When you hear the term co-occurring disorders, it might sound clinical, but the idea is straightforward: it’s the reality of facing two connected challenges at the same time—a mental health condition and a substance use disorder. It's not a personal failure or a sign of weakness. It’s a complex medical situation where each issue can feed the other, which is why it's also commonly called a dual diagnosis.
Understanding the Two-Part Challenge
Imagine trying to put out two fires that are right next to each other. If you only focus on extinguishing one, the other will keep reigniting it. That’s a perfect way to think about co-occurring disorders. A person isn’t just dealing with depression and an alcohol use problem; they are dealing with a single, intertwined condition where both parts need attention.
This is a far more common reality than many people realize. In fact, it’s a major public health challenge. According to the National Survey on Drug Use and Health, an estimated 21.2 million adults in the United States live with this dual diagnosis. These aren't isolated cases; they represent a huge number of people who need specialized, integrated care.
What This Looks Like in Real Life
The link between mental health and substance use is a two-way street. Someone struggling with anxiety might start self-medicating with alcohol to quiet their thoughts. On the flip side, someone else's heavy substance use can trigger or worsen underlying depression.
The main takeaway is that these are not separate problems to be solved one after the other. They are deeply connected. Because of this, trying to treat just one side of the equation rarely leads to lasting recovery.
At the heart of modern treatment is a simple but powerful principle: you have to address the mental health symptoms and the substance use together. If you ignore one, the other will almost certainly get worse, trapping you in a frustrating cycle of relapse and struggle.
To help you get a clearer picture, here’s a simple breakdown of the core concepts.
Key Aspects of Co-Occurring Disorders at a Glance
| Concept | Simple Explanation |
|---|---|
| Dual Diagnosis | Another common term for co-occurring disorders. |
| Intertwined Conditions | The mental health issue and substance use fuel each other. |
| Integrated Treatment | The most effective approach, addressing both conditions at once. |
| Self-Medication | Using substances to cope with or numb mental health symptoms. |
| Symptom Worsening | Substance use can trigger or intensify mental health struggles. |
Wrapping your head around this dynamic is the first step toward finding care that actually works. Once you see the deep connection between mental well-being and substance use, it becomes clear why a specialized, integrated approach is so vital. To dive deeper into one side of this equation, you can explore our guide on what is a substance use disorder.
How Mental Health and Substance Use Interact
The relationship between mental health and substance use is never a one-way street. It's a tangled, two-way interaction where each condition can trigger, worsen, and prolong the other. At its core, this is the very definition of co-occurring disorders. Understanding this dynamic is the first step toward seeing why specialized, integrated care is so critical.
Imagine someone struggling with severe social anxiety. The thought of a party or even a work event feels terrifying. One day, they might discover that having a few drinks loosens them up, making conversation feel easier. This temporary fix can quickly become a go-to coping mechanism—a pattern clinicians call self-medication. But over time, the alcohol use disrupts brain chemistry, often leading to even higher baseline anxiety when they aren't drinking.
A Cycle of Worsening Symptoms
It works the other way, too. Prolonged substance use can unmask or even directly cause a mental health condition. For example, heavy, long-term use of stimulants might trigger episodes of psychosis or paranoia in someone who has never experienced them before. In that scenario, the substance use isn't just a symptom; it's a direct cause that complicates the entire picture.
This simple but powerful equation is at the heart of what's often called a dual diagnosis.
