Let's get straight to the point: Does naltrexone actually work?
The answer is a clear yes. Naltrexone is an FDA-approved medication that has proven effective for treating both Alcohol Use Disorder (AUD) and Opioid Use Disorder (OUD). It isn't a magic pill, but it's a powerful, science-backed tool that helps people break the cycle of addiction when it feels impossible.
A Shield for the Brain: How Naltrexone Supports Recovery
When you're trying to overcome a substance use disorder, you’re not just fighting a bad habit—you're up against powerful, deeply ingrained brain chemistry. Naltrexone gives you a significant advantage by stepping directly into that biological process.
Think of it as a circuit breaker for the brain's reward system. It doesn’t create a new feeling or a "high." Instead, it blocks the euphoric effects that alcohol and opioids produce, effectively putting up a shield around the receptors they target.
This is the key. By preventing the substance from delivering its expected "reward," naltrexone helps cravings fade over time. This neurological support creates the mental space you need to fully engage in therapy, learn new coping skills, and focus on healing.
Before we get into the nuts and bolts, here's a quick summary of naltrexone's key benefits and applications, giving you a high-level overview before we dive into the details.
Naltrexone Effectiveness at a Glance
| Disorder Type | How It Works | Primary Outcome | Global Recognition |
|---|---|---|---|
| Alcohol Use Disorder (AUD) | Blocks opioid receptors, reducing the rewarding effects of alcohol. | Reduces heavy drinking days, lowers relapse risk, and diminishes cravings. | Endorsed by the World Health Organization (WHO) and SAMHSA. |
| Opioid Use Disorder (OUD) | Occupies opioid receptors, blocking the euphoric effects of heroin, fentanyl, or pain pills. | Helps prevent relapse in detoxified patients by removing the "reward" of use. | A core component of Medication-Assisted Treatment (MAT) guidelines. |
Now that you have the big picture, let's explore how this medication functions in the real world.
A Roadmap to Understanding Naltrexone
This guide is designed to give you clear, straightforward answers without the confusing medical jargon. Here’s what we’ll cover:
- The Science Explained: How naltrexone works on a biological level to interrupt the addiction cycle.
- Targeted Applications: Its specific effectiveness for both alcohol and opioid use disorders, backed by evidence.
- Treatment Options: The crucial differences between daily oral pills and the monthly extended-release injection (Vivitrol).
- Integrated Care: Why naltrexone is most successful when combined with a comprehensive recovery plan.
At its core, naltrexone provides a biological shield, giving you a better chance to focus on the psychological and behavioral work of healing. It helps level the playing field, making long-term recovery a more attainable goal.
By the end of this guide, you won't just know if naltrexone works—you'll have a solid understanding of how it works. At facilities like Altura Recovery, integrating medication-assisted treatment (MAT) with personalized therapy is fundamental. This approach treats the whole person, addressing both the physical dependence and the underlying causes of addiction. Our goal is to empower you with knowledge so you can make confident decisions on your recovery journey.
How Naltrexone Interrupts the Addiction Cycle
To really get why naltrexone works, we have to look at what’s happening inside the brain. Think of your brain’s opioid receptors as a series of locks. Substances like opioids and even alcohol act like keys that fit these locks, turning them to release a flood of feel-good chemicals like dopamine and endorphins. That rush creates an intense sense of reward and pleasure.
Addiction sinks its hooks in when the brain starts chasing that artificial high, rewiring itself to seek the substance over and over. This is where naltrexone steps in. It’s like a master key that slides perfectly into those same locks but doesn’t turn them. It just sits there, taking up space.
By binding to these opioid receptors, naltrexone acts as a blocker, or an antagonist. So when the original key—the alcohol or opioid—tries to get in, it finds the lock is already occupied. The substance is physically blocked from activating the receptor, meaning the expected euphoric rush never comes.
Breaking the Reward Cycle
This blockade is the secret to how naltrexone breaks the addiction cycle. It severs the deep-seated psychological link between using a substance and feeling a reward. When someone on naltrexone takes a drink or uses an opioid, the experience is blunted. The high they were expecting is either dramatically reduced or completely gone.
This isn’t just about stopping one high; it’s about retraining the brain. Over time, when the brain stops getting that anticipated reward, the powerful, gnawing cravings begin to fade. The motivation to use weakens simply because the payoff isn't there anymore.
