of a comprehensive plan, used alongside counseling to create a whole-person approach to healing. When cravings and withdrawal are under control, you finally have the mental space you need to build new, healthy habits and address the root causes of addiction.
Why Outpatient Programs Are a Powerful Choice

Choosing an outpatient substance abuse program isn't just about convenience. While the ability to sleep in your own bed is a huge plus, the real power of this model runs much deeper. It’s built on a simple but profound idea: your life doesn't have to stop just because your recovery is starting.
Instead of pulling you out of your world, outpatient care is designed to weave recovery skills directly into the fabric of your daily routine. This integration is what makes it such a potent and practical choice for so many people. It means you can keep your career on track, stay connected to your family, and manage real-world responsibilities while building a rock-solid foundation for sobriety.
Affordability and Accessibility
Let’s be practical: one of the biggest hurdles to getting help is often the cost. Outpatient treatment tackles this head-on. By eliminating the huge expenses of room, board, and 24/7 staffing that come with residential care, outpatient programs become a far more affordable and accessible path to recovery.
This financial feasibility has made it a cornerstone of modern addiction treatment. In fact, outpatient services now make up the largest part of the global treatment market, driven by their cost-effectiveness and better insurance coverage. Market data shows this trend isn't slowing down, as providers and insurance companies alike recognize its value. You can dig into the numbers on these global substance abuse treatment market trends to see for yourself.
Maintain Your Life and Your Privacy
For most people, stepping away from work, school, or family for a month or more just isn't an option. Outpatient programs remove that barrier entirely. You get the intensive help you need without having to put your entire life on pause.
This structure also offers a much-needed layer of privacy. You can schedule therapy sessions in the evening or on weekends, fitting treatment discreetly into your life. There’s no need to explain a long absence to your boss, coworkers, or neighbors, which reduces a ton of stress and lets you focus completely on getting well.
The real magic of outpatient care is that it turns your daily life into the training ground for recovery. Every challenge becomes an opportunity to apply new skills in real time.
Putting Recovery Skills to the Test—In Real Time
This is where an outpatient substance abuse program really proves its worth. Residential treatment is like a controlled lab—a safe bubble where you can learn new coping skills. But outpatient care is where the rubber meets the road, forcing you to use those skills immediately in the unpredictable environment of your actual life.
Think of it like learning to swim. You start in the calm, predictable water of a pool. That’s essential. But eventually, you have to learn how to handle the choppy, unpredictable waves of the ocean. Outpatient treatment is your guide in the ocean, teaching you how to navigate the real-life currents of stress, temptation, and social pressure.
- Handling Work Stress: A brutal day at the office? You can process those specific stressors in group therapy that very evening, getting immediate feedback and strategies you can use tomorrow morning.
- Navigating Social Events: You might learn refusal skills in a session on a Thursday, then put them into practice at a family barbecue that Saturday. You turn a high-risk situation into a concrete win.
- Repairing Relationships: The communication tools you gain in family therapy aren't just theoretical. You can try them out at the dinner table with your loved ones that same week.
This constant cycle of learning, applying, and getting feedback builds a kind of recovery that is resilient, practical, and deeply personal. It’s not an academic exercise; it's a lived experience. To support this hands-on approach, many programs incorporate different therapeutic tools; our guide explaining what Medication-Assisted Treatment is shows how it can fit into this real-world recovery process. This practical application builds true confidence, proving to yourself, day by day, that you have what it takes to build a fulfilling life in sobriety.
Weaving Recovery into Your Real Life
Making an outpatient program work isn’t about cramming another appointment into your already packed schedule. It's about fundamentally reshaping your daily life so that recovery becomes a natural, integrated part of your routine—not just another chore on your to-do list.
Think of it like this: you’re not just attending meetings, you’re building a personal ecosystem that nurtures sobriety. This means getting practical and intentional about how you manage your time, communicate your needs, and lean on a support network that extends far beyond the therapy room.
When you do this well, the skills you learn in treatment stop feeling like homework and start becoming second nature. You’re not just doing recovery; you’re living it.
