Stopping Valium, known medically as diazepam, isn't as simple as just deciding to quit. Attempting to do so on your own can be dangerous, even life-threatening. This isn't about willpower; it's about brain chemistry. The brain has grown to physically rely on the drug to stay balanced, and pulling it away abruptly can trigger severe consequences like seizures.
Why Valium Withdrawal Requires Medical Supervision
Think of your brain's activity level like the volume dial on a stereo. Valium's job is to turn that volume way down, creating a sense of calm by boosting GABA, the brain's main "off switch" neurotransmitter. Over time, your brain gets so used to this quieted state that it forgets how to turn down its own volume, producing less of its natural calming chemicals.
This is what doctors call physical dependence. The brain now needs Valium just to maintain a normal, stable state. If you suddenly take the drug away, it’s like yanking the volume knob from a one all the way to a ten. Without Valium there to press mute, brain activity surges out of control, sparking the intense and risky symptoms of withdrawal.
The Dangers of an Unbalanced System
This sudden, chaotic surge of neural activity is precisely what makes quitting "cold turkey" so hazardous. Your central nervous system is thrown into a state of hyper-excitement, which can set off a chain reaction of severe physical and psychological symptoms. These aren't signs of personal weakness—they are a direct, physiological response to a dramatic chemical imbalance.
This is a widespread problem. By 2015-2016, an estimated 30.5 million American adults had used benzodiazepines. Of those who misused them, more than 20% were using Valium specifically. These staggering numbers reveal just how many people are facing the difficult, and often misunderstood, journey of withdrawal. You can find more details about Valium use statistics and the public health impact they represent.
Abruptly stopping Valium is not a test of willpower; it is a neurological shock to the system. Medically supervised withdrawal is designed to safely and gradually guide the brain back to its natural balance, preventing the dangerous rebound effects that can occur.
A Path to Safe and Stable Recovery
The only proven, safe way to navigate Valium withdrawal is with medical management. This involves a carefully planned tapering schedule, where a doctor slowly reduces your dosage over weeks or even months. This gradual step-down gives your brain the time it needs to readjust and start producing its own calming neurotransmitters again, which keeps withdrawal symptoms from becoming overwhelming or dangerous.
This is where professional support is non-negotiable. Clinicians create a personalized tapering plan while providing the oversight needed to keep you safe. Proper medication management for mental health and withdrawal can ensure you are not only out of harm's way but also as comfortable as possible during this tough transition. With the right medical strategy, you can sidestep the life-threatening risks of unsupervised detox and build a solid foundation for a lasting recovery.
Navigating the Valium Withdrawal Timeline and Symptoms
Figuring out the timeline for Valium withdrawal can be tricky, mainly because it doesn't play by the same rules as other substances. Valium has a long half-life, which is just the technical way of saying it takes a long time for the drug to leave your system. Because of this, withdrawal symptoms often show up much later than people expect, catching them completely off guard.
This delay can create a false sense of security, making you think you've dodged a bullet. That’s precisely why having professional medical guidance is so important. The whole process is really about your brain recalibrating itself after getting used to having Valium around to keep things calm.