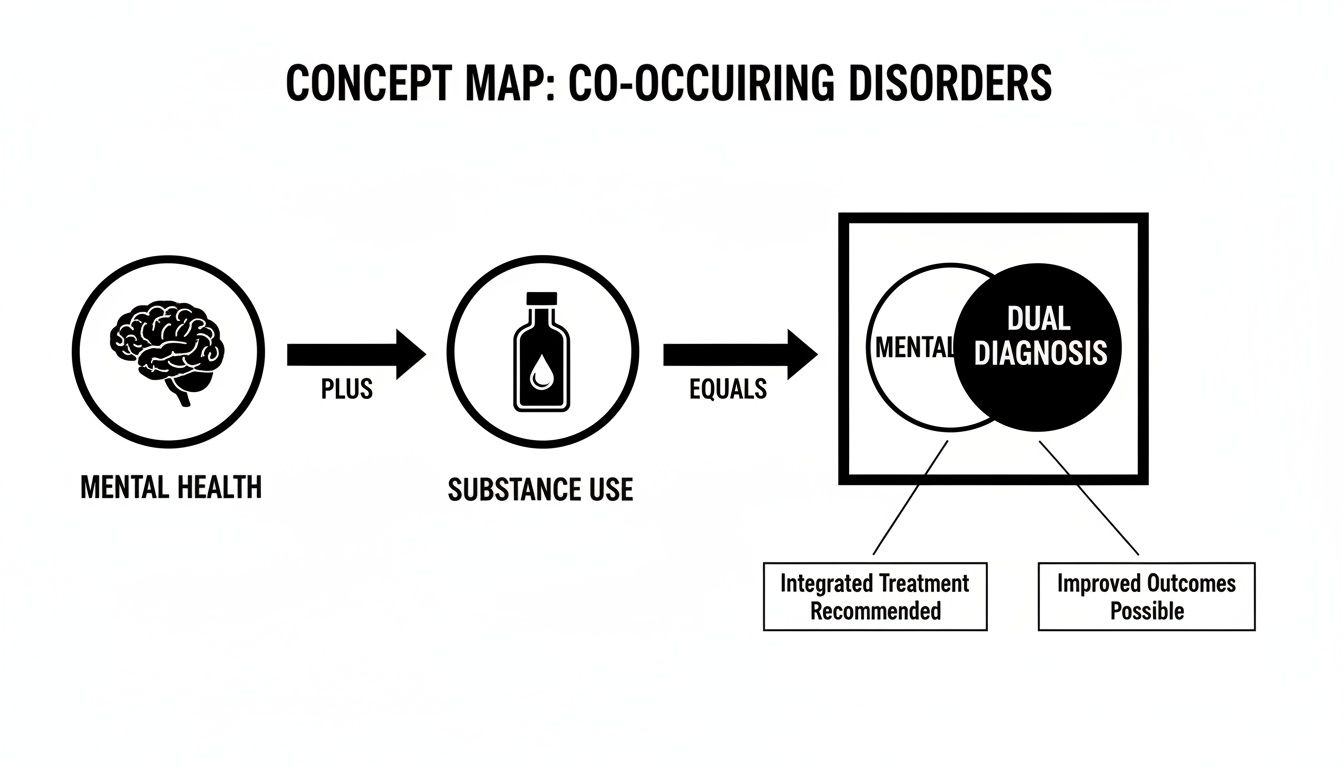
As you can see, the combination of these two distinct challenges creates a new, unified problem that demands an integrated solution.
Attempting to treat one issue while ignoring the other is like trying to fix a leaky boat by only bailing out water, without ever plugging the hole. Progress will be temporary at best, and the cycle will continue.
This constant push-and-pull is why so many people feel stuck. They might seek treatment for depression, but if their underlying alcohol use isn't addressed, their mood is unlikely to ever truly stabilize. Similarly, entering a detox program without also managing their anxiety disorder leaves them incredibly vulnerable to relapse the moment life's stressors return. You can learn more about how mental health and substance abuse are connected in our detailed guide.
Recognizing Common Co-Occurring Conditions
While the dance between substance use and mental health can look different for everyone, some patterns show up again and again. Getting familiar with these common pairings is a huge step toward making sense of your own experience or that of a loved one. It chips away at the feeling of isolation and shines a light on the most effective ways to get help.
