When you hear the term “intensive outpatient program,” or IOP, it might sound clinical or intimidating. But the idea behind it is actually quite straightforward. An IOP offers structured, evidence-based therapy for several hours a day on multiple days of the week, all without requiring you to stay overnight.
Think of it as the perfect middle ground. It’s more support than a standard weekly therapy appointment but less restrictive than full-time residential or hospital care. This structure allows you to get the robust help you need while still living at home and staying connected to your daily life.
Understanding the Bridge to Real-Life Recovery

Let’s use an analogy. Imagine you’re trying to learn a complex new skill, like playing the guitar. A single one-hour lesson each week is a good start, but putting that knowledge into practice on your own can feel slow and frustrating. An IOP is like joining an immersive workshop that meets several times a week for a few hours at a time. It gives you the focused instruction and guided practice you need to build real skills—and confidence—much more quickly.
The core principle of an IOP is to provide a high level of clinical care while letting you maintain your commitments to work, school, or family. You get powerful mental health treatment during the day or evening, then you go home. This design is crucial because it allows you to immediately apply the coping strategies and communication skills you’re learning in therapy to your actual life, right as challenges pop up.
Key Features of an Intensive Outpatient Program
This approach isn’t just about convenience; it’s a strategic model built for sustainable, real-world recovery. And the evidence backs it up. IOPs have proven remarkably effective at reducing crisis situations. For example, a 2023 study found that 94% of young adult clients with a history of recent mental health-related ER visits had zero such visits after completing an IOP. You can discover more about these IOP outcomes and their impact on crisis care.
So, what are the defining traits of this level of care? Here’s a quick look at the core components.
Key Features of an Intensive Outpatient Program
| Feature | Description |
|---|---|
| Time Commitment | Typically involves 9-20 hours of treatment per week, spread across 3 to 5 days. |
| Living Situation | You live at home or in a supportive environment, not at the treatment facility. |
| Clinical Structure | Consists of evidence-based therapies, including group sessions, individual counseling, and skill-building workshops. |
| Flexibility | Programs often offer day, evening, and virtual options to fit around existing life responsibilities. |
| Primary Goal | To build coping skills, manage symptoms, and establish a stable foundation for long-term recovery. |
At the end of the day, an intensive outpatient program for mental health serves as a vital bridge. It connects the safety and structure of a therapeutic environment with the everyday realities of your life, creating a powerful and practical pathway to lasting wellness.
Core Therapies Used in Effective IOP Treatment
An effective intensive outpatient program isn’t just a place you go; it’s a workshop where you engage with powerful, evidence-based therapies that drive real change. These are the engines of recovery, designed to do more than just manage symptoms. They give you a practical toolkit for rebuilding your life from the ground up.
Think of these therapies as different tools for a complex project. You wouldn't use a hammer to turn a screw, right? In the same way, an IOP uses specific therapeutic models to address distinct challenges, from automatic negative thoughts to overwhelming emotions.
Cognitive Behavioral Therapy: Rewiring Your Thoughts
Cognitive Behavioral Therapy, or CBT, is a foundational approach in nearly every high-quality IOP. It works on a simple but powerful idea: our thoughts, feelings, and behaviors are all connected. Change one, and you can change them all.
Imagine your mind is like a garden where weeds—those unhelpful, automatic negative thoughts—have started to take over. CBT is like a practical gardening class. It teaches you how to spot the weeds, understand why they’re growing, and intentionally replace them with healthier ways of thinking.
Many programs also use specific forms of this therapy, like Cognitive Behavioral Therapy for insomnia, to tackle related issues like sleep disturbances that often go hand-in-hand with mental health struggles. This shows how CBT provides concrete skills for real-world problems.
A core goal of CBT is to shift you from being a passive recipient of your thoughts to an active participant in your mental well-being. It empowers you to challenge and reframe the internal narratives that hold you back.
This is why CBT is so effective for conditions like depression, anxiety, and substance use disorders. It provides a structured, goal-oriented path to changing your behavior for the better.
Dialectical Behavior Therapy: Building Emotional Resilience
Dialectical Behavior Therapy, or DBT, is another cornerstone of modern IOP treatment. While CBT hones in on thoughts, DBT gives you the skills to manage intense emotions and navigate difficult relationships, especially when feelings become overwhelming.
