When you're trying to break free from opioid withdrawal, the most pressing question is always the same: How long will this relief last? For most people on a stable dose of Suboxone, the answer is a reassuring 24 to 36 hours. This makes a simple, once-a-day dose powerful enough to manage both physical withdrawal and mental cravings, giving you a steady foundation to build your recovery on.
How Suboxone Creates a Shield Against Withdrawal
Think of Suboxone less like a temporary fix and more like a time-release shield. Its entire purpose is to protect you from the intense physical and psychological distress of opioid withdrawal. By doing so, it gives your brain and body the stability they desperately need to begin healing. This powerful effect comes from two key ingredients working in tandem.
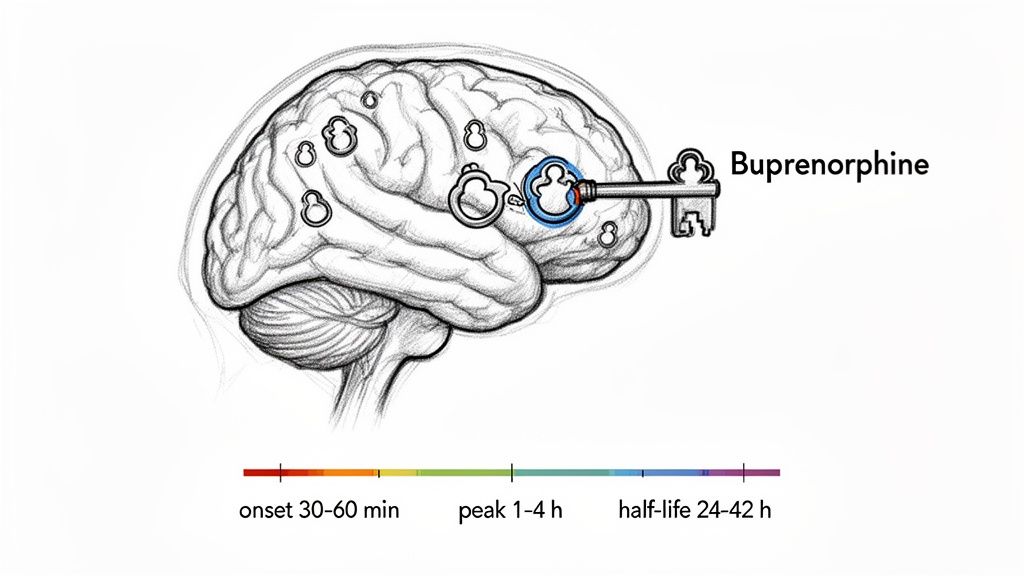
First up is buprenorphine, a long-acting partial opioid agonist. It works by gently fitting into the brain's opioid receptors—the same ones that full opioids like heroin or fentanyl target. This action is just enough to quiet withdrawal symptoms and dial down cravings, but it doesn't produce the euphoric high that drives addiction. Buprenorphine binds very tightly to these receptors, which is the secret to its long-lasting effect.
The second ingredient is naloxone, an opioid antagonist. You can think of naloxone as a built-in safety feature designed to discourage misuse. If someone were to dissolve the film or tablet and inject it, the naloxone would immediately activate, block the opioid receptors, and trigger severe withdrawal symptoms. But when you take Suboxone as prescribed (dissolved under the tongue), very little naloxone gets absorbed, allowing the buprenorphine to do its job perfectly.
Suboxone doesn't just put a temporary pause on withdrawal; it delivers a full day of stability. This 24-hour coverage is a game-changer because it breaks the exhausting cycle of constantly seeking opioids, freeing you up to focus on rebuilding your life.
The visual timeline below breaks down what happens in your body after a single dose, from the moment it starts working to how long the effects last.