Common Pairings and the Self-Medication Cycle
One of the classic connections we see is between depression and alcohol use disorder. When someone is buried under the weight of persistent sadness, alcohol can feel like a quick way to numb the pain. But this "self-medication" is a trap—alcohol is a depressant, and over time, it only digs the hole of depression deeper.
Another frequent duo involves anxiety disorders and sedatives like benzodiazepines. Someone battling generalized anxiety, panic attacks, or social phobia might use these drugs—prescribed or not—to find immediate calm. This can quickly spiral into physical dependence, and when the drug wears off, it often triggers rebound anxiety that’s even more ferocious than the original condition.
Trauma and Substance Use
The link between Post-Traumatic Stress Disorder (PTSD) and substance use is particularly powerful. Survivors of trauma often grapple with intrusive memories, a constant feeling of being on-edge, and overwhelming emotions. Many turn to substances like opioids or alcohol to escape these symptoms. It provides a temporary silence but keeps them from ever truly healing the underlying trauma.
These examples all point to the same core pattern: a substance is used as a solution to a problem it can never fix. This reality has been documented over and over in national health surveys, making co-occurring disorders a major public health issue.
To get a clearer picture of this widespread problem, you can read more about how behavioral health conditions are addressed.
Here’s a look at some of the most common pairings and why they often appear together.
Common Mental Health and Substance Use Pairings
| Mental Health Condition | Commonly Associated Substance Use Disorder | Potential Link |
|---|---|---|
| Depression | Alcohol Use Disorder | Alcohol provides temporary mood lift or numbness, but its depressant effects worsen symptoms long-term. |
| Anxiety Disorders | Benzodiazepines, Alcohol, Cannabis | Substances are used to calm racing thoughts or physical anxiety, but often lead to dependency and rebound symptoms. |
| PTSD | Alcohol, Opioids, Stimulants | Substances are used to numb intrusive memories, avoid emotions, or manage hypervigilance. |
| Bipolar Disorder | Alcohol, Cocaine, Cannabis | During manic phases, substances may be used to heighten euphoria; during depressive phases, to self-medicate sadness. |
| ADHD | Stimulants (non-prescribed), Alcohol, Cannabis | Substances may be used to increase focus (stimulants) or quiet a restless mind (alcohol/cannabis), but they disrupt executive function. |
| Personality Disorders | Polysubstance Use (multiple drugs) | Impulsivity and emotional dysregulation can drive the use of various substances to cope with intense feelings. |
These are just a few examples, but they illustrate how one condition can feed the other, creating a tangled knot that feels impossible to undo.
The specific combination of disorders is less important than recognizing the central theme: one condition is being used to manage the symptoms of the other. This creates an intertwined problem that absolutely requires a unified solution to break the cycle.
Why Integrated Treatment Is the Gold Standard of Care
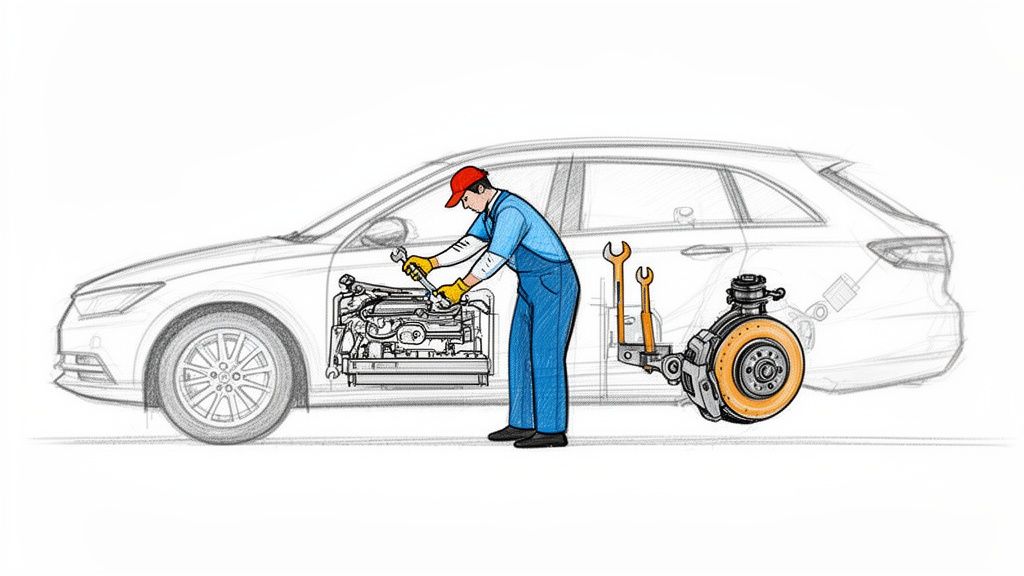
When you’re dealing with the tangled nature of co-occurring disorders, trying to treat just one condition while ignoring the other is like trying to fix a sinking boat one hole at a time. It’s an outdated and frankly, ineffective strategy. Today, evidence-based care has moved toward a unified approach called integrated treatment. This is now considered the gold standard because it addresses both the mental health and substance use disorders at the same time, with the same clinical team, under one cohesive plan.
