Imagine rebuilding your life piece by piece, without having to press pause on everything that matters. That’s the heart of outpatient drug treatment. It’s less like a hospital stay and more like specialized coaching for recovery—you get structured, expert therapy during the day but head home each night to apply what you've learned in the real world.
What Is Outpatient Drug Treatment Really Like
Outpatient drug treatment is a flexible but powerful way to address a substance use disorder while keeping up with your daily life. Unlike inpatient or residential programs that require you to live at the facility 24/7, outpatient care weaves healing right into your existing routine. You attend scheduled therapy sessions and then return to your own home.
This setup is incredibly practical. It lets you immediately practice new coping skills in the situations where you’ll actually need them. You can continue working, going to school, or caring for your family while building a rock-solid foundation for sobriety. It’s an approach that balances structured support with personal freedom, opening the door to recovery for people who simply can't step away from their commitments.
A Practical Approach to Recovery
The whole idea is to provide robust clinical support without pulling you out of your own environment. This common-sense approach is why its popularity has exploded. In fact, outpatient drug treatment has become the leading model in the global substance abuse treatment market, projected to command over 52% of total revenue in 2025. This shift shows a clear preference for community-based care that lets people tackle addiction while keeping their lives intact. You can discover more insights on the substance abuse treatment market trends and see how care models are evolving.
But this isn’t a one-size-fits-all solution; it’s a spectrum of care designed to meet you exactly where you are. The core components almost always include:
- Individual Therapy: Private, one-on-one sessions with a licensed clinician to dig into personal challenges.
- Group Counseling: A supportive space to share experiences and gain perspective from peers on the same path.
- Family Workshops: Sessions designed to heal strained relationships and build a strong support system at home.
- Medication Management: Medical oversight for any prescribed medications that can support your recovery journey.
Outpatient vs Inpatient Treatment At a Glance
To really get a feel for the different models, it helps to see them side-by-side. The biggest differences come down to where you live, how intense the care is, and how much flexibility you have.
This table breaks it down.
| Feature | Outpatient Treatment | Inpatient Treatment |
|---|---|---|
| Living Situation | Live at home, attend scheduled sessions | Reside at the treatment facility 24/7 |
| Flexibility | High; can maintain work/school | Low; all focus is on treatment |
| Intensity | Varies (PHP, IOP, SOP) | High; round-the-clock supervision |
| Cost | Generally more affordable | Typically more expensive |
| Ideal Candidate | Strong support system, stable home | Needs medical detox, unstable environment |
Ultimately, one isn't "better" than the other—it's all about finding the right fit for your specific medical needs, life circumstances, and recovery goals.
Understanding the Levels of Outpatient Care
Outpatient drug treatment isn't a one-size-fits-all program. Think of it less like a rigid highway and more like a trail map with different routes to the same destination: a stable, healthy life. It’s a flexible system with different levels of support, designed to meet you exactly where you are in your recovery journey.
This "step-down" model ensures you're never overwhelmed or left without a safety net. As you build stronger coping skills and gain confidence, you can transition to a less intensive level of care. This is key to building a sustainable, long-term recovery that fits into your real life. Let's break down the main levels—often called by their acronyms PHP, IOP, and SOP—so you can see the full picture.
This diagram helps visualize how different treatment options, including outpatient and inpatient care, form a complete system of support.
As you can see, both paths fall under the umbrella of professional treatment, but outpatient care is structured around living at home. Now, let’s explore the distinct levels within that outpatient framework.
Partial Hospitalization Program (PHP)
The Partial Hospitalization Program (PHP) is the most intensive form of outpatient care available. It’s often the right choice for people who need significant structure but have a stable and supportive home environment, so 24/7 residential care isn’t necessary. It acts as a powerful bridge, offering near-inpatient intensity with outpatient flexibility.
A PHP typically involves:
- Daily Sessions: Treatment usually runs five to seven days a week.
- Significant Time Commitment: Expect to spend several hours each day, much like a full workday, in therapy and structured activities.