This biological assist is crucial. It quiets the physical pull of addiction, giving people the mental space and stability they need to dig into the real work of recovery. It highlights the critical difference between psychological and physical dependence, both of which have to be addressed for healing to stick.
The Science of Receptor Occupancy
Naltrexone’s power lies in its ability to occupy a very high percentage of these brain receptors and to hang on tight for a long time. This creates a steady, reliable shield that helps protect against relapse and gives the brain a chance to rewire its response to triggers.
Pharmacologically, naltrexone has a very strong attraction, or affinity, for these receptors. Research shows that even at standard doses, it can achieve near-complete brain occupancy of certain opioid receptors, creating a durable blockade. This means a single oral dose can protect a person from the effects of opioids for 72 to 108 hours. For a deeper dive, you can explore the WHO's landmark public health decisions regarding essential medicines for alcohol use disorders.
This long-lasting action is vital for a few reasons:
- It Reduces Decision Fatigue: It takes the daily, sometimes hourly, battle of willpower off the table.
- It Provides a Safety Net: It offers real protection against an impulsive decision to use, preventing a slip from becoming a full-blown relapse.
- It Creates Space for Therapy: By turning down the neurological "noise" of cravings, it helps people engage more meaningfully in counseling and behavioral therapies.
Naltrexone doesn't cure addiction on its own. Instead, it creates a crucial window of opportunity. By managing the physical cravings, it empowers a person to do the emotional and psychological work necessary for long-term recovery.
In short, naltrexone helps level the playing field. It gives the brain a chance to heal and recalibrate its reward system back to normal, where pleasure comes from healthy sources, not substances. Once you understand this mechanism, it’s clear how naltrexone works as an indispensable tool in a comprehensive treatment plan.
The Evidence: Does Naltrexone Actually Work for Alcohol Cravings?
When it comes to treating Alcohol Use Disorder (AUD), the buzz around naltrexone isn't just hype. Its effectiveness is grounded in solid clinical data and recognized by major global health authorities. This isn't just another option; it's a cornerstone of modern medication-assisted treatment for alcohol dependence for a very good reason.
One of the biggest endorsements came recently when the World Health Organization (WHO) added naltrexone to its prestigious Essential Medicines List. This isn't just a small administrative update. It’s a global stamp of approval, signaling that the medication meets tough criteria for effectiveness, safety, and public health impact. It solidifies naltrexone's role in tackling the worldwide treatment gap for AUD.
So, what does that mean for you or someone you care about? It means that when you ask, "does naltrexone work?" the answer is a firm "yes," backed by extensive research showing it can genuinely change the trajectory of someone's recovery.
Taming Heavy Drinking and Slashing Relapse Risk
The main job of naltrexone in AUD treatment is to dial down the rewarding effects of alcohol. When the brain stops getting that pleasurable "hit," the powerful cravings start to fade, which helps prevent a return to heavy drinking. And the research confirms it's very good at this job.
A landmark analysis that pooled data from numerous clinical trials found that people treated with naltrexone were 17% less likely to return to any drinking and 19% less likely to return to heavy drinking compared to those who received a placebo.
These aren't just abstract numbers; they represent real, tangible change. For someone in recovery, that translates to fewer days lost to alcohol and more days building a stable, fulfilling life. The medication acts like a crucial buffer, short-circuiting the addictive feedback loop that makes quitting so incredibly difficult.
Even better, studies show naltrexone significantly reduces the number of heavy drinking days for those who do have a slip. This is a critical benefit. It helps keep a momentary lapse from spiraling into a full-blown relapse, giving people a much better shot at getting right back on track.
The Real-World Impact on Health and Survival
Beyond just managing drinking patterns, the evidence shows naltrexone has a life-saving impact. A massive national study of U.S. veterans uncovered profound long-term benefits, demonstrating that patients with AUD treated with naltrexone had a significantly lower risk of death than those who went without it.
That effect was even stronger when naltrexone was paired with supportive therapies. This highlights a key point: naltrexone works best as part of a structured recovery program, not as a magic pill on its own. It provides the neurological stability needed to fully engage with the other essential parts of healing.
- Behavioral Therapy: By quieting the brain's constant demand for alcohol, naltrexone helps people focus on learning new coping skills in therapies like Cognitive Behavioral Therapy (CBT).
