When someone is diagnosed with comorbid posttraumatic stress disorder, it’s a clinical way of saying they’re fighting a battle on two fronts. It means PTSD is happening alongside another serious mental health condition, like major depression, an anxiety disorder, or a substance use disorder. This isn't a rare exception; for those who have lived through trauma, it's practically the rule.
What Is Comorbid Posttraumatic Stress Disorder?
Think of it like this: you’re trying to mend a badly broken bone, but at the same time, you’re battling a nasty infection. The infection saps your strength, making it harder for the bone to heal properly. Meanwhile, the stress and pain from the injury weaken your immune system, letting the infection dig in deeper. One problem feeds the other, creating a cycle that can feel impossible to escape.
That analogy gets right to the heart of comorbid PTSD. The term “comorbid” just means two or more medical conditions are present in the same person at the same time. When you apply it to PTSD, you're looking at a complex picture where trauma symptoms are tangled up with the symptoms of another disorder, each one making the other worse.
Why Trauma Rarely Travels Alone
Trauma isn't a neat, contained event. It’s a seismic shock that ripples through a person’s entire nervous system, fundamentally changing how they think, feel, and perceive the world. Because its impact is so widespread, it often cracks the door open for other conditions to take hold.
For example, the constant state of high alert and fear that defines PTSD can easily bleed into a generalized anxiety disorder. The profound sense of shame, hopelessness, and isolation that follows a traumatic event shares the same DNA as major depression. The connection isn't random—it's a direct result of trauma's far-reaching consequences.
Posttraumatic stress disorder rarely exists in a vacuum. In fact, comprehensive research shows that over 90% of individuals diagnosed with PTSD have at least one other lifetime mental health diagnosis. The most common co-occurring conditions are major depressive disorder, anxiety disorders, and substance use disorders.
This staggering rate of overlap drives home a critical point: trying to treat PTSD without addressing the co-occurring depression or substance use is like setting the broken bone while letting the infection rage. You might make some progress, but a full, lasting recovery is unlikely.
Common Conditions Co-occurring with PTSD
To make sense of this overlap, it helps to see the most frequent pairings. The table below outlines common comorbid conditions and how they typically connect with PTSD.
| Co-occurring Condition | Nature of Comorbidity | Common Symptom Overlap |
|---|---|---|
| Substance Use Disorder (SUD) | Self-medication to numb intrusive thoughts, anxiety, or emotional pain from trauma. | Impulsivity, social isolation, impaired judgment, sleep disturbances. |
| Major Depressive Disorder (MDD) | Feelings of hopelessness, shame, and loss of interest are central to both conditions. | Anhedonia (loss of pleasure), negative self-view, fatigue, suicidal ideation. |
| Anxiety Disorders | Hypervigilance from PTSD fuels the worry and fear characteristic of anxiety. | Excessive worry, panic attacks, avoidance of triggers, restlessness, irritability. |
| Bipolar Disorder | Trauma can trigger or worsen manic and depressive episodes. | Mood instability, risky behaviors, sleep disruption, emotional dysregulation. |
Understanding these connections is the first step toward building a treatment plan that actually works.
Why an Integrated Approach Is Non-Negotiable
Recognizing that PTSD is often part of a larger clinical picture changes everything. It moves the focus from chasing individual symptoms to treating the whole person. This is where integrated treatment models shine, as they are designed to address all conditions at once.
By tackling the intertwined roots of trauma, depression, and addiction simultaneously, you can finally break the cycle and build a solid foundation for recovery. To see how this is done, it helps to understand what trauma-informed therapy truly entails.
When trauma takes root, it rarely stays confined to one part of a person’s life. PTSD symptoms have a way of rippling outward, creating the perfect conditions for other mental health struggles to surface. These co-occurring conditions aren't separate problems; they become deeply tangled with the trauma itself, and understanding them is the first step toward effective treatment.
Substance Use Disorder: The Self-Medication Cycle
Of all the conditions seen alongside PTSD, Substance Use Disorder (SUD) is one of the most common. There's a powerful reason for this, often explained by the "self-medication" hypothesis. In simple terms, people use drugs or alcohol to get a moment's peace from the relentless symptoms of PTSD.