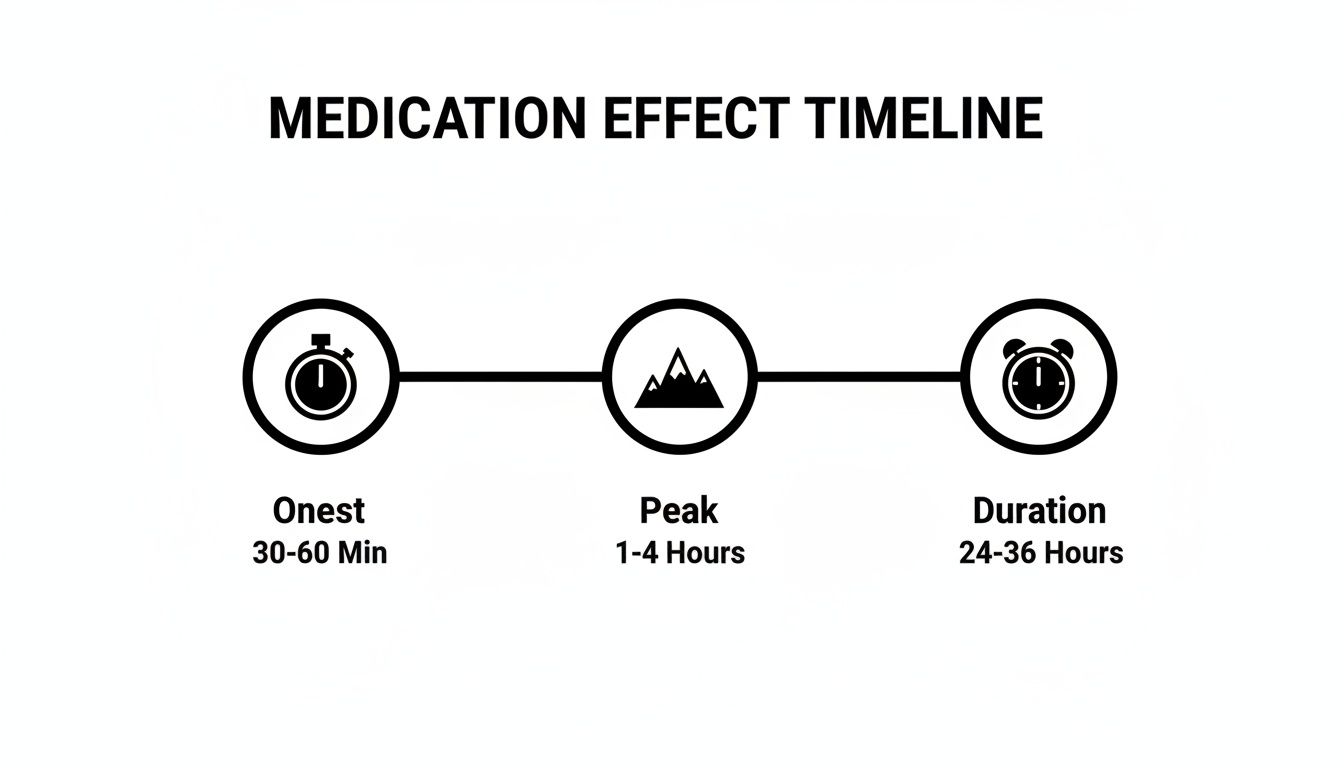
As you can see, the medication gets to work quickly, its effects become strongest within a few hours, and then it holds steady for a full day or even longer. This long duration is precisely what makes Suboxone such a cornerstone of effective medication-assisted treatment.
The Science Behind Suboxone's Lasting Effects

To really get why Suboxone is so effective for so long, you have to understand how its main ingredient, buprenorphine, works in the brain. Think of your brain’s opioid receptors as locks on a door. Buprenorphine is like a very special key.
Unlike full opioids (like heroin or oxycodone) that turn the lock and swing the door wide open, buprenorphine is a partial agonist. It fits the lock perfectly but only opens the door partway. That partial activation is just enough to quiet withdrawal and shut down cravings, but it's not enough to produce a euphoric high.
But here’s the most important part: buprenorphine has an incredibly high affinity for those receptors. Once its key is in the lock, it latches on and doesn't let go easily. This means other opioids can’t just come along and push it out of the way. This super-strong bond is the secret to Suboxone’s long-lasting power.
Breaking Down Suboxone's Lifespan
When we talk about how long a medication works, we’re really looking at a few key milestones. Knowing these terms makes it clear why Suboxone provides such steady, sustained relief.