Give Your Day a Backbone
In the shaky first months of recovery, routine is your best friend. A predictable schedule acts as an anchor, cutting down on decision fatigue and leaving less mental space for old, destructive habits to sneak back in.
This doesn’t mean your day has to be rigid or mapped out to the minute. It’s simply about creating a framework that supports your well-being.
- Own Your Morning: Before the world starts making demands, claim the first 10 minutes for yourself. A short meditation, a quick walk, or just jotting down your thoughts can set a calm, centered tone for the rest of the day.
- Schedule Your Downtime: Burnout is a massive relapse trigger. If you don't intentionally block out time to rest and recharge, it won't happen. Put "do nothing" on your calendar and treat it like a doctor's appointment.
- Create an Evening Wind-Down: Shut down the screens and give your brain a chance to switch off. Reading a book or listening to quiet music helps improve your sleep, which is non-negotiable for keeping your emotions and mental health on an even keel.
By building this structure, you’re creating a life that actively defends your sobriety instead of one that constantly tests it.
Learn to Use Your Voice: Needs and Boundaries
A huge part of weaving recovery into your life is learning how to talk to the people in it—your family, your boss, your friends. This means getting clear about what you need and setting firm boundaries to protect your progress. It’s awkward at first, but it's absolutely essential.
This could be as simple as telling your friends you can't hit the bar on Friday but suggesting a coffee run on Saturday morning instead. Or it might mean asking your partner to keep alcohol out of the house for a while.
Healthy boundaries aren't walls you build to keep people out. They are fences you put up to protect the space you need to heal. They’re a sign of self-respect, and you can’t have lasting recovery without them.
These conversations take courage, but they put you back in the driver's seat. You start shaping your environment to support your goals, rather than letting your environment dictate your choices.
Build Your Team Beyond Therapy
While your therapy sessions are the heart of your treatment, a strong support system outside of your outpatient substance abuse program is just as vital. These are the people who offer encouragement and accountability when you need it most, reminding you that you're not on this journey alone.
Many people find that mutual support groups are the perfect complement to formal treatment, reinforcing the principles you’re learning in a real-world setting.
- 12-Step Programs: Groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) have been around for decades for a reason. They offer a time-tested, peer-driven path to sobriety based on a set of guiding spiritual principles.
- Alternative Groups: If the 12-step model doesn't resonate, organizations like SMART Recovery or Refuge Recovery provide secular, evidence-based approaches that focus on cognitive skills, self-empowerment, and mindfulness.
Plugging into these groups gives you a safe space to talk through your struggles and celebrate your wins with people who truly get it. This external support system becomes a powerful safety net, helping you navigate life's inevitable curveballs while strengthening your commitment to staying sober for good.
How to Find the Right Outpatient Program

With so many options out there, choosing the right outpatient substance abuse program can feel overwhelming. But finding a program that genuinely fits your life, your needs, and your goals is the single most important step you can take toward building a recovery that lasts.
This isn't about finding the "best" program in a generic sense. It's about finding the best fit for you. Think of it like hiring a guide for a tough expedition. You wouldn’t just pick anyone; you'd want someone with the right experience, credentials, and tools to help you navigate the specific terrain you're about to face. By taking a methodical approach, you can turn a daunting choice into a clear, manageable process.
Vetting Potential Programs
Before you commit to anything, it's time to do some homework and ask direct questions. A quality provider will be transparent and happy to give you the information you need to feel confident in your decision. Arm yourself with a checklist so you know you've covered all the critical bases.
Here are the key areas to dig into:
- Accreditation and Licensing: Is the facility licensed by the state? Is it accredited by a respected body like The Joint Commission or CARF? These credentials are the baseline for quality and safety.
- Staff Qualifications: Who will be guiding your recovery? Look for licensed professionals like therapists (LCSW, LPC), psychologists, and medical doctors who specialize in addiction medicine.