Imagine being stuck in a constant state of high alert, your mind replaying the worst moments of your life without warning. For someone living with that reality, alcohol might seem like the only way to quiet the intrusive thoughts, while a pill could feel like a lifeline to finally calm a nervous system that won't shut down. The substance offers a brief, predictable escape from an internal world that feels anything but.
This coping strategy, while completely understandable, quickly spirals into a destructive cycle. The temporary relief comes at a steep price. Once the substance wears off, the PTSD symptoms often roar back, sometimes even stronger than before, which only intensifies the urge to use again.
This creates a vicious feedback loop:
- PTSD symptoms ignite: A trigger—a loud noise, a specific smell—causes a flashback and overwhelming distress.
- Substances provide an escape: The person turns to their substance of choice to numb the anxiety and pain.
- Consequences pile up: The substance use leads to arguments, missed work, and health problems.
- Symptoms get worse: The hangover, withdrawal, or shame from using only adds fuel to the fire, making the original PTSD symptoms feel even more unmanageable.
This cycle is precisely why treating PTSD and SUD at the same time is non-negotiable for lasting recovery. Breaking free means addressing the deep connection between mental health and substance abuse head-on.
Major Depression: When Hopelessness Takes Hold
It's also incredibly common for Major Depressive Disorder (MDD) to develop in the shadow of PTSD. The two conditions share so much common ground—isolation, loss of interest, negative self-talk—that they can feel like one seamless experience of suffering.
Think about a survivor of a serious accident who now avoids friends and family. The hobbies that once brought them joy now feel pointless, and they're weighed down by a profound sense of being "broken" or "damaged." These feelings of hopelessness, numbness, and shame are classic signs of both PTSD and depression.
The emotional detachment that helps a person survive trauma can easily curdle into the pervasive emptiness of depression. The belief that the trauma has permanently changed you for the worse is the very thought pattern that fuels a depressive episode.
Anxiety Disorders: When Hypervigilance Runs Wild
Given that PTSD is itself a trauma- and stressor-related disorder, it’s no surprise that other anxiety disorders frequently show up, too. The constant state of being "on guard" that defines post-traumatic stress is the perfect breeding ground for persistent, widespread fear.
Here’s how that can play out:
- Generalized Anxiety Disorder (GAD): The hypervigilance of PTSD—always scanning the environment for threats—can bleed into everyday life, morphing into the chronic, free-floating worry of GAD. Suddenly, it’s not just about avoiding trauma reminders; it's about catastrophizing every work email, financial decision, and family matter.
- Panic Disorder: A combat veteran with PTSD might have an intense flashback while in a crowded mall. The sudden, terrifying physical sensations—a racing heart, shortness of breath, a feeling of dying—are so frightening that they begin to fear the panic attack itself. This "fear of the fear" is the hallmark of panic disorder.
In every case, the nervous system dysregulation caused by trauma provides the fuel for the co-occurring condition. Trying to treat just one part of the problem while ignoring the other is like trying to bail out a boat without plugging the hole. A truly effective approach has to address the entire picture of what a person is going through.
How Comorbidity Complicates PTSD Symptoms and Recovery
When PTSD shows up with another condition, they don’t just sit next to each other quietly. They interact, feeding off one another and creating a cycle that can feel impossible to break on your own.
Imagine trying to untangle a knot made of two different kinds of rope—one rough, one smooth. Every time you pull on one, it just tightens the other, making the whole mess worse. This is what it’s like living with comorbid posttraumatic stress disorder.
The two conditions often share symptoms, and one can easily pour gasoline on the other’s fire. For example, the bone-deep exhaustion and lack of motivation from depression can make the hard work of trauma therapy feel like climbing a mountain. Just getting to an appointment can seem overwhelming, let alone digging into painful memories.
It works the other way, too. Substance use often starts as a way to numb the razor-sharp edges of PTSD symptoms like hypervigilance or intrusive thoughts. While it might bring a moment of relief, it actively blocks the emotional processing needed to actually heal. By numbing the pain, you also numb your ability to recover from it, putting a massive roadblock in the way of getting better.
