Staging an intervention is one of the most loving, and most difficult, things you can do for someone. It’s a carefully planned conversation designed to help a person you care about finally see the impact of their self-destructive behavior and, most importantly, accept professional help.
This isn't a surprise attack or a chance to vent. It's a structured, empathetic process focused on one thing: connecting your loved one with a pre-arranged treatment plan that can save their life.
What a Modern Intervention Really Looks Like
Before we get into the "how-to," we need to get rid of the dramatic images from TV and movies. An effective, modern intervention isn't about shame, ambushes, or guilt trips. It’s a thoughtful, loving process designed to break through the walls of denial and guide someone toward help.
The goal is to present a unified, supportive front that clearly communicates two things: profound love and serious concern. It’s a structured meeting where family and friends come together to share, one by one, how the person’s substance use has personally affected them. Think of it as a chorus of voices speaking with a single, clear message—we love you, we are worried, and we have a solution ready for you right now.
Shifting from Confrontation to Compassion
The old model of intervention was often harsh and confrontational, which we now know can backfire. Today, the focus has shifted dramatically toward compassion.
The foundation of this approach is understanding addiction as a treatable illness, not a character flaw. It's a medical issue requiring professional care, just like diabetes or heart disease. Framing it this way removes blame and opens the door for a real conversation.
This compassionate approach is built on a few key elements:
- Empathy and Validation: Acknowledging the person's pain without condoning their behavior.
- Factual Examples: Using specific, non-judgmental "I" statements. For example, "I felt scared when you drove after drinking last Tuesday."
- Pre-Arranged Help: Having a treatment plan ready to go removes any barriers to them saying "yes."
- Unified Support: Showing that everyone in the room is there out of love and is committed to a positive outcome.
To help you understand the different ways an intervention can be structured, here's a quick look at some common approaches.
Intervention Approaches: A Quick Comparison
While every intervention is unique, most follow an established model. Understanding the options helps you and your professional guide choose the best fit for your family's situation.
| Approach Type | Key Characteristic | Best For |
|---|---|---|
| Johnson Model | A surprise meeting where the person is confronted by loved ones with pre-written letters. | Individuals deep in denial who are unlikely to attend a pre-planned meeting. |
| Systemic Model | The whole family, including the person with the SUD, meets with a therapist to address group dynamics. | Families where communication breakdowns and enabling are significant contributing factors. |
| ARISE Model | A gradual, invitational process that involves the person from the start, with no surprises. | Individuals who may be open to discussion but are resistant to being confronted. |
Each style has its place, but they all share a common goal: to guide the person toward accepting help in a supportive, structured way.
Why a Structured Approach Works
Spontaneous, emotional pleas rarely lead to lasting change. A well-planned intervention, on the other hand, organizes love and concern into a powerful force. This structured process involves careful planning among family, friends, and—ideally—a professional interventionist.
The data backs this up. With professional guidance, 70-80% of interventions successfully lead to the person accepting help. That success rate can plummet to as low as 40-50% for interventions attempted without an expert, which really highlights the value of having a professional in your corner. For more on this, you can dig into findings on structured interventions at Nature.com.
A successful intervention isn't just a single event. It's the first deliberate step in a long-term healing journey for the entire family. It lays the groundwork for recovery by establishing healthy boundaries and offering a clear path forward.
Ultimately, staging an intervention is about creating a moment of clarity so profound that it becomes easier for your loved one to accept help than to continue down their current path. It is an act of collective courage, fueled by love and hope.
Building Your Compassionate Intervention Team
The power of an intervention doesn't come from a crowd; it comes from a unified, supportive team. Putting together the right group of people is one of the most important things you'll do. This isn't about overwhelming your loved one. It's about creating a small, focused circle that can deliver a loving but firm message of support.
The sweet spot for an intervention team is usually between four and six people. Any smaller, and the message might not carry enough weight. Any larger, and your loved one is likely to feel ambushed, which can trigger a defensive reaction and shut the whole conversation down before it even starts.
Who Should Be on the Team?