- Support Groups: With cravings under control, a person can participate more meaningfully in peer support groups, building the community and accountability that are so vital to recovery.
- Mindfulness and Stress Management: The mental space that opens up allows individuals to practice techniques that address the underlying triggers for drinking. You can find valuable tools in guides detailing mindfulness exercises for stress relief, which work hand-in-hand with the biological support from naltrexone.
Closing a Critical Treatment Gap
Despite its proven success, a shocking number of people who could benefit from naltrexone never receive it. The gap between those who need help for AUD and those who actually get it is immense. Medications like naltrexone are vital tools for closing this gap, offering an accessible, evidence-based option that can be seamlessly integrated into outpatient care.
By making alcohol less rewarding, naltrexone empowers people to break free from the exhausting cycle of craving and consumption. The evidence is clear: it's an indispensable tool that helps people regain control, reduce harm, and build a lasting foundation for recovery.
Using Naltrexone for Opioid Use Disorder
When it comes to treating Opioid Use Disorder (OUD), naltrexone carves out its own unique and vital path. It works differently than other common medications like methadone or buprenorphine. Those medications partially activate the brain's opioid receptors (they’re called agonists), but naltrexone is a non-agonist.
This means it doesn't activate those receptors at all. Because of this, it carries zero risk of dependence or addiction.
Think of naltrexone as a complete shield for the brain. It fully blocks the opioid receptors, making it impossible for drugs like heroin, fentanyl, or prescription painkillers to deliver their euphoric high. This approach is incredibly valuable for people who are highly motivated to recover or who simply prefer a treatment that is entirely non-addictive.
By taking the "reward" out of the equation, naltrexone helps break the powerful psychological loop of addiction. When someone knows there will be no high, the urge to use opioids starts to fade—a massive step toward lasting recovery.
The Crucial Role of Treatment Retention
One of the biggest hurdles in overcoming OUD is simply sticking with treatment long enough for new, healthy habits to take root. This is where naltrexone really shines. Staying engaged in a recovery program is one of the strongest predictors of long-term success, and the evidence shows naltrexone helps people do just that.
A major meta-analysis found that naltrexone significantly boosts the odds of someone staying in treatment compared to controls. Across all the studies included, the average retention rate was 41.0%, highlighting its power to keep people on their recovery path. You can dig into the full research about naltrexone's impact on treatment retention.
This data helps answer the question "does naltrexone work?" by showing it gives people the staying power they need to build a life free from opioids.
Navigating the Induction Phase
Starting naltrexone for OUD requires a critical first step known as the induction phase. Because naltrexone is such a powerful blocker, it can’t be started while opioids are still in a person's system. Taking it too soon would trigger precipitated withdrawal—a sudden, severe, and potentially dangerous onslaught of withdrawal symptoms.
To avoid this, a person must be completely opioid-free for 7 to 10 days before their first dose. This medically supervised detox period is non-negotiable for safety and comfort. While it can sound daunting, it’s a manageable and essential part of the process.
Here’s what this phase usually involves:
- Medically Supervised Detox: Healthcare professionals manage withdrawal symptoms with supportive care and medications, making the process as safe and comfortable as possible.
- Symptom Monitoring: The clinical team keeps a close watch to pinpoint the exact moment it's safe to administer that first dose of naltrexone.
- Support and Preparation: This time is also used to prepare the person for the next stage of recovery, including therapy and counseling.
The challenges of this initial period can sometimes be made tougher by symptoms that linger. Understanding the nature of Post-Acute Withdrawal Syndrome (PAWS) can be a game-changer for patients and families, as it explains the longer-term emotional and psychological symptoms that can follow the acute detox phase.
The induction phase is a bridge to a new kind of freedom. While it requires commitment, successfully navigating this period opens the door to a non-addictive treatment that can provide a powerful defense against relapse.
At Altura Recovery, our team provides the compassionate, expert support needed to guide individuals safely through this process. We make sure the transition onto naltrexone is handled with the utmost care, setting the stage for successful, long-term recovery. This approach—combining medication with robust therapeutic support—addresses both the physical and psychological sides of addiction, empowering people to reclaim their lives.
Oral Naltrexone vs. Injectable Vivitrol
When it comes to naltrexone, one of the first conversations we have with patients is about the delivery method: a daily pill or a once-a-month injection? Both approaches block opioid receptors, but how they fit into your real life is worlds apart. Making an informed choice between oral naltrexone and its injectable form, Vivitrol, is a critical step in building a solid recovery plan.