Think of it like a skilled mechanic looking at your car. If the engine is misfiring and the brakes are shot, fixing only the engine doesn't make the car safe to drive. To get the car running properly and safely, both critical systems have to be repaired together. This simple but powerful logic is exactly why integrated care is so crucial for a dual diagnosis.
Unifying the Path to Recovery
In the past, treatment was often split up. A person might see a psychiatrist for their depression and a completely separate counselor for their substance use, with little to no communication between them. This fragmented approach often led to conflicting advice and painfully slow progress, as the untreated condition would consistently undermine any gains made in the other.
An integrated model recognizes that you simply cannot separate the two issues. It ensures that therapies for anxiety, for instance, also include strategies for managing cravings. It means relapse prevention skills are taught with a deep awareness of mental health triggers.
This holistic strategy is proven to lead to significantly better long-term outcomes, including:
- Lower rates of relapse and hospitalization.
- Improved psychiatric symptoms and overall daily functioning.
- Greater housing stability and life satisfaction.
- A more comprehensive and sustainable path to genuine healing.
As we dig into the benefits of integrated treatment, it can be insightful to compare different support systems, such as understanding the role of therapy compared to AI companionship. This approach provides the most complete and effective toolkit for recovery. For anyone seeking this level of care, you can learn more about integrated treatment for dual diagnosis and see how it builds a strong foundation for lasting well-being.
Recognizing The Signs In Yourself Or Someone You Love
Knowing the definition of co-occurring disorders is one thing, but spotting the signs in real life can be a whole lot harder. The symptoms of a mental health condition and a substance use disorder often get tangled up, masking each other and making it tough to see the full picture.
Recognizing these patterns is the first real step toward getting the right kind of help. These signs aren't about judgment or blame; they're simply clues that a deeper, more complex issue might be at play.
Behavioral And Emotional Warning Signs
How a person acts and feels often tells a powerful story. You might notice that someone’s mood swings become far more extreme after they’ve been drinking, or that their anxiety seems to spiral when they can’t use a particular substance. It's all about the patterns.
Keep an eye out for these shifts:
- Dramatic Shifts in Behavior: Obvious changes in personality, energy levels, or mood that seem directly linked to substance use.
- Social Withdrawal: Pulling away from friends, family, or hobbies that were once important. This often happens as a way to hide substance use or to cope with overwhelming mental health symptoms.
- Difficulty Managing Responsibilities: Struggling to keep up with work, school, or home life because of the combined weight of both conditions.
- Using Substances to Cope: This is a big one. You might hear them talk openly about needing a drink or a drug to relax, fall asleep, or just to face a social situation.
Perhaps the biggest red flag of all is a history of seeking treatment for one condition—like depression or anxiety—that consistently fails. If progress is always short-lived, it's often because an unaddressed substance use issue is quietly undermining the entire healing process.