- Therapeutic Models: What specific evidence-based therapies do they use (e.g., CBT, DBT, EMDR)? Does their philosophy align with what you need, especially if you're dealing with a dual diagnosis for co-occurring mental health conditions?
- Insurance and Cost: Does the program take your insurance? Ask for a clear, upfront breakdown of all costs, including co-pays and any out-of-pocket expenses. Financial surprises are the last thing you need.
A program’s willingness to openly discuss its methods, staff credentials, and costs is a strong signal of its integrity and commitment to client care. Don't hesitate to ask for specifics.
Where to Find Trusted Providers
The good news is you don't have to do this search alone. Several reliable resources can point you toward reputable programs in your area and help you start the vetting process.
A great first step is to talk with trusted professionals who already know your health history. Your primary care physician or a mental health therapist can often provide referrals to programs they know and trust.
Additionally, government-backed resources offer impartial guidance. The Substance Abuse and Mental Health Services Administration (SAMHSA) runs a National Helpline (1-800-662-4357) that provides free, confidential treatment referrals 24/7.
This growing network of providers reflects a simple truth: more and more resources are becoming available. The global addiction treatment market was valued at about USD 9.44 billion in 2024 and is projected to hit over USD 16.22 billion by 2034, partly thanks to government initiatives promoting these vital services. You can learn more about the growth in addiction treatment services and what it means for people seeking help. Taking these steps equips you to select a program that will truly support your journey to lasting freedom.
Have Questions? Let's Get Them Answered
Stepping into the world of recovery can feel like learning a new language. It’s completely normal to have a lot of questions. Here are some straightforward answers to the things people most often ask when considering an outpatient program.
Is Outpatient Treatment the Right Choice for Me?
The only way to know for sure is to get a professional clinical assessment, but we can give you some solid guideposts. Outpatient treatment tends to be most successful for people who have a stable, supportive home life. It’s a great fit if you don’t require a medically supervised detox or 24/7 monitoring to stay safe.
Think of it this way: if your home is a safe harbor, outpatient care helps you navigate the waters of daily life while always having that harbor to return to.
On the other hand, if you’ve struggled with frequent relapse or your living situation is unstable, a higher level of care like an inpatient program might be a better starting point. Motivation is also a huge factor—since you’ll be living at home, your personal commitment is the engine that drives your recovery forward.
Will My Insurance Cover an Outpatient Program?
Yes, in most cases. The vast majority of major health insurance plans cover outpatient substance abuse treatment. In fact, insurers often prefer it because it’s more cost-effective than residential care.
But—and this is a big but—the details of your coverage can vary wildly. Your copays, deductible, and the number of sessions your plan will approve all depend on your specific policy.
Crucial next step: Before you commit to any program, you absolutely must contact your insurance provider directly. Better yet, have the treatment center’s admissions team verify your benefits for you. This one step will save you from surprise bills and give you a clear picture of your financial responsibility.
What Happens After I Finish an Outpatient Program?
Graduating from a program is a huge milestone, but it’s the beginning of a new chapter, not the end of the book. Recovery is a lifelong journey. A good outpatient program won’t just hand you a certificate and say goodbye; they'll work with you to build a detailed aftercare plan. This is your personal roadmap for staying sober for the long haul.
This plan is all about creating a safety net so you never feel like you’re on your own. It usually includes things like:
- Stepping down to a less intensive level of care, like moving from an IOP to one weekly therapy session.
- Connecting you with an individual therapist for continued one-on-one support.
- Providing recommendations for support groups like AA, NA, or SMART Recovery to help you build a sober community.
- Giving you access to an alumni network for ongoing encouragement from people who’ve walked the same path.
The goal here is simple: to make sure you have a web of support to catch you. This structured follow-up is what helps turn short-term progress into lasting, confident recovery.
At Altura Recovery, we know that no two recovery journeys are the same. Our team is here to create a personalized plan that fits your life, meets your needs, and empowers you to build a solid foundation for a sober future. If you’re ready to see what that could look like, contact Altura Recovery today and let’s talk.