You want people who have a close, meaningful relationship with your loved one—individuals whose opinions they respect and whose presence clearly says, "I am here because I care about you." As you think about who to ask, look for a few key qualities.
- A Calm Demeanor: Everyone involved must be able to keep their own emotions in check. This is not the time for tears, angry accusations, or rehashing old arguments.
- A Commitment to the Goal: Every single person must be on the same page, fully dedicated to the goal of getting your loved one into a pre-arranged treatment program.
- A Strong Relationship: Think about the people your loved one truly trusts and values. This often includes a spouse, parent, adult child, sibling, or a very close, long-term friend.
When you approach potential members, be direct and honest. Explain that you're organizing a structured, loving meeting to help, and that their voice is important. Be clear about their role: to share specific, personal examples of how the substance use has affected them and to back the unified request for treatment.
Who You Should Not Invite
Deciding who not to include is just as critical as choosing who to invite. This can be a tough and delicate process, but it’s essential for protecting the focus and integrity of the meeting.
You should avoid inviting anyone who:
- Has an Unmanaged Substance Use Issue: Their presence could completely undermine the message.
- Is Prone to Anger or Unpredictability: High-voltage emotions can easily derail the entire process.
- Might "Cave" or Back Out: The team absolutely must present a united front. No exceptions.
- Historically Enables the Behavior: This person may instinctively try to "rescue" your loved one from the difficult conversation, sabotaging the effort.
It's often a smart move to bring in a professional interventionist to help navigate these tricky family dynamics. They provide an objective perspective that can be a game-changer.
For instance, the Association of Intervention Specialists (AIS) is a great resource for finding certified professionals in your area.

Organizations like AIS offer directories and credential verification, helping you find a qualified expert to guide your team and ensure the intervention is structured for the best possible outcome.
Aligning on a Single Goal
Once you have your team, the next step is getting everyone perfectly aligned. The main goal isn't just to talk about the problem; it's to present a clear, immediate solution. This is why having a treatment plan ready to go is non-negotiable.
The strength of an intervention lies in its unity. Every person in the room must share the same script: "We love you, we are concerned, and we have a path to help you that can start today." Any deviation from this message can create an opening for refusal.
The group has to agree on both the treatment plan and the specific boundaries that will be enforced if your loved one refuses help. This collective agreement is what transforms individual worries into a powerful, unified call to action. It can also be helpful for the team to understand the differences between individual therapy vs. group therapy, as this gives everyone more context for the recommended plan. Preparing together ensures your compassionate team is ready to offer a true lifeline.
Why You Should Hire a Professional Interventionist
Trying to stage an intervention on your own can feel like trying to direct a play where every actor has gone off-script. Even with the best intentions, the raw emotion, tangled family history, and high stakes can quickly spiral out of control. This is exactly where a professional interventionist steps in—not as a judge, but as a skilled and objective guide.
Hiring an expert isn't about admitting you've failed; it's a strategic move to give your loved one the absolute best chance at saying "yes" to help. An interventionist is trained to navigate these emotionally charged conversations, de-escalate conflict, and keep everyone focused on the one thing that matters: getting your loved one into treatment.

The Role of an Intervention Specialist
A certified interventionist does so much more than just lead the meeting. Their work starts weeks before and often continues long after, creating a supportive framework for the entire family. They handle the clinical and logistical heavy lifting so you can focus on communicating love and concern.
Here’s what they actually do:
- Clinical Assessment: They start with a deep dive into your loved one’s history of substance use, any co-occurring mental health issues, and the family dynamics at play. This isn't just a formality—it's how they determine the right level of care.
- Team Coaching: The interventionist becomes your coach. They'll work with the group to help you write impactful letters, practice how you'll read them, and get everyone aligned on the boundaries you're going to set.
- Logistical Legwork: They take care of the behind-the-scenes details that can easily trip families up, like vetting and choosing the right treatment center, coordinating travel, and handling the admissions process.
- Meeting Facilitation: On the day of the intervention, they are the calm center of the storm. They guide the conversation, manage emotional flare-ups, and make sure the meeting achieves its goal without getting derailed by anger or blame.