Recognizing The Statistical Reality
This powerful connection between substance use and mental health isn't just anecdotal—the numbers tell the same story. Research shows that 37% of people with alcohol use disorders also have at least one serious mental illness.
That figure jumps to a staggering 53% for individuals with other drug use disorders.
If these signs feel familiar, remember that simply recognizing them is a sign of strength, not weakness. Understanding your own emotional landscape is critical, and practices like exploring the benefits of journaling for mental health can provide incredible self-insight. For a closer look at a specific substance, you can review the warning signs of alcohol addiction.
Answering Your Questions About Co-Occurring Disorders
When you’re trying to make sense of a dual diagnosis, a lot of questions pop up. Getting straight answers is the first step toward making a clear-headed decision about getting help. Let's tackle some of the most common ones.
Which Comes First: The Mental Health Issue or The Addiction?
This is the classic "chicken or egg" question, and honestly, there's no single answer. It plays out differently for everyone.
Sometimes, a mental health condition like anxiety or depression comes first. Someone might start using substances as a way to self-medicate, just trying to quiet the noise in their head or numb overwhelming feelings. In other cases, it’s the other way around. Heavy, long-term substance use can physically change the brain's chemistry, triggering a mental health issue that wasn't there before or making a mild one much worse.
Most often, the two conditions develop in tandem, feeding off each other in a vicious cycle.
Ultimately, trying to pinpoint which one started first is less important than recognizing that both need to be treated together. The real goal is to break the current cycle, not to perfectly map its origins.
Is Recovery From Co-Occurring Disorders Harder?
It can be more complex, but "harder" isn't the right word. With the right approach, recovery is absolutely achievable. The non-negotiable key is integrated treatment—a plan that addresses both the mental health condition and the substance use simultaneously.
If you only treat one, the other is left to act as a constant trigger. Imagine getting therapy for depression but continuing to drink heavily; the alcohol will just keep undermining any progress you make. A truly comprehensive program gives you the specific skills and therapies needed to manage both sets of symptoms, creating a much stronger foundation for lasting well-being.
Can I Manage a Co-Occurring Disorder Without Professional Help?
While things like support groups, journaling, and self-help books are fantastic tools for any recovery journey, the sheer complexity of a dual diagnosis nearly always requires professional, evidence-based care. Just getting an accurate diagnosis is a critical first step, and that can only be done by a qualified clinician.
A professional team provides essential support you just can't replicate on your own, including:
- Medical Oversight: To keep you physically safe, especially during the detox and withdrawal phase.
- Medication Management: To prescribe and adjust medications that can stabilize psychiatric symptoms and make therapy more effective.
- Specialized Therapies: To get to the root causes driving both conditions.
What Is The Best Therapy For Co-Occurring Disorders?
There's no single "best" therapy, as every effective treatment plan is personalized. However, a few specific models have proven incredibly successful for people navigating a dual diagnosis.
- Cognitive Behavioral Therapy (CBT): This is all about helping you spot, challenge, and change the destructive thought patterns and behaviors that connect your mental health struggles to your substance use.
- Dialectical Behavior Therapy (DBT): This approach is a game-changer for teaching emotional regulation, mindfulness, and distress tolerance. These are crucial skills for managing the intense feelings that can trigger both mental health symptoms and cravings.
- Eye Movement Desensitization and Reprocessing (EMDR): For anyone whose substance use is tangled up with trauma, EMDR can be a profoundly powerful tool for healing the underlying wounds that often fuel the cycle of self-medication.
The best programs don't just pick one; they use a mix of these therapies to build a complete and resilient recovery toolkit that's tailored to you.
At Altura Recovery, we specialize in providing the integrated, evidence-based care needed to effectively treat co-occurring disorders. Our team of compassionate professionals is ready to help you or your loved one find the path to real healing. Learn more about our dual diagnosis programs and start your journey today.