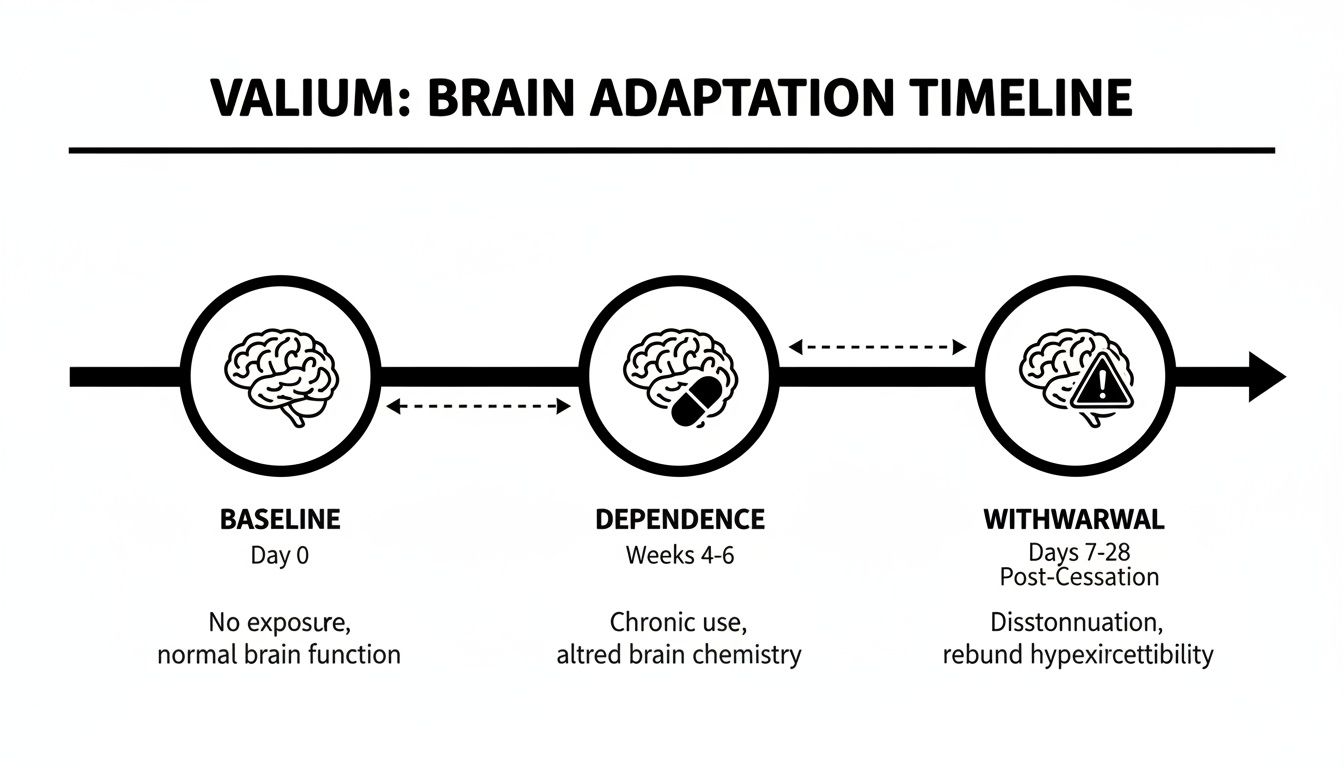
As this image shows, the brain goes from its normal baseline state, to a state of dependence, and then through the difficult withdrawal phase as it relearns how to function without the drug's influence.
The Early Phase: Onset Within Days
The first hints of withdrawal usually start between 1 to 4 days after the last dose. This is a stark contrast to short-acting benzos, where you might feel sick within hours. Valium’s lingering presence is what causes the delay.
At first, the symptoms are often subtle but they build over time. You'll likely notice:
- A major spike in anxiety and restlessness, often called "rebound anxiety."
- Trouble falling asleep or staying asleep, leading to insomnia.
- A general sense of irritability and feeling on edge.
These early signs are your central nervous system starting to wake up and react to the absence of a drug it has learned to rely on.
The Acute Phase: Peak Withdrawal Symptoms
This is the toughest stretch. It typically kicks in around the first week and can last for two to four weeks. During this window, symptoms hit their peak intensity as your body works overtime to get its brain chemistry back in balance.
While Valium's half-life can vary, withdrawal symptoms often ramp up quickly, peaking within the first 1 to 4 days of this phase. People can experience intense anxiety, tremors, muscle spasms, nausea, and powerful cravings.
During the acute phase, the brain is essentially in a state of hyper-excitement. The symptoms experienced—from muscle spasms to heightened anxiety—are direct results of the nervous system over-firing without Valium to suppress it. This is the most critical time for medical monitoring.
Many people find that supplementing with certain nutrients can help manage the intense symptoms. For example, some find that a magnesium glycinate supplement for sleep, anxiety, and recovery can help take the edge off and support the nervous system.
The Post-Acute Phase: Lingering Symptoms
Once the most severe physical symptoms start to fade, some people move into a stage known as Post-Acute Withdrawal Syndrome, or PAWS. This phase isn't about intense physical sickness; it's more about persistent psychological and emotional symptoms.