In short, they provide the structure and clinical expertise that a family, caught in the emotional whirlwind of addiction, simply can't provide for itself.
Finding a Qualified Professional
It's critical to know that not all interventionists are created equal. You want to find a certified professional with real-world experience. The gold standard in this field is the Certified Intervention Professional (CIP) credential, which is managed by the Pennsylvania Certification Board. This certification means the person has met strict requirements for experience, ongoing education, and ethical practice.
A professional interventionist isn't just a facilitator; they are a clinical strategist. They understand the psychology of addiction and denial, allowing them to anticipate reactions and steer the conversation toward a positive resolution.
A great place to start your search is with organizations that vet their members, like the Association of Intervention Specialists (AIS). They maintain directories of qualified professionals. When you start making calls, have your questions ready.
Questions to Ask a Potential Interventionist:
- What are your credentials, specifically are you a CIP?
- What intervention model do you typically use and why is it a good fit for our situation?
- Can you share your experience with cases involving the specific substances our loved one uses?
- What does your preparation process for the family look like?
- How do you go about selecting and recommending a treatment facility?
- What does your fee cover, and what are your payment terms?
- What happens after the intervention? What kind of support do you offer the family?
Viewing the Cost as an Investment
Hiring a professional interventionist can cost anywhere from a few thousand to over $10,000, based on their experience, the complexity of the case, and any travel involved. It’s a significant number, and it's easy to get sticker shock.
But it’s crucial to see this as an investment, not just an expense.
Think about the staggering ongoing cost of addiction—the lost jobs, the legal bills, the emergency room visits, and the constant emotional toll on everyone. A successful intervention that gets your loved one into treatment can stop that financial and emotional bleed.
When a life is on the line, the guidance of a professional is priceless. Their expertise not only dramatically increases the odds of your loved one accepting help but also helps your entire family start its own healing journey, often by connecting you with resources like finding the right substance abuse therapy near you. This professional support creates a stable foundation for everyone to begin recovering.
Writing Your Letter with Love and Boundaries
The letters read during an intervention are its heart and soul. This isn't the time for off-the-cuff remarks or emotional outbursts. Each message needs to be a deliberate, thoughtful expression of your love, your deep concern, and your unshakeable resolve.
Crafting this letter is about turning your fear and pain into a clear, compassionate call to action. The goal is simple: be honest without being accusatory and firm without being punishing. The right words can open a door that’s been slammed shut for a long time, creating a moment of clarity for the person you care about.
Structuring Your Message for Impact
To keep your letter focused and effective, it’s best to follow a simple four-part structure. This framework helps you cover all the essential points while keeping the message grounded in love and fact-based concern. Think of it as a roadmap for a conversation you’ve probably wanted to have for months, if not years.
Your letter should flow through these four elements, in this order:
- Start with Love. Before you get into the hard stuff, affirm your love and appreciation for the person. Mention a specific positive memory or a quality you admire. This reminds them—and you—of the person you know and care for underneath the addiction.
- Express Specific Concern. State your worry directly, but always use "I" statements. Instead of saying, "You are destroying your health," try, "I am so worried about your health." This shifts the focus from accusation to your personal feelings.
- Share Factual Examples. This is the core of your letter. Provide two or three specific, undeniable examples of how their substance use has negatively impacted you. Stick to the facts, not judgments.
- State Your Boundary. Clearly and calmly state the action you will take to protect yourself if they refuse help. This is the consequence, your "bottom line." It’s not a threat; it’s a promise to yourself.
This structure moves the conversation away from blame and toward a productive dialogue about the reality of the situation. It’s a powerful way to show you mean what you say.
Your letter is not a list of grievances. It is a carefully constructed message designed to break through denial by combining heartfelt love with undeniable facts and a clear, non-negotiable boundary.
What to Say and What to Avoid
The language you choose is critical. Your tone should be loving, but your message has to be firm. Let's look at some real-world examples to see how this works in practice.
Effective (What to Say):
- "I will always remember our hiking trip in the mountains, and I miss that version of us. It’s why I’m so scared when I see how much alcohol is controlling your life now."