Think of DBT as learning to captain a ship in a stormy sea. It doesn't promise to stop the waves (difficult emotions), but it teaches you how to become a skilled sailor. You learn to ride those waves without capsizing by mastering four key skill sets:
- Mindfulness: Staying present and observing your thoughts and feelings without judgment.
- Distress Tolerance: Getting through crisis situations without making them worse.
- Emotion Regulation: Understanding and managing your emotional responses in a healthier way.
- Interpersonal Effectiveness: Communicating your needs, setting boundaries, and building positive relationships.
DBT is especially helpful for individuals struggling with conditions like borderline personality disorder, self-harm, and co-occurring disorders. It acknowledges the intensity of their emotional experience and offers practical ways to build a life they feel is worth living. Group sessions are a huge part of this, offering a safe space to practice these new interpersonal skills. In fact, building these skills is often a key part of many relapse prevention activities for groups.
EMDR: Processing and Healing from Trauma
For those whose mental health challenges are rooted in trauma, Eye Movement Desensitization and Reprocessing (EMDR) is a specialized and powerful therapy. It helps the brain correctly process and store traumatic memories so they no longer trigger a fight-or-flight response in daily life.
Imagine a traumatic memory is like a corrupted file on your computer. Every time you try to open it, the whole system crashes. EMDR works like a defragmentation tool, helping your brain re-file the memory so you can access it without causing system-wide distress.
During an EMDR session, a therapist guides you in recalling a traumatic event while engaging in bilateral stimulation, like side-to-side eye movements. This process helps dial down the memory's vividness and emotional charge. The goal isn't to forget what happened, but to finally remove its painful grip on your present.
These core therapies—CBT, DBT, and EMDR—form the clinical backbone of a quality intensive outpatient program. They aren't just abstract concepts; they are active, skill-building practices that put you back in the driver's seat of your own recovery.
Who Is an Intensive Outpatient Program For?
Deciding if an intensive outpatient program for mental health is the right next step is about more than a diagnosis. It’s about matching the level of care to your real-life circumstances, your current struggles, and where you want to go. An IOP isn’t for everyone, but for the right person, it’s often the exact catalyst needed to create meaningful, lasting change.
Here’s one way to think about it: If weekly therapy is like meeting a personal trainer once a week, and inpatient care is a full-immersion fitness bootcamp, an IOP is like a dedicated training camp. You get focused, expert guidance several days a week while still going home to test your new strengths in the real world.
The Ideal Candidate Profile
An IOP is most effective for people who are medically stable but need more support and structure than traditional outpatient therapy can provide. They aren't in immediate crisis, but they're struggling enough that their daily functioning—at work, school, or home—is taking a significant hit.
This level of care is a game-changer for two main groups:
- Those Stepping Down from a Higher Level of Care: Someone finishing an inpatient or residential stay often needs a bridge back to everyday life. An IOP provides the clinical structure to make new coping skills stick and prevent relapse while getting back into the rhythm of personal and professional responsibilities.
- Those Needing More Than Weekly Therapy: For individuals whose symptoms are getting worse or just not improving with once-a-week sessions, an IOP offers a much-needed boost in intensity. It provides the momentum required to break through plateaus and start making tangible progress.
The core requirement for success in an IOP is a basic level of stability. Having a safe and reasonably supportive home environment is crucial because you'll be actively applying therapeutic skills to real-life triggers and stressors between your sessions.
How an IOP Fits into Real Life
The flexible nature of an IOP makes it a practical choice for people from all walks of life. A working professional struggling with anxiety and burnout can attend evening sessions without having to step away from their career. A college student facing depression can schedule treatment around their classes, letting them stay on track with their education while building essential mental health skills.
For those dealing with substance use alongside their mental health, an IOP offers a structured environment to practice skills for curbing cravings and managing triggers in their day-to-day environment.
The demand for this kind of flexible yet structured care is undeniable. In 2023, over 20% of U.S. adults experienced a mental illness, yet more than half received no treatment at all. As the need for care grows, IOPs are proving to be a highly effective solution. Recent data from the Cleveland Clinic, for instance, showed that among outpatient clients with moderate depression, 42.8% improved and 50% remained stable over several months of treatment. Learn more about these Cleveland Clinic mood disorder treatment outcomes.