PAWS can drag on for several months, with symptoms that tend to come and go in waves. These often include:
- Lingering anxiety and depression
- Mood swings and irritability
- Chronic fatigue and low energy
- Cognitive issues like "brain fog" or memory problems
Understanding PAWS is key for long-term recovery. These lingering effects can be a huge trigger for relapse if you don’t know what’s happening or how to manage it. You can learn more about Post-Acute Withdrawal Syndrome in our detailed guide to be better prepared for this stage.
Having a structured timeline can help set realistic expectations for what’s ahead. Below is a general overview of what to expect during the different phases of withdrawal.
A Typical Valium Withdrawal Timeline
This table breaks down the withdrawal journey into its core phases, giving you a general idea of the timeline and the kinds of symptoms that are common at each stage.
| Withdrawal Phase | Typical Onset After Last Dose | Peak Severity | Common Symptoms |
|---|---|---|---|
| Early Withdrawal | 1-4 days | 4-7 days | Increased anxiety, insomnia, irritability, restlessness. |
| Acute Withdrawal | 4-7 days | 7-14 days | Severe anxiety, tremors, muscle pain, nausea, sweating, potential for seizures. |
| Post-Acute (PAWS) | After 2-4 weeks | Varies (comes in waves) | Mood swings, depression, sleep disturbances, fatigue, cognitive fog. |
Think of this table as a general roadmap, not a strict schedule. Everyone's experience is unique. Factors like how much you were taking, for how long, and your overall health all play a role in the timeline and severity of your symptoms. This is why a personalized, medically supervised plan is always the safest and most effective approach.
The Dangers of an Unsupervised Valium Detox Can Be Life-Threatening
Trying to quit Valium on your own isn't just a matter of gritting your teeth through a rough patch. It's a dangerous gamble with your brain's chemistry. This isn't about willpower; it's about navigating a period of profound neurological instability that carries severe, sometimes fatal, risks. The danger is baked right into how the drug works.
Valium boosts GABA, the brain's primary calming neurotransmitter, essentially putting a powerful brake on your central nervous system. After long-term use, your brain adapts by producing less of its own GABA and becoming less sensitive to it. If you suddenly yank the drug away, you're not just taking off the brake—you're slamming the accelerator on a system that has forgotten how to slow itself down. The result is a state of extreme, chaotic overactivity.
The Real Risk of Seizures
The most frightening consequence of this neurological rebound is a grand mal seizure. This is what happens when the brain's electrical activity becomes so disorganized that it triggers violent convulsions, a complete loss of consciousness, and powerful muscle contractions. It is the ultimate sign of a central nervous system in full-blown crisis.
Think of your brain as a complex electrical grid that Valium has been forcing to run at a low, steady voltage. Quitting cold turkey is like hitting that grid with a massive, unexpected power surge. The circuits overload, causing a system-wide failure that can erupt as a seizure. While the risk peaks during the acute phase of withdrawal, a seizure can strike without warning, making medical supervision non-negotiable.
When Psychological Distress Becomes a Medical Emergency
Beyond the physical storm, the psychological fallout from a cold-turkey detox can be just as devastating. The abrupt absence of GABA's calming influence can unleash severe mental health crises that are a world away from typical anxiety or moodiness.
These complications aren't just uncomfortable—they're medical emergencies:
- Psychosis: This can mean experiencing hallucinations, delusions, and a total disconnect from reality, making it impossible to function or stay safe.
- Extreme Psychological Distress: This isn't just feeling anxious. It’s debilitating panic attacks, intense paranoia, and a constant, overwhelming sense of terror or dread.
- A Spike in Suicide Risk: The crushing weight of deep depression, hopelessness, and severe anxiety can dramatically increase the risk of suicidal thoughts and actions.
These symptoms are not a reflection of someone's character. They are the direct, predictable outcome of a brain thrown into severe chemical imbalance and require immediate professional help.
"The rebound effect during Valium withdrawal is a critical concern. The original symptoms the drug was prescribed for—like anxiety or insomnia—can return with a vengeance, often becoming far more severe than they were initially. This intense rebound can feel unbearable and often drives relapse."
The Perilous Cycle of Relapse and Overdose
This intense rebound, combined with overwhelming cravings, creates a perfect storm for relapse. Anyone suffering through an unmanaged withdrawal might understandably reach for Valium again, desperate for the symptoms to stop. But that one moment of seeking relief can turn fatal.