- "Last Tuesday, when you didn't pick up the kids from school, I felt terrified and alone. I had to leave an important work meeting to rush over there."
- "If you decide not to accept the help we've arranged today, I will no longer be able to let you stay in our home. I love you, but I cannot continue to watch this happen."
Ineffective (What to Avoid):
- "You're a completely different person now. You're ruining our family." (This is blaming and shaming.)
- "You're always drunk, and you never think about anyone but yourself." (This is a generalization and an attack.)
- "If you don't go to rehab, you'll never see your kids again!" (This is a threat, not a boundary.)
Remember to stick to the facts. Avoid dramatic language, generalizations like "always" or "never," and any statements that could be twisted into a personal attack. This approach makes your message much harder to argue with.
The Power of Healthy Boundaries
The final part of your letter—the boundary—is often the hardest to write and enforce, but it is absolutely non-negotiable. A boundary is not a punishment or a threat. It is a loving action you take to protect your own well-being and to stop enabling the addiction. A critical part of any successful intervention is establishing clear and compassionate healthy relationship boundaries.
Enabling behaviors, which often come from a place of love, actually shield the person from the natural consequences of their actions. This just allows the addiction to continue. Stating a clear boundary is how you lovingly step out of the way so they can finally feel the full weight of their choices.
Common boundaries might include:
- No longer providing financial support.
- Asking the person to move out of the house.
- No longer making excuses for them to employers or friends.
- Refusing to allow substance use in the home.
For families struggling with this, our guide on how to help an alcoholic husband offers deeper insights into setting these crucial limits. The key is that every single person on the intervention team must be 100% committed to upholding their stated boundary if your loved one refuses treatment. This unity is what gives the intervention its strength and creates the powerful motivation needed for change.
Navigating the Day of the Intervention
All the planning, letter writing, and rehearsals have led you to this moment. The day of the intervention will almost certainly be emotionally charged, but your solid plan is the anchor that will keep the environment calm, focused, and loving. That’s the atmosphere that gives your loved one the best possible chance to finally accept help.
Success today really boils down to managing the small details and staying committed to the process you've built together.
Setting the Stage for a Calm Conversation
The physical space you choose is critical. It needs to be neutral, private, and completely free from distractions. A family home can work, but only if it feels safe and not like anyone's "territory." Often, an interventionist's office or even a trusted friend's quiet living room is a better choice. Make sure all phones are off—not just on silent—and that there are zero potential interruptions.
Getting your loved one to the location without making them suspicious is a delicate art. The goal is to have them arrive without feeling ambushed. A common and effective strategy is to have one trusted person—someone they won't suspect, like a parent or spouse—invite them under a plausible pretext.
For example, you could say, "I really need to talk with you about something important with the family. Could you meet us at Aunt Susan's at 10 AM?" The key is being honest about the meeting's seriousness without revealing the exact format.
Everyone else on the team should plan to arrive 30-45 minutes early. This gives you all time to settle in, run through the plan one last time, and get centered emotionally before the main event.