- Comprehensive Services: This includes individual therapy, group counseling, psychiatric evaluations, and medication management.
This level of care is ideal for those stepping down from an inpatient program or for individuals who need more support than a less intensive program can offer to prevent a relapse.
Intensive Outpatient Program (IOP)
Just one step down from PHP is the Intensive Outpatient Program (IOP). This is one of the most common and versatile levels of care, designed to balance a robust recovery schedule with daily responsibilities like work, school, or family life. It provides a ton of support without requiring a full-day commitment.
An IOP offers a solid therapeutic schedule, typically requiring at least nine hours of treatment per week, often spread across three to five days. This structure provides a strong safety net while allowing you to immediately apply your recovery skills in the real world.
In an IOP, you’ll dive into a variety of evidence-based therapies and group sessions. The schedule is often flexible, with many programs offering evening sessions to accommodate jobs and other obligations. This balance is exactly why outpatient treatment is an effective option for so many people—it lets you build a foundation for sobriety while still navigating everyday life.
Supportive Outpatient Program (SOP)
The Supportive Outpatient Program (SOP), sometimes just called standard outpatient, is the least intensive level. It’s an essential final step in the formal treatment process, laser-focused on maintaining long-term sobriety and preventing relapse. An SOP is perfect for individuals who have already completed a more intensive program and have developed solid coping skills.
Key features of an SOP include:
- Reduced Frequency: Sessions are less frequent, often just once or twice a week.
- Focus on Maintenance: The primary goal is to reinforce the skills you learned in PHP or IOP.
- Building Independence: It helps you confidently manage your recovery with less direct clinical oversight.
This final level provides ongoing accountability and connection as you fully reintegrate into your life. It ensures you have a consistent touchpoint with your support network while navigating the challenges of long-term sobriety, solidifying all the progress you’ve made.
The Core Therapies That Drive Real Change
Successful outpatient treatment isn’t just about putting a stop to substance use. It's about getting to the root of the problem—rewiring the thoughts, emotions, and behaviors that keep the cycle of addiction going in the first place. This is where evidence-based therapies come in. Think of them as the engines that power lasting recovery, giving you practical tools to build a new life from the inside out.
At the heart of any quality program, you’ll find specific, well-researched therapeutic models. These aren't just casual chat sessions; they are structured approaches designed to heal the mind and build resilience. It’s like having a toolkit for your mental and emotional health. A skilled mechanic uses different tools for different engine problems, and a skilled clinician uses various therapies to address the unique challenges of addiction.
A well-structured roadmap is key to any effective outpatient drug treatment, laying out the therapeutic journey ahead. For practical treatment plan examples that are tailored for substance abuse, it's always helpful to see how these plans are put together.
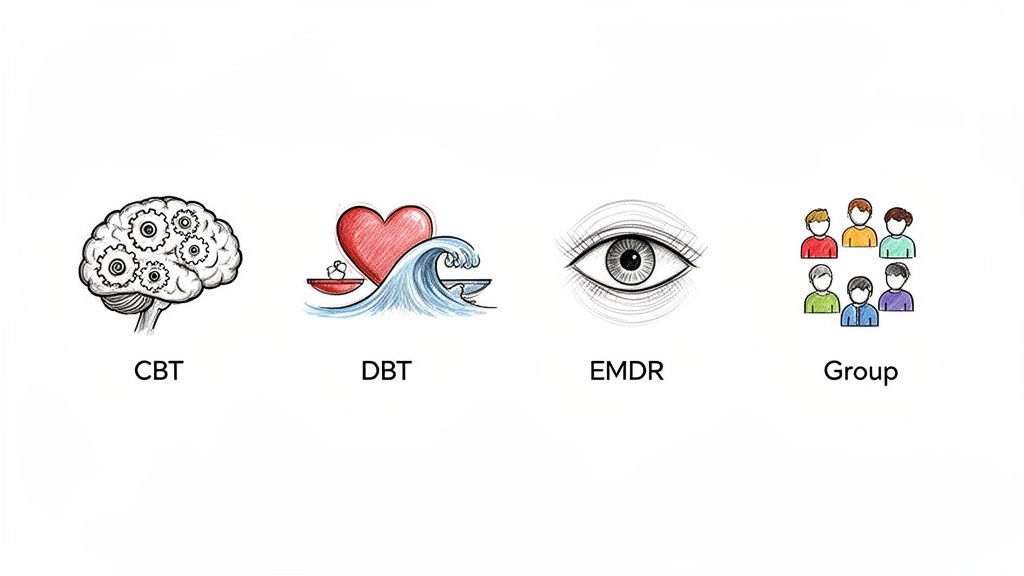
Let's break down the core methods you'll likely encounter.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a true cornerstone of modern addiction treatment. The core idea is simple but incredibly powerful: our thoughts, feelings, and actions are all connected. CBT helps you spot and challenge the negative or distorted thought patterns that lead directly to using substances.