The Amplification Effect of Co-occurring Conditions
Having a second disorder doesn't just add to the weight; it multiplies it. This dynamic, what clinicians call the amplification effect, means the combined impact is far greater than the sum of its parts. Each condition makes the other worse in a vicious, self-sustaining loop.
Think about these real-world scenarios:
- Depression and PTSD: The hopelessness that comes with depression can cement the traumatic belief that you’re permanently broken or that the world is fundamentally unsafe. This deepens the trauma response, which in turn leads to more isolation and even worse depression.
- Anxiety and PTSD: The constant on-edge feeling of PTSD hyperarousal is fuel for the relentless worry of generalized anxiety disorder. A person might become so terrified of a trauma reminder triggering a panic attack that they develop a full-blown panic disorder on top of everything else.
- Substance Use and PTSD: Using drugs or alcohol to cope often leads to more impulsivity and risk-taking—behaviors already common in PTSD. This can tragically lead to new traumatic events or compound the consequences of the original trauma.
The diagram below shows how some of the most common conditions get tangled up with PTSD.
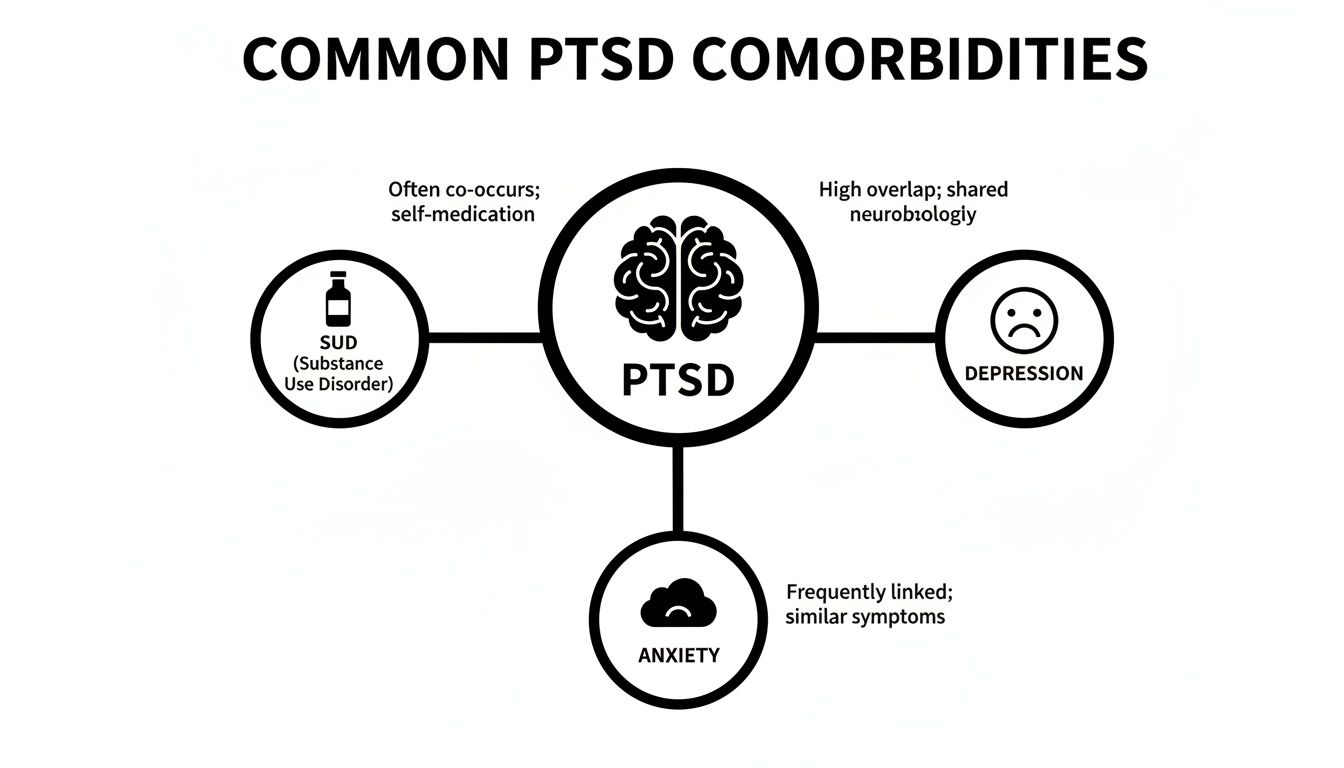
This visual makes it clear: Substance Use Disorder, Depression, and Anxiety aren't just separate problems. They're deeply woven into the core experience of living with post-traumatic stress.