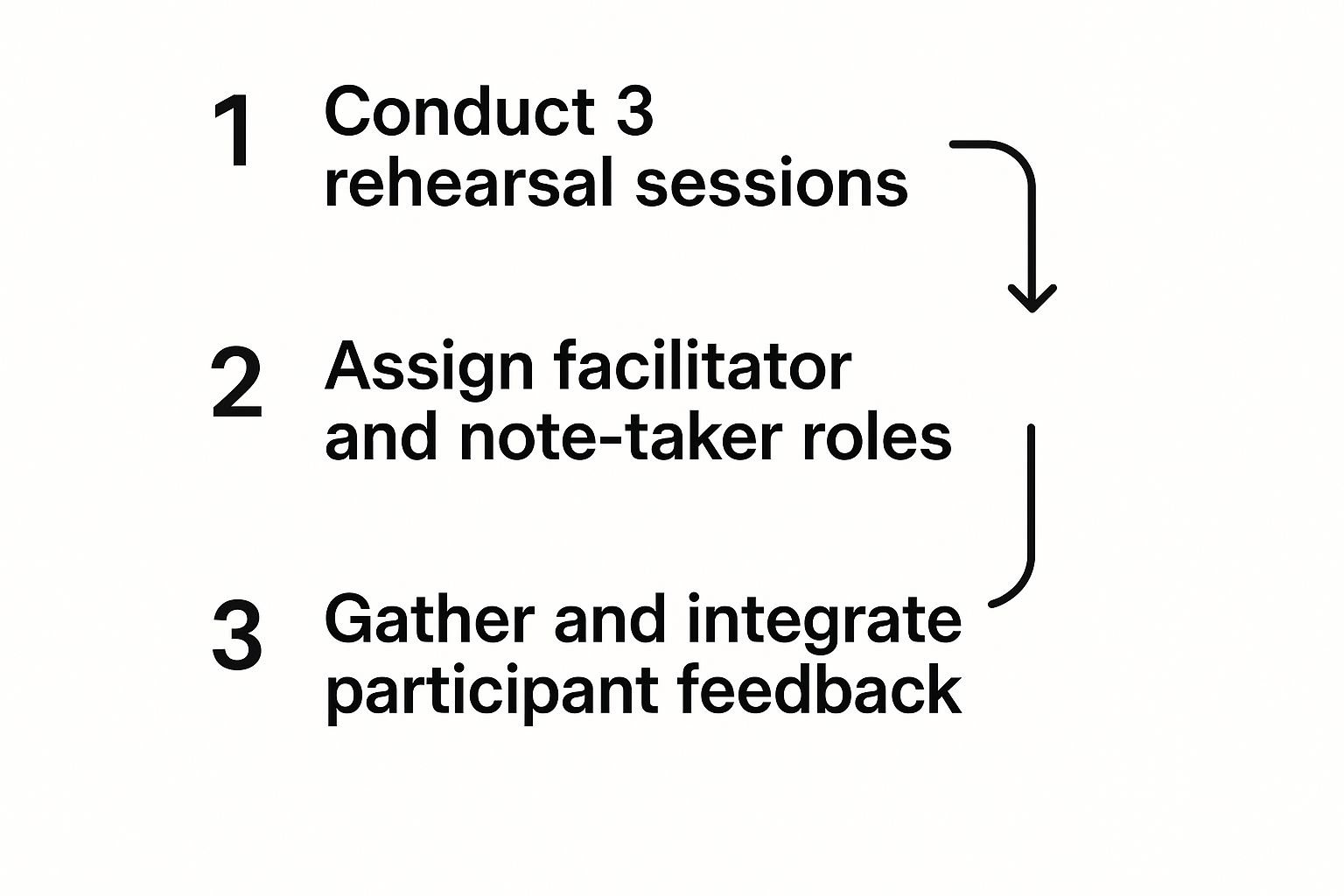
This final prep time is all about reinforcing the structure you've created. Running through the order of speakers and reminding everyone of their roles ensures you are a unified, calm front when your loved one walks in the door.
The Flow of the Meeting
Once everyone is present, the intervention needs to follow the sequence you rehearsed. If you're working with a professional, they will guide this process. If not, your designated facilitator must be ready to keep the conversation on track and gently steer it back if it goes off-course.
The meeting will typically unfold like this:
- The Opening: The facilitator starts by explaining why everyone is there, making it clear that the gathering comes from a place of deep love and concern.
- Reading the Letters: One by one, each person reads their letter. This must be done calmly and without interruption. It is absolutely crucial that no one adds off-the-cuff remarks, gets drawn into arguments, or deviates from their script.
- The Treatment Offer: After the final letter, the facilitator formally presents the pre-arranged treatment option. This isn't a vague idea; it's a concrete plan. You should state the facility's name, explain that travel is already arranged, and confirm that a spot is waiting for them right now.
- The Decision: Your loved one is then asked a direct question: "Will you accept this offer of help?"
The power of a structured intervention comes from its focused, uninterrupted flow. Each letter builds on the last, painting a comprehensive picture of love and consequence that becomes very difficult to deny or argue with. Sticking to the structure is everything.