Ultimately, the best candidate for an IOP is someone who is motivated and ready to actively participate in their own recovery—someone equipped to turn the lessons learned in therapy into life-changing habits.
Comparing Levels of Mental Health Treatment
To really grasp why an intensive outpatient program for mental health is such a game-changer, it helps to see the whole landscape of care. Mental health treatment isn’t a one-size-fits-all deal; it’s a spectrum designed to meet you exactly where you are.
Think of it like physical therapy after an injury. Some people need to be in the hospital with 24/7 monitoring right after surgery. Others just need a weekly check-in with a therapist to stay on track. An IOP sits right in that vital middle ground.
It offers a significant leg up from traditional weekly therapy but doesn't require you to put your entire life on hold for residential care. This creates a much more gradual, sustainable path to getting better, especially for anyone moving from a higher level of support back into their daily life.
This flow chart shows the typical "step-down" journey, moving from the most intensive care to the most independent.
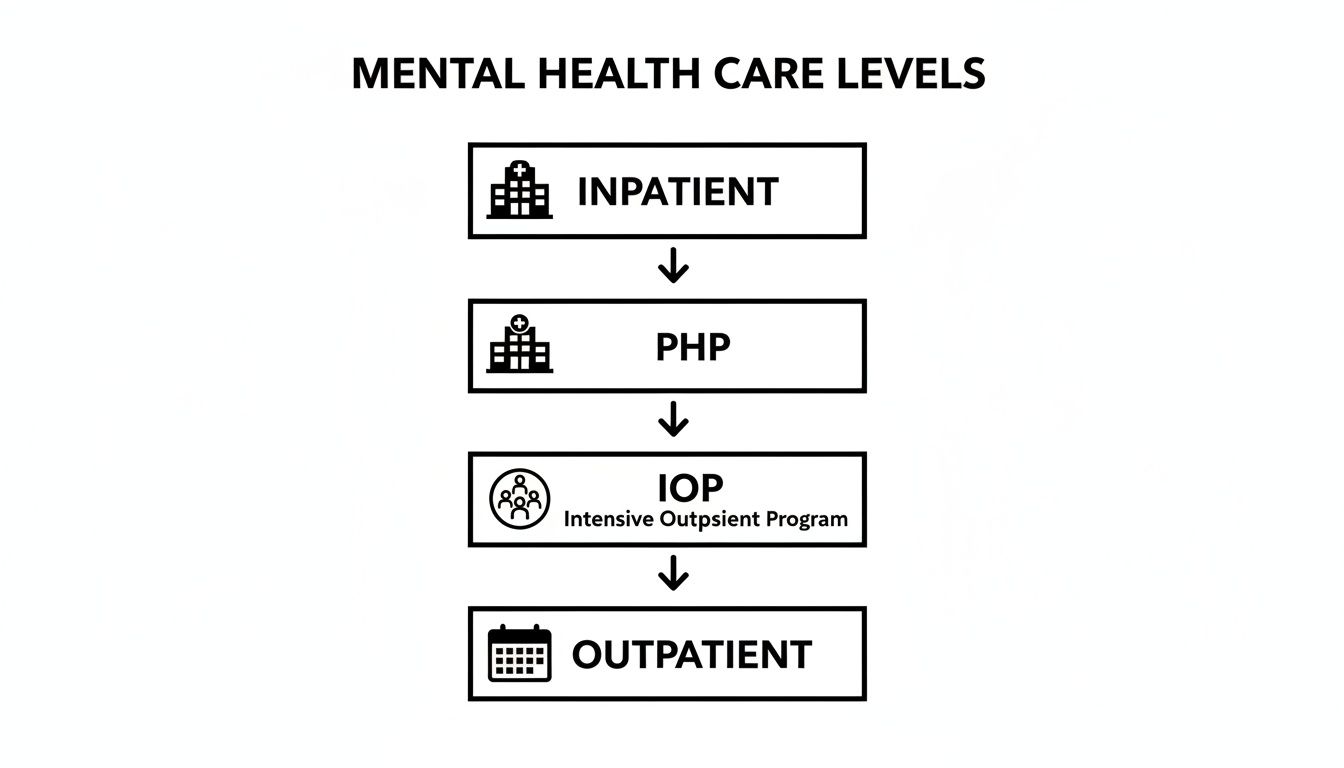
As you can see, each level has a distinct job. Together, they form a clear pathway that allows you to build stability and independence one step at a time. Let's dig into what makes each one different.