Imagine your brain has created automatic shortcuts, like "If I feel stressed, then I need a drink to cope." CBT is all about interrupting that automatic process. Your therapist will guide you in recognizing those triggers, questioning the thought itself, and swapping it out for a healthier, more constructive response. It’s a very hands-on, practical way to change your behavior by first changing your mind.
Dialectical Behavior Therapy (DBT)
While CBT hones in on your thoughts, Dialectical Behavior Therapy (DBT) is brilliant at helping you manage overwhelming emotions. Many people turn to substances as a way to escape intense feelings of anger, sadness, or anxiety. DBT gives you concrete skills to navigate these emotional storms without turning to self-destructive behaviors.
DBT is built on four key modules:
- Mindfulness: Learning to stay present and simply observe your emotions without judging them.
- Distress Tolerance: Building skills to get through crisis moments without making things worse.
- Emotion Regulation: Understanding your emotions and reducing your vulnerability to the negative ones.
- Interpersonal Effectiveness: Fostering healthier relationships and learning to communicate your needs clearly.
This therapy is particularly effective for anyone dealing with co-occurring disorders, as it provides a solid framework for achieving emotional stability.
Eye Movement Desensitization and Reprocessing (EMDR)
Addiction and trauma are often deeply tangled together. Eye Movement Desensitization and Reprocessing (EMDR) is a specialized therapy designed to help the brain heal from traumatic memories that can act as powerful triggers for substance use.
Sometimes, traumatic memories get "stuck," causing the mind and body to relive the event over and over. EMDR uses bilateral stimulation, such as guided eye movements, to help your brain reprocess these memories and reduce their emotional power. It doesn't erase what happened, but it helps file it away correctly so it no longer controls your reactions today.
EMDR is a game-changer for those whose substance use is a way of coping with past pain. By healing the underlying trauma, it removes a primary driver of the addiction itself, paving the way for more profound and sustainable recovery.
The Power of Connection and Holistic Care
Beyond these individual therapies, a strong outpatient drug treatment program weaves in other vital services. Group therapy creates a safe space where you can share your experiences and realize you’re not alone, which helps reduce shame and build connection. Family counseling works to repair damaged relationships and create a supportive home environment—something that is absolutely crucial for long-term success.
Finally, many programs bring in holistic services like yoga, mindfulness, and nutritional counseling. These practices support your overall well-being, helping to heal the mind-body connection that addiction so often disrupts. Together, these therapies create a rich, supportive ecosystem that addresses every part of your health, building a solid foundation for real, lasting freedom.
Deciding between outpatient and inpatient care is one of the most important calls you'll make on the road to recovery. Outpatient drug treatment is a powerful option, but its success really depends on how well it lines up with your life, your needs, and your own motivation to get well. This isn't about which one is "better" in a general sense—it's about finding the right fit for you, right now.
Choosing this path is a bit like renovating your house while you're still living in it. It takes a ton of discipline and a solid foundation to build on. If your home life is stable and supportive, and you have that fire in your belly to make a change, this model can work wonders. It lets you weave healing into your daily world without having to press pause on your entire life.