- Onset of Action: This is how fast you feel it working. With the sublingual film or tablet, you’ll typically start to feel relief within 30 to 60 minutes.
- Peak Effects: This is when the medication is working its hardest. Withdrawal symptoms and cravings are most suppressed between 1 and 4 hours after your dose.
- Half-Life: This is the time it takes for your body to clear out half of the drug. Buprenorphine has a remarkably long half-life, ranging from 24 to 42 hours.
This long half-life is the reason a single daily dose is usually enough to keep you stable. The medication leaves your system very slowly, preventing the rollercoaster of highs and lows that comes with short-acting opioids and giving your brain a chance to find balance.
By stabilizing brain chemistry for over 24 hours, Suboxone provides more than just symptom relief. It creates a crucial window of clarity, allowing you to focus on the psychological and emotional work of recovery.
The Bigger Picture: Lasting Recovery
The daily effect of Suboxone is one thing, but the long-term duration of treatment is what leads to lasting recovery. Daily stability is the foundation, but successful recovery is a marathon, not a sprint. Sticking with treatment for the long haul is proven to save lives.
Research shows that staying on medication-assisted treatment for 15-18 months or longer dramatically reduces risks, leading to 173% fewer overdoses and 128% fewer opioid-related emergency room visits. Short-term tapers often fail because the brain simply needs more time to heal and rewire.
One study of nearly 5,000 patients found that stopping treatment between 91 and 180 days more than doubled the risk of overdose compared to those who continued. If you want to dive deeper, you can explore the full study about treatment duration and patient outcomes.
Individual Factors That Influence Suboxone's Duration
While the typical 24-hour duration of Suboxone is a reliable benchmark, it’s not set in stone. The real answer to "how long does Suboxone work" is unique to each person. Several individual factors can speed up or slow down how your body processes the medication, directly impacting how long you feel its stabilizing effects.
Think of your body's metabolism like a car's engine. Some engines burn fuel quickly, while others are more efficient and burn it slowly. A person with a faster metabolic rate will process and clear buprenorphine from their system more quickly, potentially shortening the medication's effective window. This is why some people might feel withdrawal symptoms creeping back in before the 24-hour mark, while others feel stable for much longer.
Your Health and Medication History
Your overall health profile plays a huge role, especially the condition of your liver. The liver is the body's primary processing plant for medications like Suboxone. If it's not functioning at its best due to conditions like hepatitis or other liver diseases, it can struggle to break down buprenorphine efficiently.
This can cause the medication to last longer in your system than intended, which requires careful dose adjustments from a medical professional to stay safe and effective.
Other key factors also come into play:
- Body Mass and Composition: A person's weight and body fat percentage can influence how Suboxone is distributed and stored in the body, which can alter its duration.
- Severity of Opioid Use: Someone with a long history of high-dose opioid use may need a higher or more frequent dose of Suboxone to feel stable, as their brain chemistry has adapted differently.
- Other Medications: Certain medications can interfere with the liver enzymes responsible for processing buprenorphine. Some might make it last longer, while others could clear it out of your system faster.
Understanding these individual variables is essential for effective treatment. A one-size-fits-all approach just doesn't work in recovery, which is why personalized medication management is so important.
At Altura Recovery, our clinicians conduct thorough evaluations to understand these unique factors for every person we help. This allows us to make precise dose adjustments, ensuring the medication works effectively for your specific needs. By tailoring the treatment plan, we help you maintain the stability needed to focus on your recovery without the distraction of returning cravings or withdrawal symptoms. This careful, individualized approach is key to building a strong foundation for long-term success.
Comparing Suboxone Films and Tablets
When you're prescribed Suboxone, it usually comes in one of two forms: a thin film that dissolves under your tongue or a small tablet that does the same. While both deliver the exact same medication—buprenorphine and naloxone—there are a few subtle differences that can impact your daily routine.
The most important thing to get right, no matter which form you use, is how you take it. Both the film and the tablet are designed to be absorbed directly into your bloodstream through the membranes in your mouth. This means you have to let them dissolve completely under your tongue (sublingually) or inside your cheek (buccally).
If you swallow them, they're not going to work. The medication will head straight to your liver, which deactivates most of it before it ever has a chance to help. This can dramatically shorten its effects and bring withdrawal symptoms roaring back.