The Step-Down Model In Action
The "step-down" process is a cornerstone of modern recovery. It’s the intentional journey from a highly structured, supervised environment back to independent living, but with guardrails.
Someone might start at an inpatient facility to get through a crisis. From there, they could move to a Partial Hospitalization Program (PHP) for all-day, structured treatment. An IOP is the next logical step down, scaling back the time commitment while keeping the clinical support strong.
This gradual transition is everything. It prevents the jarring shock of going from 24/7 support straight back to the triggers and stresses of daily life, which can easily derail progress. Each step down reinforces the skills you've learned and builds the confidence you need to use them.
The goal of the step-down model is not just to treat symptoms, but to build a foundation for lasting wellness. It’s about practicing recovery in real-world settings with a safety net that slowly becomes less needed over time.
For many people, this journey also includes supportive housing. For those who need a stable, sober environment while in outpatient care, resources like a sober living house can be an essential component of a solid recovery plan.
IOP vs Other Levels of Care: A Side-by-Side Comparison
To make the differences crystal clear, let's look at how these programs stack up in terms of time, structure, and focus. This table gives you a quick snapshot of where an IOP fits into the bigger picture.
| Level of Care | Time Commitment (Weekly) | Living Situation | Primary Focus |
|---|---|---|---|
| Inpatient Hospitalization | 24/7 supervision | Live at the hospital or facility | Crisis stabilization, medical safety, and intensive psychiatric care. |
| Partial Hospitalization (PHP) | 20-30+ hours (5 days/week) | Live at home or in supportive housing | Intensive, structured daily therapy to build foundational coping skills and prevent re-hospitalization. |
| Intensive Outpatient (IOP) | 9-20 hours (3-5 days/week) | Live at home | Applying coping skills to real life, managing symptoms, and integrating recovery into work/school routines. |
| Standard Outpatient | 1-3 hours (1-2 days/week) | Live at home | Ongoing maintenance, relapse prevention, and processing specific life challenges. |
Ultimately, choosing the right level of care comes down to your current needs, your stability, and the support system you have around you. The beauty of this tiered system is its flexibility—it allows your treatment plan to evolve right alongside your progress.
What to Expect During Your IOP Journey
Starting an intensive outpatient program for mental health can feel like stepping into the unknown. But the journey is structured, supportive, and designed with your real life in mind. It all begins with a foundational first step to ensure your care is perfectly aligned with your needs. This isn’t about fitting you into a pre-made box; it’s about building a program around you.
The whole experience kicks off with a comprehensive initial assessment. Think of it as creating a detailed map before a road trip. In a confidential and compassionate conversation, our clinical team gets to know you—your history, current struggles, strengths, and recovery goals. That assessment becomes the basis for your personalized treatment plan, which outlines the specific therapies, goals, and schedule that will guide your time with us.
A Look Inside a Typical Session
Once your plan is in place, you’ll start attending sessions. These are typically held for about three hours a day, three to five days a week. We intentionally design the schedule to be a dynamic and engaging mix of different therapeutic activities. While every program has its unique flow, a typical day often includes a combination of core components.
A session might start with a group check-in, where members share recent wins and challenges. That could be followed by a skill-building group focused on a specific topic, like mindfulness, emotion regulation from DBT, or challenging negative thought patterns from CBT. This blend of sharing and learning creates a powerful environment for growth.