To figure out if outpatient treatment is the right move, a professional evaluation is the essential first step. This process often includes a psychiatric assessment to get a clear, honest picture of your mental health and substance use history. This ensures the level of care you choose actually matches what you need to succeed.
Who Thrives in an Outpatient Setting
Some people are uniquely set up for the flexibility and structure of an outpatient program. Success in this environment usually means having a few key things already in place. Think of it like having the right scaffolding before you start building.
You might be a great candidate for outpatient care if these scenarios sound familiar:
- You Have a Stable Home Life: A supportive, safe place to live is the bedrock of a successful outpatient recovery. It gives you a secure base to return to after your daily sessions.
- You Possess Strong Internal Motivation: While outside support is huge, your personal commitment to getting sober is non-negotiable. Outpatient care relies on you showing up, doing the work, and applying what you learn.
- You Need to Maintain Responsibilities: For professionals who can't just step away from a career, students juggling classes, or parents with kids to care for, outpatient treatment is often the only realistic choice.
For example, a single parent who has to be home for their kids in the evening or a professional who needs to keep working to pay the bills can absolutely thrive in an Intensive Outpatient Program (IOP) that offers flexible evening sessions.
When Inpatient Treatment Is a Better Starting Point
It's just as important to recognize when a more immersive, structured environment is needed. Outpatient treatment might not be the best first step if you're up against severe challenges that demand round-the-clock support and supervision.
You should seriously consider inpatient treatment first if you're dealing with:
- Severe Addiction or Medical Needs: If you need medical detox to safely manage withdrawal symptoms, an inpatient setting is critical. The 24/7 medical oversight keeps you safe during that incredibly vulnerable phase.
- An Unstable or Triggering Home Environment: Trying to recover while living in a place that enables or encourages substance use is like trying to swim upstream in a waterfall. Inpatient care gets you out of those triggers and into a safe space where you can focus completely on healing.
- Co-Occurring Disorders Requiring Stabilization: If you have a serious co-occurring mental health condition like major depression or bipolar disorder that needs intensive stabilization, a residential program provides the integrated, constant care required to tackle both issues at the same time.
Ultimately, the goal is to set yourself up for success. Being brutally honest about your current situation, your support system, and the severity of your addiction is the first and most important step toward finding the right level of care and building a foundation for a life of freedom.
How to Choose the Right Outpatient Program
Finding the right outpatient drug treatment program can feel like searching for a needle in a haystack. But when you know what to ask, the best options quickly stand out. Not all programs are created equal, and your recovery depends on finding one that truly fits your life and your specific needs. This is your guide to making a confident, informed decision.
Think of it like hiring a specialized guide for a difficult expedition. You wouldn't just pick anyone. You'd look for someone with the right credentials, proven tools, and a map that has led others to success. The same logic applies here. The goal is to move past the glossy brochures and find a program that delivers real, evidence-based care designed for you.
Start with the Essentials: Accreditation and Staff Credentials
Before diving into therapy types or schedules, start with the fundamentals. Accreditation from organizations like The Joint Commission or CARF International is a non-negotiable mark of quality. It confirms the facility meets high standards for safety, care, and professionalism.
Just as important are the people who will be guiding your recovery day-to-day. Don't be shy about asking about the credentials of the clinical team. You should be looking for:
- Licensed Clinicians: Therapists should be licensed professionals, such as LPCs (Licensed Professional Counselors) or LCSWs (Licensed Clinical Social Workers).
- Medical Oversight: A qualified psychiatrist or medical doctor should be on staff, especially if you need medication management or dual-diagnosis care.
- Specialized Training: Ask if therapists hold certifications in specific methods like EMDR or DBT. This signals a deeper level of expertise.
A program’s commitment to hiring highly qualified professionals says a lot about the quality of care you’ll receive.
Dig Into the Treatment Approach
Once you've confirmed a program is credible, it's time to look at how they actually help people get better. A one-size-fits-all approach is a massive red flag. A quality outpatient drug treatment program will always create a personalized plan based on a thorough initial assessment.