Film vs. Tablet: Which Is Right For You?
Honestly, the choice between the film and the tablet often just comes down to personal preference. Some people love the convenience of the film, while others are just more comfortable with a traditional tablet.
Here are a few things to think about when you talk to your doctor:
- How fast does it dissolve? The film is usually quicker, disappearing in about 5 to 10 minutes. The tablet can take a bit longer, closer to 10 to 15 minutes.
- What about taste and texture? Both have a citrus-like flavor, but the feel is different. The film is paper-thin and discreet, while the tablet feels like a tiny pill.
- Is it easy to adjust the dose? This is where films have a clear edge. They can be easily and precisely cut if your doctor is tapering your dose. Splitting a tiny tablet accurately is much trickier.
No matter which one you use, the goal is the same: let it fully dissolve. To get the full, long-lasting benefit, avoid eating, drinking, or smoking for at least 15-30 minutes after it's gone. This gives your body time to absorb everything.
Thinking through the practical side of things can make a real difference in sticking with your treatment. The table below breaks down the key features of each option to help you see how they stack up side-by-side.
Suboxone Film vs. Tablet At a Glance
| Feature | Suboxone Film | Suboxone Tablet |
|---|---|---|
| Administration | Placed under the tongue to dissolve | Placed under the tongue to dissolve |
| Dissolve Time | Faster (approx. 5-10 minutes) | Slower (approx. 10-15 minutes) |
| Dose Flexibility | Easily cut for precise dose adjustments | Can be harder to split accurately |
| Portability | Individually wrapped, flat, and discreet | Packaged in a bottle or blister pack |
At the end of the day, both the film and the tablet are equally effective when you take them correctly. The "best" one is simply the one that fits seamlessly into your life and recovery plan.
If you have questions about your prescription or feel like one form might work better for you than the other, don't hesitate to bring it up. The expert team at Altura Recovery can provide the medication management guidance you need to feel confident and stable on your recovery journey.
Daily Relief vs. Long-Term Recovery
It’s one of the most common points of confusion: How long does a dose of Suboxone last versus how long should I stay in treatment? While a single, daily dose provides roughly 24 hours of relief from cravings and withdrawal, true, lasting recovery is built over a much longer horizon. Getting this distinction right is probably one of the most important parts of succeeding with medication-assisted treatment.
Think of it like taking medication for high blood pressure. You take a pill every day to keep your numbers stable and prevent a crisis. That daily action is critical, but the real goal is to stay on it long-term to prevent a heart attack or stroke down the road. Suboxone works the same way. The daily dose manages the immediate symptoms, but staying in treatment for months—or even years—is what protects you from relapse and gives your brain the time it needs to heal.
Why Treatment Duration Matters More Than Daily Dose
The stability you feel from a daily dose is the foundation, but it's not the whole house. Opioid use disorder creates profound changes in brain chemistry, and it takes a long time for those neural pathways to find their way back to a healthy balance. Ending treatment too soon is like trying to run on a broken leg before it has fully mended—it’s just a recipe for reinjury.
The goal isn't just to get through the day without using opioids; it's to build a life where you no longer need them. That process requires time to forge new coping skills, lean on a strong support system, and dig into the root causes of the addiction in the first place.
Lasting recovery isn't measured in hours or days. It's measured in the sustained commitment to a treatment plan that gives your brain the time it needs to heal. Rushing this process is one of the biggest risks to your long-term success.
This isn't just a hunch; the scientific evidence overwhelmingly backs this long-term approach. Longer treatment durations are directly linked to significantly better outcomes, including much lower rates of relapse and overdose.
The Evidence for Longer Treatment
The data on Suboxone's effectiveness over time is crystal clear. While a quick taper might sound appealing, it often leads straight back to relapse because the brain's opioid receptors haven't had nearly enough time to normalize. In fact, some research shows that more than 90% of individuals relapse after a rapid, three-week taper.
Contrast that with sticking to treatment for an extended period, which yields dramatic improvements in safety and stability. One powerful study showed that patients who remained in treatment for 15-18 months or more saw a 173% reduction in overdoses and a 128% drop in opioid-related emergency room visits compared to those in treatment for shorter stints. You can learn more about the findings on extended treatment and its benefits.