Handling Common Reactions with Grace
You can't predict exactly how your loved one will react, but you can prepare for the most common responses. Knowing what to expect helps the team remain calm and resolute instead of getting flustered.
- Denial: You'll likely hear things like, "It's not that bad," or "You're all blowing this out of proportion." The right response is to gently redirect them back to the facts in your letters. Don't argue. Simply restate, "This has been my experience, and my concern for you is real."
- Anger: Lashing out is a classic defense mechanism. They might try to blame people in the room or start a fight to derail the entire meeting. The team cannot take the bait. Stay calm. Do not raise your voices. The facilitator should step in to de-escalate, saying something like, "We hear your anger, but we're here today because we love you."
- Bargaining: Expect promises. "I swear I'll cut back on my own," or "Just give me one more chance to prove I can handle it." The team's response here must be unified and firm: "We appreciate that you want to change, but we believe professional help is what you need right now." This is where holding the line is non-negotiable.
Throughout this entire process, your collective calm is your greatest tool. By remaining a focused, loving, and resolute team, you create a powerful moment of clarity. This supportive atmosphere makes it much easier for your loved one to see the path you're offering not as a punishment, but as the lifeline it is.
What Happens After the Intervention Ends

The silence after the final letter is read can feel immense. The intervention itself is a single, powerful moment, but the real work—for both your loved one and the family—begins the second it’s over. Your preparation for this next phase is just as important as the meeting itself.
Whether the answer is an immediate "yes" or a heartbreaking "no," the path forward requires clarity, resolve, and a commitment to follow through. The journey doesn’t end here; it simply takes a new direction.
When Your Loved One Says Yes
Hearing "yes" is a moment of profound relief and hope. However, this is also when you must act with swift and gentle efficiency. The window between acceptance and arrival at treatment is fragile, and hesitation can give second thoughts room to grow.
This is why having all logistics pre-arranged is non-negotiable.
- Transportation is ready. A car should be waiting to take them directly to the facility. This is not the time for "one last stop" or a detour that could derail the commitment.
- A bag is packed. Have a pre-packed bag ready with essentials like comfortable clothing, toiletries, and any necessary personal items. This removes a significant logistical and emotional barrier.
- The facility is on standby. The treatment center should have been notified and be expecting your loved one’s arrival. The admissions process should be ready to begin as soon as they walk through the door.
Your role in this moment is to be supportive and reassuring. Avoid celebrating as if a victory has been won; instead, convey calm confidence that they are making a brave and positive choice. This smooth, immediate transition is the bridge from their old life to the first day of their recovery.
When the Answer Is No
Hearing "no" is incredibly painful, but it is not a failure. It is, however, the moment your resolve will be tested the most. If your loved one refuses help, the focus must immediately shift to the boundaries that each team member clearly stated in their letter.
This is the hardest part of staging an intervention, but it is also the most critical.
Following through on your boundaries is not a punishment; it is the most loving action you can take. It ends the cycle of enabling and allows your loved one to finally feel the natural consequences of their addiction, which is often the catalyst for future change.
Enforcing boundaries must be done with love, not anger. You can say, "I love you, and because I do, I must follow through on what I said. The offer for treatment is always on the table when you are ready." There should be no negotiation, no bargaining, and no "one more chance."
Consistency among the entire team is essential. If one person wavers on their boundary, it undermines the entire effort and sends a mixed message. Upholding these new rules shows you are serious and creates a new, healthier dynamic for everyone involved.
To help you stay aligned, here is a quick-action checklist for the moments immediately following the intervention, based on the outcome.
Post-Intervention Action Plan
| Scenario | Immediate Action Steps | Long-Term Family Support |
|---|---|---|
| Loved One Says "Yes" | 1. Calmly initiate pre-arranged travel to the facility. 2. Contact the admissions team to confirm arrival time. 3. Provide the pre-packed bag. 4. Offer quiet, reassuring support without celebration. | 1. Attend family therapy sessions offered by the center. 2. Begin attending Al-Anon or Nar-Anon meetings. 3. Learn about the recovery process to prepare for their return. |
| Loved One Says "No" | 1. Calmly and lovingly restate your boundary. 2. End the meeting; do not engage in arguments. 3. Each team member must enforce their stated consequence immediately. 4. Leave information about the treatment center easily accessible. | 1. Hold firm on all boundaries, consistently. 2. Work with an interventionist or therapist on managing guilt. 3. Continue your own therapy and support group attendance. |
This table serves as a quick reference, but the emotional follow-through is where the real work lies. Staying united as a family, regardless of the path chosen, is paramount.