Your treatment plan should feel like a custom-fit suit, not a rental. It should address not just the substance use, but also any co-occurring mental health conditions, past trauma, or specific life challenges you face.
Ask direct questions about their therapeutic philosophy. Do they use proven, evidence-based therapies like CBT, DBT, and EMDR? Do they offer family therapy to help rebuild your support system? A program that can clearly explain its methods and how they tailor them to individual clients is one you can trust.
Address the Practical Realities: Insurance and Flexibility
Finally, you need to make sure the program fits into your life. Navigating insurance can be a headache, so a good admissions team will help verify your benefits and clearly explain any out-of-pocket costs. Never commit to a program without a transparent breakdown of all potential expenses.
Flexibility is another key factor for success in an outpatient setting. Your recovery shouldn't force you to sacrifice your job or family commitments. Be sure to ask about:
- Scheduling Options: Do they offer evening or morning sessions to fit around a work schedule?
- Telehealth Services: Is there a virtual or hybrid option for days when you can't make it to the facility in person?
A high-quality program that respects your daily responsibilities is essential for building a sustainable, long-term recovery. Asking these key questions is the first step toward finding a true partner in your healing journey.
To make this process easier, we've put together a checklist of essential questions to ask any potential treatment center. Use this table to compare programs and ensure you're making the most informed choice for your recovery.
Key Questions to Ask a Potential Treatment Center
| Category | Question to Ask |
|---|---|
| Accreditation & Licensing | Are you accredited by The Joint Commission or CARF? Are your clinicians licensed in Texas? |
| Assessment & Planning | What does your initial assessment process involve? How do you create an individualized treatment plan? |
| Therapeutic Approach | Which evidence-based therapies (CBT, DBT, EMDR) do you use? Do you offer specialized trauma therapy? |
| Staff Qualifications | What are the credentials of your therapists and medical staff? Is there a psychiatrist on staff for medication management? |
| Dual Diagnosis Care | How do you treat co-occurring mental health conditions like anxiety or depression alongside substance use? |
| Family Involvement | Do you offer family therapy or educational programs for loved ones? How are they included in the process? |
| Program Structure | What is the daily/weekly schedule for the PHP and IOP programs? What is the typical client-to-therapist ratio in groups? |
| Practical Matters | Can you verify my insurance and explain my out-of-pocket costs upfront? Do you offer telehealth or flexible scheduling options? |
| Aftercare & Relapse Prevention | What kind of aftercare planning and alumni support do you provide after treatment completion? |
By using this list, you can cut through the noise and focus on what truly matters: finding a program with the expertise, structure, and flexibility you need to build a lasting recovery.
Building a Foundation for Lifelong Sobriety

Successfully finishing an outpatient drug program is a massive achievement, but it isn't the finish line. Think of it as graduating from training camp. Now, it's time to step onto the field and put everything you've learned into practice in the real world.
Long-term sobriety is all about building on this new foundation with continued support, honest self-awareness, and a solid game plan. Recovery isn't just about saying "no" to substances; it's about building a life so fulfilling that the old urge to escape simply fades away. This is where you transition from the structured environment of treatment to confidently managing your own recovery, armed with the tools you need to thrive.
Creating a Solid Relapse Prevention Plan
One of the most valuable tools you'll leave treatment with is your relapse prevention plan. This isn't some vague idea you keep in your head. It's a concrete, personalized strategy for navigating the inevitable challenges that life will throw your way—your personal roadmap for staying sober when things get tough.
A strong plan boils down to two key steps:
- Identifying Personal Triggers: These are the specific people, places, emotions, or situations that spark cravings or tempt you to use. Getting brutally honest with yourself here is non-negotiable.
- Developing Healthy Coping Strategies: For every single trigger, you need an immediate, healthy action plan. This could be calling your sponsor, hitting the gym, using a mindfulness app, or simply removing yourself from a stressful situation.
Having these responses ready before a trigger hits is like keeping a fire extinguisher in your kitchen. You hope you never need it, but if a fire starts, you're prepared to put it out immediately, stopping a small flare-up from turning into a full-blown disaster.