Oral naltrexone is a simple daily tablet. This gives you flexibility and is less invasive, but it also puts the entire burden of consistency squarely on your shoulders. In early recovery, when your motivation can swing and new routines feel fragile, remembering a pill every single day can be a monumental task. If you miss a dose, that protective shield drops, leaving you vulnerable to cravings and a potential relapse.
This daily challenge is precisely where the injectable version, Vivitrol, comes in.
The Adherence Advantage of Vivitrol
Vivitrol is an extended-release formula of naltrexone, given as one injection each month. This "one-and-done" approach takes the daily pressure of remembering a pill completely off the table. Instead of having to make the right choice 30 times a month, you just have to commit to showing up for one appointment.
This isn't just a matter of convenience; it’s a clinically proven advantage. The steady protection from a monthly shot provides a reliable safety net, which is absolutely vital during the turbulent first few months of recovery.
By maintaining a consistent level of naltrexone in your system, Vivitrol keeps that neurological barrier against cravings firmly in place without any daily effort on your part. This frees up so much mental energy that you can then pour into therapy, building new habits, and reclaiming your life.
This decision tree helps illustrate how a person’s motivation and desire for a non-agonist treatment path can lead them toward naltrexone for Opioid Use Disorder.
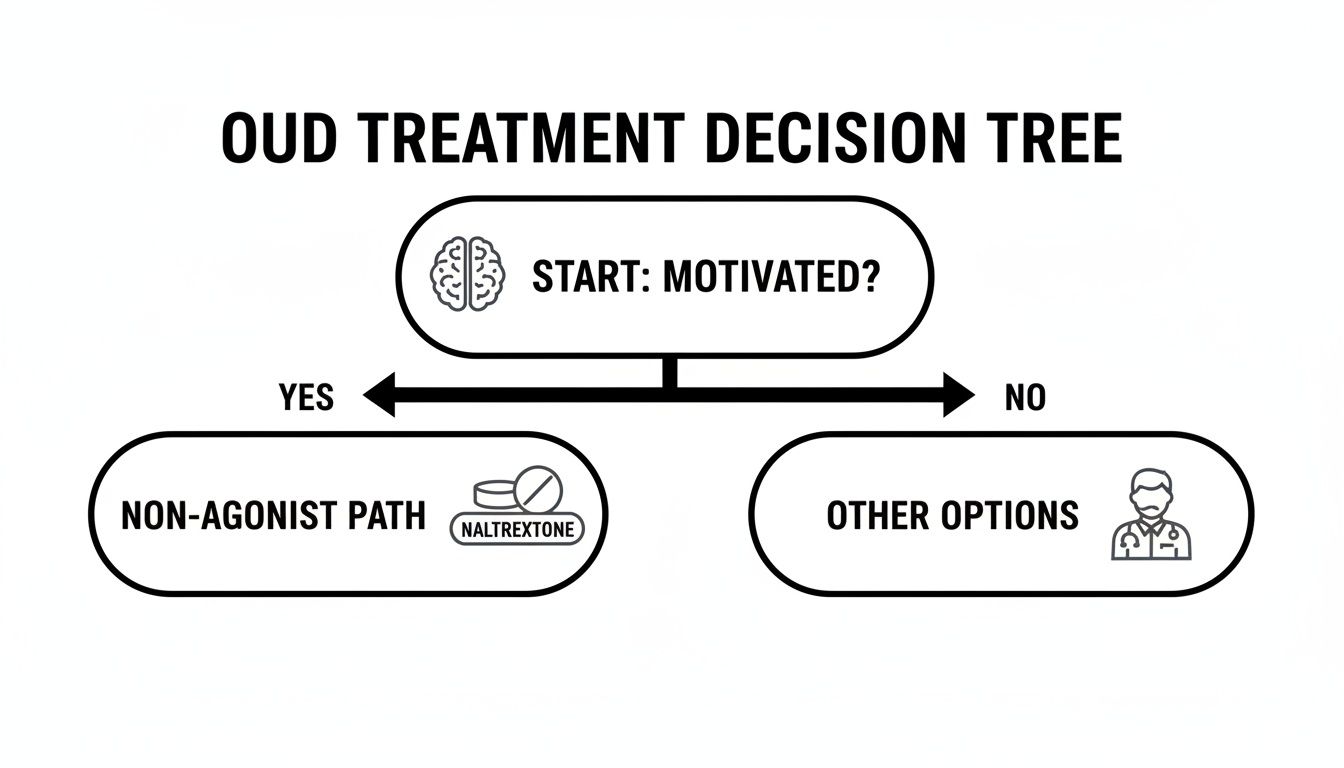
As the visual shows, for people who are motivated and want a non-addictive medication, naltrexone is a primary option to consider.