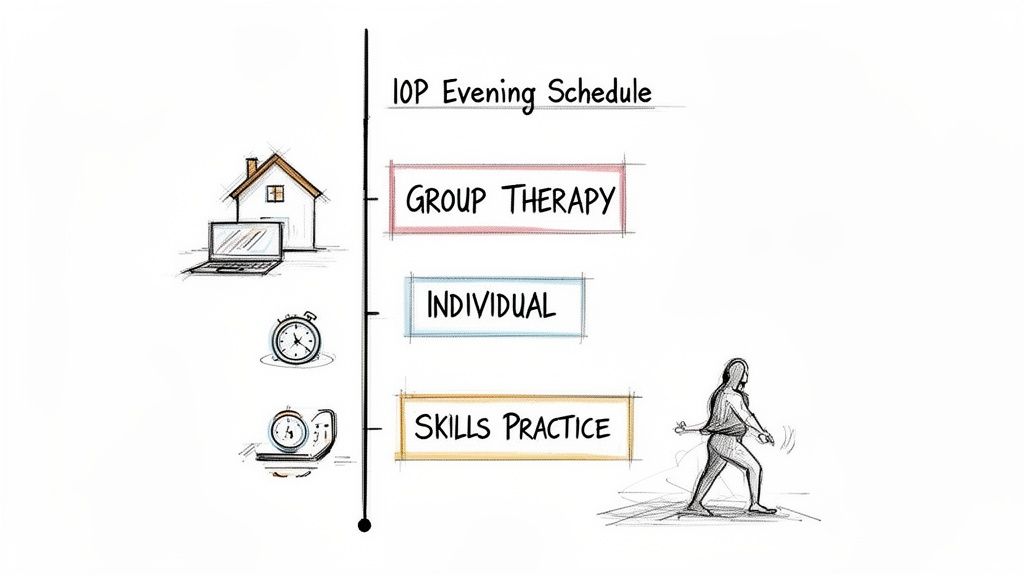
- Individual Counseling: These one-on-one sessions with your primary therapist are your time to dive deeper into personal issues, process trauma, and track progress toward your goals.
- Group Therapy: This is really the heart of the IOP experience. Led by a licensed clinician, these sessions provide a safe space to practice communication skills, gain new perspectives, and realize you are not alone in your struggles.
- Family Workshops: Many programs, including ours, offer sessions that include loved ones. These workshops help repair relationships, improve communication, and build a strong support system at home—which is vital for long-term success.
Flexibility That Fits Your Life
One of the greatest strengths of an intensive outpatient program is its inherent flexibility. The goal is to integrate treatment into your life, not force you to put your life on hold. That’s why most high-quality programs offer multiple scheduling options.
The core idea behind IOP is that recovery happens in the real world. By allowing you to stay connected to your work, school, and family, the program turns everyday challenges into immediate opportunities to practice and reinforce new coping skills.
This flexibility extends to how care is delivered. In addition to traditional in-person sessions, many providers now offer virtual IOP options. These online programs provide the same level of evidence-based care through secure video platforms, removing geographical barriers and making treatment accessible to more people.
Virtual IOPs are proving to be highly effective. A 2023 analysis of one virtual program found that 90% of clients experienced a significant reduction in distress, with depression symptoms dropping by an average of 45%. You can learn more about these virtual IOP findings and see how they are expanding access to quality care. This model is perfect for busy professionals, students, or anyone who needs effective mental health support that fits a demanding schedule.
Your journey through an IOP is an active, collaborative process designed to empower you with the tools and confidence for lasting wellness.
How to Find and Pay for the Right Program
Finding the right intensive outpatient program for mental health comes down to two things: figuring out the money and vetting the quality of the care. It can feel like a lot to tackle at once, but breaking it down into a clear plan makes the whole process manageable, helping you find a provider that’s a genuine fit.
The best place to start is with your financial options. Most quality IOPs accept commercial health insurance, and recent policy changes have opened up access significantly. As of January 1, 2024, Medicare officially began covering IOP services for both mental health and substance use disorders—a huge step forward for countless people who need this level of care.
Navigating Insurance and Payment
Before you even start calling different programs, make a quick call to your insurance provider. Just flip over your insurance card, dial the member services number, and ask them to walk you through your specific benefits for outpatient mental health services. Trust me, this one phone call can save you a mountain of confusion down the road.
When you're sorting out how to pay for an IOP, a little homework goes a long way. Getting familiar with the basics of medical billing for mental health empowers you to ask smart questions about copays, deductibles, and out-of-pocket maximums.
Most programs also have admissions coordinators who will do the legwork for you by running a verification of benefits. They’ll contact your insurance company on your behalf to pin down your exact coverage, giving you a clear picture of any costs. It's an invaluable service that takes a lot of the guesswork out of the process.
Don't let financial questions stop you from seeking help. A good program will be transparent about costs and work with you to understand your benefits and payment options before you ever commit to starting treatment.