The Power of Ongoing Support and Aftercare
You don't have to walk the path of recovery alone. In fact, trying to do so is one of the biggest mistakes you can make. Connection is one of the most powerful shields against relapse, which is why stepping into ongoing support after graduating from a PHP or IOP is absolutely essential for keeping your momentum going.
Lifelong recovery is a team sport. Aftercare programs and community support groups provide the accountability, encouragement, and shared experience necessary to navigate the ups and downs of sobriety long after formal treatment ends.
This support system can take many forms, and finding the right mix for you is key to long-term success.
- Aftercare Programs: Many treatment centers offer step-down options, like a Supportive Outpatient Program (SOP), or alumni groups that provide a continued, structured connection to your clinical team and peers who get it.
- Community Support Groups: Organizations like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) offer free, accessible peer support nearly everywhere, providing a structured program for long-term recovery.
- Building a Sober Network: This is huge. It means actively cultivating friendships with other people in recovery who understand your lifestyle and can provide a social circle that genuinely supports your sobriety.
Embracing a New Way of Life
Ultimately, outpatient drug treatment equips you with the skills not just to survive without substances, but to build a vibrant, meaningful life. This involves more than just therapy sessions. It includes practical life skills training—learning how to manage finances, build a career, and foster healthy, honest relationships.
True freedom from addiction comes from building resilience. It’s knowing how to handle stress without reaching for a substance, how to celebrate successes in healthy ways, and how to connect with others authentically. By actively using your relapse prevention plan and leaning hard on your support network, you transform the lessons of treatment into a powerful foundation for a lifetime of sobriety.
Common Questions About Outpatient Treatment
Jumping into outpatient drug treatment naturally brings up a lot of questions. That’s a good thing. It’s smart to get a clear picture before you commit to a path that’s going to reshape your future. We’ve pulled together answers to the questions we hear most often from people considering this flexible, effective form of care.
Can I Keep My Job While in an Outpatient Program?
Absolutely. For many people, this is the single biggest reason they choose outpatient care. These programs are built to fit into your existing life, not completely upend it.
An Intensive Outpatient Program (IOP), for instance, almost always has evening sessions. This flexibility means you can keep your career on track, stay in school, or handle family duties while still getting the comprehensive support you need to heal.
How Long Does Outpatient Drug Treatment Last?
There’s no magic number here—the timeline is tailored to your clinical needs and how you’re progressing. Think of it less like a fixed class schedule and more like a personalized training plan.
However, there are some general timeframes:
- A Partial Hospitalization Program (PHP) is more intense, so it might last for several weeks.
- An Intensive Outpatient Program (IOP) typically runs from several weeks to a few months.
Often, you’ll step down through these levels of care. Your clinical team will work with you to adjust the timeline, making sure it always supports your recovery goals.
What if I Also Have Anxiety or Depression?
You’re not alone—this is incredibly common. Substance use and mental health conditions are often deeply intertwined, which is why finding a program that specializes in dual-diagnosis care is critical.
A reputable outpatient center is fully equipped to treat these co-occurring disorders at the same time. Using an integrated plan, therapies like CBT and DBT are used to tackle both the addiction and the underlying mental health challenge, paving the way for a much stronger, more sustainable recovery.
Is Telehealth as Effective as In-Person Treatment?
For many people, the answer is a resounding yes. When it’s delivered through a structured, high-quality program, virtual therapy can be just as effective as showing up in person.
Telehealth is a game-changer because it knocks down common barriers like transportation issues, childcare needs, or rigid work schedules. This makes getting help far more realistic. Research consistently shows that virtual services achieve similar positive outcomes and patient satisfaction rates as traditional face-to-face treatment, ensuring you get the support you need, wherever you are.
At Altura Recovery, we provide a clear path forward with flexible scheduling and evidence-based care tailored to your life. If you're ready to start your journey toward healing, explore our outpatient programs at https://www.alturarecovery.com.