A person's tolerance to Valium drops dramatically after even a short period of abstinence. Taking the same dose they used before trying to quit can easily overwhelm their system, leading to a life-threatening overdose. This is precisely why the World Health Organization advises a slow, medically supervised dosage taper over several days.
The statistics are a grim reminder of the stakes. Tragically, in 2014, nearly 8,000 people died from benzodiazepine overdoses, with many of these deaths linked to these exact withdrawal-relapse cycles. You can learn more about how withdrawal contributes to overdose risk. These numbers show the stark reality: what feels like a desperate search for relief can quickly become a fatal mistake.
Proven Medical Strategies for a Safe Valium Taper
If there’s one non-negotiable rule for coming off Valium, it's this: never stop abruptly. The gold standard for safely discontinuing this medication is a slow, methodical process known as tapering, which must be supervised by a medical professional. This involves gradually reducing your daily dose over an extended period.
Think of it like descending a steep mountain. Rushing down is a surefire way to get seriously hurt. The safe way involves taking small, calculated steps along a planned route, giving your body time to adjust to each new altitude. Tapering works the same way for your brain, preventing the neurological shock that triggers severe withdrawal.
This gradual reduction is essential. It gives your brain’s GABA system the time it needs to slowly come back online and start producing its own calming neurotransmitters again. The goal is to keep withdrawal symptoms manageable and, most importantly, to avoid life-threatening complications like seizures.
Tailoring the Tapering Plan
There is no such thing as a "one-size-fits-all" tapering schedule. A safe and effective plan has to be meticulously customized by a doctor, who will weigh several critical factors to structure your taper.
Key factors include:
- Current Dosage: Higher daily doses almost always require a longer, more gradual taper.
- Duration of Use: The longer you’ve taken Valium, the more your brain has adapted, demanding a slower process.
- Individual Health: Your overall physical and mental health, including any co-occurring conditions, plays a major role.
- Personal Response: Your doctor will closely monitor how you feel after each dose reduction and adjust the pace accordingly.
This personalized approach is exactly why trying to taper on your own is so risky. A physician can make real-time adjustments to ensure the process remains safe and tolerable—something that’s impossible to do without clinical oversight.
Common Tapering Strategies
Doctors rely on evidence-based methods to structure a Valium taper. While the specific schedule will be unique to you, it will likely follow one of two established strategies designed to maximize safety and minimize withdrawal symptoms.
- Direct Tapering: This is the most straightforward approach. Your doctor creates a schedule to gradually lower your daily Valium dose. For instance, they might decrease it by a small amount every one to two weeks, carefully watching your reaction before the next step down.
- Substitution Tapering: Sometimes, a person might be on a short-acting benzodiazepine. In these cases, a doctor may first switch them to a long-acting one like Valium, stabilize them on an equivalent dose, and then begin the taper. The longer half-life creates a smoother, more stable withdrawal experience by preventing sharp peaks and valleys in the drug's concentration in your system.
A well-structured tapering plan is the cornerstone of a successful withdrawal. Studies show that with a professionally managed, gradual taper, an estimated 65-80% of individuals can discontinue benzodiazepine use successfully. This highlights just how effective a slow, controlled approach is compared to stopping suddenly.
Throughout the taper, your medical team provides crucial support, which often includes non-addictive medications to manage specific symptoms like nausea or insomnia. This is a key part of what’s known as medication-assisted treatment, or MAT. To understand this better, you can explore how medication-assisted treatment supports recovery in our detailed guide. This comprehensive care transforms a potentially dangerous process into a manageable, medically sound journey.
Choosing the Right Support for Your Recovery Journey
Figuring out how to manage Valium withdrawal isn't just about getting through the symptoms—it's about picking the right place to do it safely. The two main paths are inpatient medical detox and outpatient withdrawal management. The best one for you comes down to your unique situation, and making this choice is one of the most critical decisions at the start of your recovery.
An inpatient facility offers the highest, most intensive level of care. Think of it as a protected bubble where you live on-site 24/7 during the toughest parts of withdrawal. This constant medical supervision is designed to manage severe symptoms and, most importantly, respond instantly to emergencies like seizures.