Critical Questions to Ask Any IOP Provider
Once you have a handle on the financial side, it’s time to shift your focus to the quality of the treatment itself. Not all IOPs are created equal. You need to become an investigative reporter for your own well-being. Asking sharp, specific questions helps you see past the marketing brochures and understand the real substance of a program.
Think of this as a checklist. The answers you get will tell you volumes about a provider’s clinical expertise, their philosophy of care, and how committed they are to your long-term success.
- What are the credentials of your clinical staff? You want to hear about licensed professionals like LPCs (Licensed Professional Counselors), LCSWs (Licensed Clinical Social Workers), and psychiatrists or psychiatric nurse practitioners for medication management.
- What specific evidence-based therapies do you use? A quality program won’t hesitate to name their core methods, like CBT, DBT, or EMDR, and should be able to explain how they put them into practice.
- How is the treatment plan personalized? Ask them how they’ll tailor the program to your specific diagnosis, history, and goals. The answer shouldn’t be generic.
- What does family involvement look like? Find out if they offer family therapy or educational workshops. Healing is a team sport, and a strong support system is key.
- What is your approach to aftercare planning? A great program doesn’t wait until the last day to talk about what comes next. They should start planning your transition to a lower level of care, like a supportive outpatient program, from day one.
- How do you support clients with co-occurring disorders? This one is vital. If you’re dealing with both mental health and substance use issues, the program must be equipped to treat both. Overlooking one can put your entire recovery at risk. For a closer look at this, you can learn more about the complexities of withdrawal symptoms and co-occurring conditions in our guide.
Common Questions About IOP for Mental Health
Thinking about an intensive outpatient program always brings up a lot of practical questions. Getting clear, straightforward answers is the key to feeling confident about taking the next step.
Let's walk through some of the most common uncertainties to help you understand exactly what to expect and demystify the process.
How Long Does a Typical Intensive Outpatient Program Last?
While there's no universal timeline, most IOPs run for about 8 to 12 weeks. The exact duration, however, is always tailored to you.
A high-quality program will continuously assess your progress and adjust the length of your stay based on your unique needs and therapeutic milestones. This makes sure you get the right amount of support without dragging out treatment unnecessarily. The goal is always to prepare you for a smooth transition to a lower level of care, like a standard outpatient program, making your recovery durable.
Can I Still Work or Go to School While in an IOP?
Yes, absolutely. This is one of the biggest advantages of the IOP model and a primary reason people choose this level of care.
Programs are specifically designed to fit into your existing life. With flexible schedules that often include day, evening, and even virtual sessions, you can get the structured treatment you need without having to pause your career, education, or family commitments. It's all about integrating recovery directly into your daily routine.
An IOP is built on the principle that real healing happens in your real-world environment. It gives you the chance to apply new skills and coping mechanisms immediately, turning everyday challenges into opportunities for growth and resilience.
What Is the Difference Between IOP Group Therapy and a Support Group?
The main difference comes down to the clinical structure and leadership. IOP group therapy is a formal type of treatment led by a licensed therapist or clinician.
These sessions use evidence-based methods, like CBT or DBT, to teach specific skills, process emotions, and work toward defined treatment goals. Think of it as an active, guided therapeutic process.
In contrast, support groups (like those run by NAMI or DBSA) are typically peer-led. They provide invaluable mutual encouragement and shared experience but aren't a substitute for clinical treatment. Both play important roles, but an IOP group is a core component of your professional mental health care plan.
Will My Family Be Involved in My IOP Treatment?
Family involvement is often a vital part of a successful recovery and is highly encouraged in many programs. When your loved ones are part of the process, the entire support system gets stronger.
Many IOPs offer dedicated family therapy sessions, educational workshops, and other resources. This approach helps heal relationship dynamics, improve communication, and give your family the tools to support you effectively. Building an informed and supportive home environment creates a much stronger foundation for lasting wellness for everyone.
At Altura Recovery, we understand that these questions are just the beginning. Our dedicated team is here to provide clear answers and guide you through every step of the process. We believe in a personalized, step-down model that empowers you with the skills for real healing and sustainable growth, all while fitting into your life. To learn more about our flexible and evidence-based intensive outpatient programs, visit us at https://www.alturarecovery.com.