These numbers paint a clear picture: how long Suboxone works for your recovery is a far more important question than how long a dose works in a single day. At Altura Recovery, our outpatient treatment programs are built around providing this essential long-term support, helping you build a sustainable foundation for a future free from addiction.
Building Your Path to Sustainable Recovery
Knowing how long Suboxone works each day is the first piece of the puzzle. But the real goal, the more important step, is building a life where that daily stability leads to lasting freedom from addiction. This is where a structured, supportive treatment plan becomes non-negotiable.
Successful recovery is about so much more than just taking medication. It's about creating an entire ecosystem of support that empowers you to heal from the inside out.
This is exactly why comprehensive outpatient programs are so effective. They provide the clinical care and structure you need, but with the flexibility to keep up with your life—work, school, or family. Recovery starts to integrate into your world instead of disrupting it, letting you build and practice real-world coping skills as you go.
Creating Your Ecosystem of Support
Sustainable recovery isn’t built in isolation. It’s nurtured through a combination of evidence-based care and genuine human connection. Think of it as assembling a dedicated team, with each member playing a vital role in your long-term success.
A strong plan almost always includes:
- Psychiatric Care: It's incredibly common for people with substance use disorder to also face challenges like anxiety or depression. Treating these co-occurring conditions is critical for preventing relapse.
- Evidence-Based Therapy: Modalities like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) are powerful tools. They help you rewire old thought patterns and develop healthier ways to respond to stress and emotions.
- Community Connection: Group therapy and other support networks provide a safe space to share what you're going through. It’s a powerful reminder that you are not alone on this journey.
Lasting freedom isn't just about stopping substance use; it’s about building a life so fulfilling that you no longer feel the need to escape from it. Treatment provides the tools, but you build the future.
This holistic approach transforms treatment from a temporary fix into a foundation for real, sustainable growth. For anyone exploring their options, understanding the different types of support available is key. A great place to start is by learning more about finding the right fit among the various addiction recovery programs near you that offer this kind of integrated care.
Frequently Asked Questions About Suboxone

As you settle into your recovery, it's natural for practical questions to pop up. Feeling confident in your treatment plan is a huge part of staying committed, so let’s clear up a few things you might be wondering about.
Can I Take Suboxone Twice a Day If It Wears Off Early?
This is a common question, especially in the early days of treatment. While most people do well on a once-a-day schedule, it’s not a one-size-fits-all situation. For some, especially those with a faster metabolism, the effects can start to fade before that 24-hour mark, bringing back cravings or mild withdrawal.
In these cases, a provider might recommend splitting the dose. However, this is a medical decision. Never adjust your dose or timing on your own. Your doctor needs to assess your symptoms to find the safest and most effective strategy for you. Proper medication management is what keeps your recovery stable and on track.
What Should I Do If I Miss a Dose of Suboxone?
First, don't panic. Thanks to its long half-life, missing one dose usually won't send you into full-blown withdrawal, especially if you’ve been on a stable dose for a while. You might notice some cravings creeping back in or feel a little off as the medication levels in your system dip, but it's generally manageable.
If you remember later in the day, go ahead and take the missed dose—unless it's already close to your next scheduled one. The most important rule is to never double up your dose to catch up. If you're unsure, the best move is always to call your provider for guidance. They can tell you exactly how to get back on schedule safely.
How Will I Know When It Is Time to Stop Taking Suboxone?
Deciding to taper off Suboxone is a major step in recovery, and it's a decision that you and your treatment team must make together. There's no magic timeline; it’s all about your personal progress and stability.
When you're consistently sober, have a rock-solid support system, and feel confident in your coping skills, that's when the conversation can begin.
Tapering has to be done slowly and under close medical supervision to keep withdrawal symptoms at bay and prevent relapse. Rushing this process is one of the biggest threats to the stability you've worked so hard to build.
Navigating the road to recovery isn’t something you have to do alone. At Altura Recovery, we create personalized outpatient programs that give you the expert guidance and community support needed to build a life free from addiction. Find out more about how we can help at https://www.alturarecovery.com.