The Family's Healing Journey
Regardless of the outcome, the intervention marks a turning point for the family as well. Addiction impacts the entire family system, and your own healing must become a priority. You have been carrying an immense emotional weight, and it’s time to start setting it down.
Engaging in your own support system is not selfish; it’s necessary for long-term recovery for everyone.
- Family Therapy: Working with a therapist can help you process the experience and learn new, healthier ways of communicating and interacting.
- Support Groups: Organizations like Al-Anon or Nar-Anon provide a community of people who understand exactly what you’re going through. Sharing experiences can be incredibly validating and healing.
- Continued Education: Learning about the nature of addiction and recovery helps you become a more effective and compassionate support person. Exploring options like a local sober living near me can also provide insight into the structured environments that support long-term sobriety.
The intervention is the start of a new chapter. Whether your loved one is in treatment or you are learning to live with your new boundaries, the focus shifts to building a healthier future for yourself and your family, one step at a time.
Of course. Here is the rewritten section, crafted to sound natural and human-written, following the style of the provided examples.
What If It Doesn't Go According to Plan? Common Intervention Questions
Even the most carefully planned intervention comes with a dose of uncertainty. It's completely normal to have a few “what-if” questions running through your mind. Thinking through these possibilities ahead of time is one of the smartest things your group can do. It keeps everyone on the same page and ready to respond with calm, unified support, no matter which way the conversation turns.
What if My Loved One Says No to Treatment?
This is the number one fear, and for good reason—it happens. If they refuse to go, the single most important thing is for every person in the room to lovingly but firmly hold to the boundaries they wrote down in their letters.
This isn't about punishment. It's about breaking a painful cycle of enabling that has kept everyone stuck. A professional interventionist is invaluable here, helping you navigate the emotional fallout. They’ll remind you that sometimes, seeing these consequences become real is the very thing that nudges someone toward accepting help later on. The door to treatment should always, always be left open.
Responding to a "no" with firm, loving boundaries is not a failure. It is the successful execution of your plan, designed to protect your well-being and create the conditions necessary for your loved one to eventually choose recovery.
How Do We Choose the Right Treatment Center?
Trying to pick the right facility on your own can feel like throwing a dart in the dark. This is where your interventionist becomes your most critical resource. They’ll start by doing a deep dive to figure out exactly what your loved one needs.
The evaluation will look at a few key things:
- What substance are they using, and how severe is the dependence?
- Are there any co-occurring mental health issues, like depression or anxiety, that need to be addressed at the same time?
- What are the practical logistics, like insurance coverage and finances?
Because interventionists have working relationships with high-quality, reputable centers, they can cut through the noise and recommend a program with the right level of care and therapeutic style. This ensures a much better chance of a good fit from day one.
Is There Ever a Time When an Intervention Is a Bad Idea?
Yes, absolutely. A traditional intervention can be inappropriate, or even unsafe, in a few specific scenarios. You should seriously reconsider this approach if the person has a history of severe mental illness (like psychosis), is actively suicidal, or has a documented history of violence.
In these high-stakes situations, talking to a mental health professional or an interventionist beforehand isn't just a good idea—it's essential. They can help you figure out the safest way forward, which might mean using a completely different strategy to get your loved one the help they need without putting anyone at risk.
At Altura Recovery, we know that walking a family through this process is one of the most difficult—and important—things we can do. Our compassionate professionals are here to offer the clinical guidance and steady support you need to help your loved one find their way to healing. If you're thinking about an intervention, contact us to see how our evidence-based programs can build a foundation for a lasting recovery.