Outpatient management, on the other hand, gives you medical guidance and therapy while you continue living at home. This route offers a lot more flexibility, letting you keep up with work, school, or family life. For it to work, though, you absolutely need a stable and supportive home environment.
When Inpatient Medical Detox Is Essential
For some people, going to an inpatient facility isn't just a preference—it's a medical necessity. This level of support is crucial when the risk of severe, or even life-threatening, complications is high. A clinical team will strongly recommend an inpatient stay if certain factors are in play.
Consider an inpatient program if any of these apply to you:
- High-Dose or Long-Term Dependence: If you've been taking large amounts of Valium for a long time, the risk of dangerous withdrawal symptoms, including seizures, goes way up.
- History of Seizures: Anyone who has experienced seizures before—either during a previous withdrawal attempt or due to another condition—needs 24/7 medical oversight. No exceptions.
- Co-Occurring Conditions: Serious mental health disorders like severe depression, bipolar disorder, or psychosis can be dangerously destabilized by withdrawal, requiring close psychiatric monitoring.
- Unstable Home Environment: Trying to detox in a chaotic or stressful home, especially one without support or where others are using substances, makes a safe outpatient process nearly impossible.
This is a major public health concern. Treatment admissions for diazepam actually jumped sevenfold between 2003 and 2012. While the numbers have leveled off since then, they remain high, showing just how persistent the challenge of managing Valium withdrawal safely is. Medical detox programs are specifically designed to prevent the brutal, lingering symptoms like deep anxiety and insomnia that can drag on for months.
Finding Success with Outpatient Support
Outpatient withdrawal management can be a fantastic and effective option for individuals who fit a specific profile. The ideal candidate usually has a lower-dose dependency and is in good physical and mental health. The real key to making it work is having a rock-solid foundation at home.
The success of outpatient care hinges on a robust support system. When family and friends are engaged and the home environment is stable, individuals can effectively manage withdrawal while staying connected to their daily lives and responsibilities.
Professional outpatient services, like those we offer at Altura Recovery, provide the necessary medical supervision and therapeutic guidance for a safe taper. This includes regular check-ins with our medical team, medication management to ease symptoms, and counseling to help you work through the psychological side of recovery. It’s a structured yet flexible path for those who don’t need around-the-clock monitoring.
To help clarify which path might be a better fit, let's compare the two side-by-side.
Comparing Inpatient and Outpatient Valium Withdrawal Support
| Feature | Inpatient Medical Detox | Outpatient Withdrawal Management |
|---|---|---|
| Environment | Live-in facility with 24/7 medical supervision. | Live at home, attend scheduled appointments. |
| Medical Oversight | Constant monitoring of vital signs and symptoms. | Regular check-ins with medical staff. |
| Ideal Candidate | High-dose use, history of seizures, severe co-occurring disorders, unstable home life. | Lower-dose use, good overall health, stable and supportive home environment. |
| Flexibility | Low; requires taking time off from work, school, and other responsibilities. | High; allows you to maintain daily routines and commitments. |
| Emergency Response | Immediate, on-site medical intervention available 24/7. | Relies on the individual to seek emergency care if needed. |
| Peer Support | Structured, on-site access to peers going through the same process. | Group therapy sessions provide peer connection during appointments. |
Ultimately, the goal is to match the intensity of your care to the intensity of your needs. For those who can safely manage withdrawal from home, it’s vital to understand how to build a support system that provides both encouragement and accountability. This network becomes your safety net, helping you navigate challenges as they arise and reinforcing your commitment to getting well.
Building a Foundation for Lasting Recovery
Getting through the physical gauntlet of Valium withdrawal is a huge win, but it’s really just clearing the runway. True, lasting recovery means building a whole new life from the ground up—one that addresses not just the physical side of dependence, but the psychological reasons you started using in the first place. This is where professional, structured support shifts from a service to a partnership.
Think of it like this: the withdrawal process is like clearing a plot of land after a hurricane. The initial detox is all heavy lifting—hauling away downed trees and making the area safe. But a cleared lot isn't a home. The next, and most important, phase is about carefully designing and building a new, resilient structure with the right tools and a solid blueprint.