Comparing Treatment Outcomes
So, which form of naltrexone actually works better? When you look at the data on who successfully stays on their medication, the injectable version has a clear edge.
Head-to-head clinical trials have shown Vivitrol’s significant upper hand. In one study with 248 participants, those who received the monthly injection stuck with their treatment at much higher rates. The numbers are telling: 40.7% of the Vivitrol group maintained high adherence, compared to just 26.6% of those taking the daily pill. You can read more about these crucial findings on naltrexone adherence.
That statistic means people on the monthly shot are nearly twice as likely to take their medication as prescribed. That translates to a much stronger and more consistent defense against relapse when it matters most.
Making the Right Choice for You
Ultimately, the decision between oral naltrexone and Vivitrol is a personal one, made in conversation with your healthcare provider. You’ll want to weigh a few key factors.
- Lifestyle: Do you have a stable daily routine where remembering a pill is no problem? Or would a single monthly appointment be far easier to manage amidst work, family, and therapy?
- Cost and Coverage: Insurance plans can cover these two forms differently. The injection often has a higher upfront cost, so it's important to check what your plan will pay for.
- Personal Preference: Some people feel more in control taking a daily pill. Others find the freedom and peace of mind that comes with a monthly injection invaluable.
Both forms of naltrexone are powerful tools in the recovery toolbox. The most important thing is choosing the one that you can stick with consistently. By removing the daily hurdle of adherence, Vivitrol often gives people a more solid foundation to stand on while they do the real work of recovery.
Why Naltrexone Works Best with Professional Support
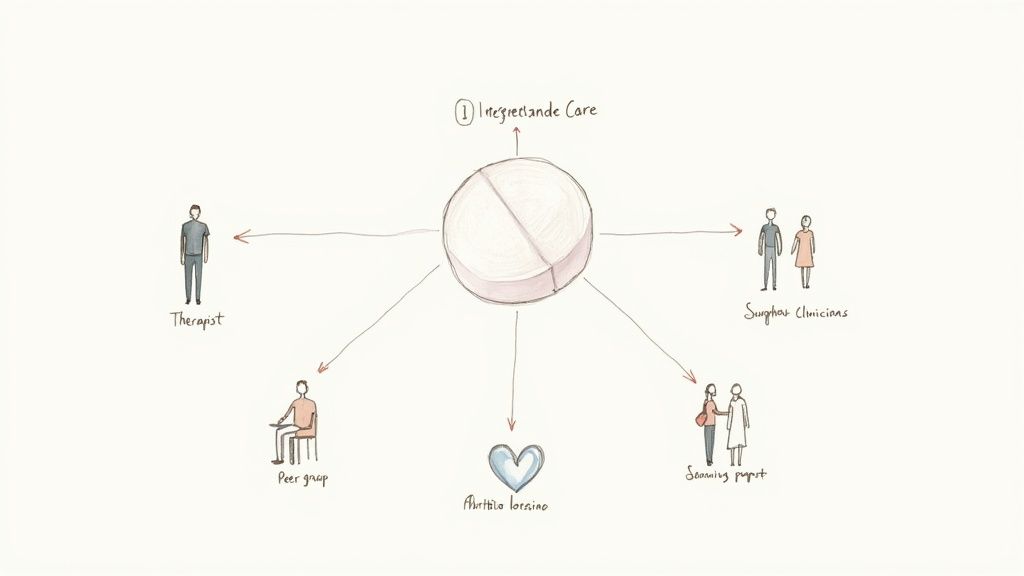
Naltrexone is a powerful tool, but it's important to be clear: it's not a standalone cure for addiction. True, lasting recovery is built on a foundation of comprehensive, integrated support. The medication is just one piece of the puzzle—a very important piece, but a piece nonetheless.