Increased Risks and the Need for Integrated Care
This complicated interplay dramatically raises the risk for severe outcomes. The sheer weight of battling two serious conditions at once can feel crushing, leading to a much deeper sense of despair than either one would cause alone.
Addressing only one piece of the puzzle often leads to frustration and relapse. For example, if you treat the substance use without addressing the underlying trauma that drives it, the person is left without healthy coping skills when PTSD symptoms inevitably flare up.
This is exactly why a comprehensive, integrated approach isn’t just a good idea—it’s non-negotiable for real, lasting recovery.
The link between comorbidity and risk isn't just a theory; it's backed by some stark numbers. Epidemiological studies have shown that having comorbid conditions dramatically increases the risk of the worst outcomes, including suicide attempts. For instance, one study found that individuals with both PTSD and a substance use disorder were nearly three times more likely to reattempt suicide within six months of an initial attempt. You can dig into the research on comorbid PTSD and suicide risk to better understand the urgency.
This highlights the absolute necessity of a treatment plan that sees the whole person and tackles all interconnected issues at the same time.
Navigating Diagnosis and Integrated Treatment Plans
Getting the right diagnosis is the essential first step toward healing from comorbid posttraumatic stress disorder. A solid assessment goes way beyond a simple PTSD checklist; it’s a comprehensive evaluation designed to see the full, interconnected picture of what’s going on. A skilled clinician will ask detailed questions not just about the trauma itself, but about your mood, any substance use, anxiety levels, and how you’re managing day-to-day.
Think of it like a home inspector checking the foundation, plumbing, and electrical systems all at once. They know a problem in one area—like leaky pipes—can wreak havoc on another, like the wiring. In the same way, a clinician needs to understand how depression might be making PTSD avoidance worse, or how drinking is secretly fueling hypervigilance.
The Importance of a Comprehensive Evaluation
This deep dive is critical because comorbid conditions can easily mask or mimic each other. The irritability from PTSD can look a lot like the agitation from an anxiety disorder. The emotional numbness of trauma might be mistaken for the flat affect of major depression. A surface-level diagnosis could easily miss these overlaps, leading to a treatment plan that only tackles half the problem.
This is especially true when you realize that having one condition can dramatically increase the risk for another. For example, research shows that people with major depressive disorder have more than a sevenfold increased risk of developing PTSD after a traumatic event compared to those without it. This finding really drives home how pre-existing conditions create vulnerabilities, making an integrated diagnostic approach an absolute must. You can read the full research about these psychiatric illness findings to see the data for yourself.
A proper assessment will almost always involve:
- Structured Clinical Interviews: Using standardized, evidence-based tools to carefully evaluate symptoms for PTSD, depression, anxiety, and SUDs.
- A Detailed Personal History: Exploring your personal story with trauma, mental health, substance use, and family dynamics to see how all the pieces fit together.
- Screening Tools: Specific questionnaires that help quantify how severe symptoms are and give a baseline to track progress over time.
This thorough process makes sure that the treatment plan that follows is built on a solid, accurate foundation.
Creating an Integrated Treatment Plan
Once a clear, comprehensive diagnosis is in place, the focus shifts to creating an integrated treatment plan. This is the modern gold standard for treating comorbid posttraumatic stress disorder, and for very good reason. It moves completely away from the old, ineffective method of treating things one by one—like telling someone to "get sober first, and then we’ll deal with the trauma." We now know that approach rarely works.