From Detox to Daily Life
This transition is best managed through a "step-down" model of care. The idea is simple: the intensity of support gradually decreases as your own coping skills and confidence grow. It starts with maximum support during the acute withdrawal phase and then methodically transitions to ongoing outpatient therapy and relapse prevention planning. This approach ensures you’re never left without a safety net as you reclaim your independence.
This isn't a niche problem; it's a global one. Benzodiazepine prescriptions are highest across North America and Western Europe, creating widespread withdrawal challenges. Here in the U.S., where over 30 million adults recently used benzos like Valium, the fallout is clear. In 2022, benzodiazepines were involved in a staggering 73% of emergency room visits for multi-substance cases.
The Essential Tools for Rebuilding
A comprehensive recovery program uses a combination of medical and therapeutic tools to build this new foundation. These pieces work together, addressing every facet of Valium dependence from brain chemistry to daily habits.
Key components of long-term care include:
- Ongoing Medical Monitoring: Even after the taper is done, regular medical check-ins ensure your physical and mental health stay stable. This is critical for catching and managing any post-acute symptoms that might pop up weeks or even months later.
- Integrated Therapies: This is where the real change happens. Modalities like Cognitive-Behavioral Therapy (CBT) are crucial for helping you identify the thought patterns and behaviors that led to substance use, then replacing them with healthier coping skills that actually work.
- Relapse Prevention Planning: This isn't a generic worksheet. It's a personalized strategy to map out your specific triggers—whether it’s stress, a certain social circle, or a particular emotional state—and develop a clear, actionable plan for what to do when you encounter them.
Lasting recovery isn't about erasing the past. It’s about building a future where you have the skills, support, and confidence to handle life’s challenges without turning back to a substance. It's an active, ongoing process of growth.
Cultivating a Supportive Environment
A huge part of this journey happens outside the clinic walls. It's about consciously creating a life that supports your sobriety, from your daily routines and relationships to your overall well-being. As you build this new foundation, it can be incredibly helpful to explore health and wellness resources that reinforce your new lifestyle.
At Altura Recovery, our outpatient services are specifically designed to guide you through this transition. We provide the medical oversight for a safe withdrawal and the therapeutic support to build a strong psychological foundation. By integrating care into your daily life, we help you construct a resilient, sustainable recovery—one step at a time.
Common Questions About Valium Withdrawal
When you’re facing Valium withdrawal, you’re bound to have urgent, specific questions. Let's cut through the noise and get straight to the facts, reinforcing the most critical safety information from this guide.
Can I Taper Off Valium on My Own at Home?
Absolutely not. This is incredibly dangerous and something medical professionals strongly advise against. Trying to manage a withdrawal from Valium without a doctor's supervision opens the door to severe symptoms, including seizures that can be fatal. A physician is non-negotiable for creating a safe, personalized taper schedule and stepping in if any complications pop up.
How Long Does Valium Withdrawal Last?
This is different for everyone. The most intense phase, known as acute withdrawal, typically lasts anywhere from one to four weeks. But it's important to understand that a medically supervised taper is a much longer game, often stretching over several months. This slow-and-steady approach is what allows your brain and body to adjust safely.
It’s also crucial to know about Post-Acute Withdrawal Syndrome (PAWS).
PAWS isn't about physical detox; it's the lingering psychological symptoms like anxiety, mood swings, or sleep problems that can show up in waves for months after the acute phase is over. This is a powerful reminder that ongoing support is vital long after you’ve physically stabilized.
What Medications Help Manage Valium Withdrawal Symptoms?
The main "medication" is actually Valium (diazepam) itself, used in a meticulously controlled tapering plan. This lets your body ease off the substance slowly and safely. To handle specific symptoms that pop up along the way, doctors might prescribe other non-addictive medications. These can help with things like nausea, insomnia, or intense spikes of anxiety. Any extra medication must be chosen and managed by a doctor who understands your specific health needs.
Getting through Valium withdrawal is a journey that demands expert medical guidance and genuine, compassionate support. At Altura Recovery, our outpatient programs are designed to provide the medical oversight and therapy you need to detox safely while still managing your daily life. If you're ready to take that first step, you can learn more about our approach at https://www.alturarecovery.com.