Think of naltrexone as scaffolding for a building under construction. It provides crucial stability and support, making the whole structure safer and more resilient while the real work gets done. But the scaffolding isn't the building. You still have to lay the bricks, run the wiring, and finish the interior.
This is exactly how Medication-Assisted Treatment (MAT) is designed to work. Naltrexone gives you the neurological stability to quiet the constant noise of cravings. This creates the mental and emotional space you need to dig in and do the deeper work of recovery.
The Synergy of Medication and Therapy
When your brain isn't screaming for a drink or a drug, you can finally focus. This is where behavioral therapy, counseling, and peer support become incredibly effective. They are the essential next steps that build on the foundation naltrexone provides.
Naltrexone treats the biological component of addiction, while therapy addresses the psychological and behavioral roots. Combining them ensures you are treating the whole person, not just the symptoms.
At a clinic like Altura Recovery, this integrated approach is central to helping people build a life they don't want to escape from. The goal isn't just to manage addiction but to construct a fulfilling, resilient future. This process involves several key components working together:
- Developing Healthy Coping Skills: Therapy helps you pinpoint your triggers and develop new, constructive ways to manage stress, anxiety, and tough emotions without turning to a substance.
- Addressing Root Causes: Counseling offers a safe space to explore the underlying issues that may have fueled the substance use in the first place, like trauma, depression, or family dynamics.
- Building a Support System: Group therapy and peer support connect you with others who get it. This sense of community and accountability is vital for long-term success.
Knowing what happens in counselling sessions can make starting therapy feel much less intimidating. This powerful synergy also empowers you to rebuild other areas of your life, making things like exploring self-care activities for mental health a practical and crucial part of the healing journey.
By combining medication with professional guidance, you’re not just hoping for the best—you're building a robust framework for a recovery that's designed to last.
Your Questions About Naltrexone, Answered
Starting any new medication brings up questions, and that's completely normal. Feeling informed is a huge part of feeling confident in your recovery plan. Let's walk through some of the most common concerns people have before starting naltrexone and get you some clear, practical answers.
What Are the Most Common Side Effects?
Like a lot of medications, naltrexone can have side effects, but for most people, they're on the milder side and don't last long. The most common things people report are nausea, a headache, some dizziness, or feeling tired.
Usually, these initial issues fade within the first week or two as your body gets used to the medication. It's always smart to talk to your doctor about anything that feels bothersome or sticks around, but most people find the benefits of naltrexone far outweigh these temporary discomforts.
How Long Do I Have to Be Opioid-Free Before Starting?
This one is absolutely critical for safety. If you're dealing with Opioid Use Disorder, you must be completely opioid-free for 7 to 10 days before your first dose of naltrexone. No exceptions.
Why? Starting too soon can throw your body into what's called precipitated withdrawal—a sudden, intense, and frankly miserable onset of withdrawal symptoms. This transition must be handled under medical supervision to make sure it's done safely and as comfortably as possible.
Think of naltrexone as a powerful shield. That mandatory opioid-free window ensures the shield can go up and protect you from relapse without first causing a painful reaction. It sets you up for a much smoother start.
Will Naltrexone Stop Me from Feeling Happy?
This is a big—and very understandable—concern. The short answer is no, it won't. Naltrexone is specifically designed to target and block the intense, artificial rush of euphoria that comes from substances like opioids and alcohol.
It does not get in the way of your brain’s natural reward system. You can still feel genuine joy from everyday life—laughing with friends, finishing a project, or enjoying a hobby. If you ever notice significant mood changes, that's definitely something to bring up with your healthcare provider.
Can I Get Pain Relief If I Get Injured?
Yes, but it takes some planning with your medical team. Since naltrexone blocks the effects of opioid painkillers (like morphine or Vicodin), it is vital that you tell every healthcare provider you see—from your dentist to the ER staff—that you are taking it.
There are many effective non-opioid pain management strategies available. Your doctors can easily create a safe pain relief plan that works alongside your naltrexone treatment, ensuring you get the care you need without putting your recovery at risk. For those looking into medication access, certain platforms can help you get online prescriptions from licensed providers, which could be a convenient way to manage non-opioid medications with your doctor's guidance.
At Altura Recovery, we believe answering your questions is the first step in building a recovery plan you can trust. If you're ready to see how Medication-Assisted Treatment can fit into your journey, contact us today at https://www.alturarecovery.com.