An integrated plan treats all diagnosed conditions at the same time, in the same place, with a cohesive clinical team. It’s built on the understanding that the symptoms are tangled together. Trying to fix one without addressing the others is like trying to repair the leaky plumbing while ignoring the faulty wiring that keeps causing the short circuits.
This concurrent approach is the bedrock of effective, lasting recovery. By getting to the root trauma that may be driving the substance use, and at the same time addressing the depressive symptoms that drain motivation for therapy, an integrated plan can finally break that frustrating cycle. It gives you the skills to manage all your symptoms at once, building a much stronger foundation for a healthy future. You can learn more about how this works by exploring our guide on integrated treatment for dual diagnosis.
Evidence-Based Therapies for Comorbid PTSD
Starting treatment for comorbid PTSD can feel overwhelming, but a handful of proven, evidence-based therapies offer clear, structured paths toward healing. The goal isn’t to erase painful memories. Instead, these approaches help you change your relationship with them, dialing down their emotional volume and giving you new skills to manage both the trauma and any co-occurring conditions at the same time.
Think of it like this: if a traumatic memory is a deeply rutted, muddy road you’re forced to drive down every day, therapy helps you pave it. The road is still there, but it becomes smoother and easier to travel, letting you get where you’re going without constantly getting stuck.
Eye Movement Desensitization and Reprocessing (EMDR)
One of the most powerful trauma-focused therapies available is Eye Movement Desensitization and Reprocessing (EMDR). It’s a highly structured therapy designed to help the brain reprocess traumatic memories, moving them from "active crisis" storage to a more settled, historical file.
During an EMDR session, a therapist guides you to briefly focus on a distressing memory while engaging in bilateral stimulation—often by following their fingers back and forth with your eyes. This dual-attention process helps “unstick” the memory from its raw, emotional state. It’s like helping your brain’s natural information processing system finally file away a chaotic pile of papers into the right cabinet. The memory stops feeling like it's happening right now and becomes a part of your past you can recall without being overwhelmed.
EMDR has a strong track record. Studies have shown that up to 73.1% of participants no longer met the criteria for PTSD after completing treatment. You can get a much deeper look into how it works by reading our detailed guide on what EMDR therapy is.
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
Another cornerstone of treatment is Trauma-Focused Cognitive Behavioral Therapy (TF-CBT). This therapy is built on the core principle that our thoughts, feelings, and behaviors are all connected. Trauma often leaves behind powerful, negative thought patterns—like "I'm not safe" or "It was all my fault"—that act as fuel for feelings of fear, shame, and hopelessness.
TF-CBT gets right to work challenging these harmful beliefs. With a therapist's guidance, you learn to spot these automatic negative thoughts and examine the actual evidence for and against them. Over time, this helps you reframe them into more balanced and realistic perspectives, effectively dismantling the cognitive engine that powers both PTSD and conditions like depression.
Dialectical Behavior Therapy (DBT)
For many people with comorbid posttraumatic stress disorder, the daily struggle is with emotional dysregulation—feeling like your emotions are constantly hijacking your life. This is where Dialectical Behavior Therapy (DBT) comes in. While it’s not strictly a trauma-processing therapy, DBT provides the exact skills needed to manage the intense emotions that come with PTSD and co-occurring disorders like substance use.
DBT is organized around four key skill sets:
- Mindfulness: Learning to stay grounded in the present moment without judgment.
- Distress Tolerance: Finding healthy ways to get through painful emotions without making things worse (like turning to alcohol or drugs).
- Emotion Regulation: Understanding your emotions and learning how to influence them.
- Interpersonal Effectiveness: Building skills to communicate your needs and maintain healthy relationships.
These skills create the stability required to safely do the deeper work of processing trauma.
By building a solid foundation of emotional regulation and coping skills, therapies like DBT empower individuals to handle the difficult work of trauma processing without becoming destabilized. It’s about building the container before you pour in the challenging content.
To help clarify how these therapies differ in their approach, let's compare them side-by-side.
Comparing Therapeutic Approaches for Comorbid PTSD
| Therapy | Primary Focus | Key Techniques |
|---|---|---|
| EMDR | Reprocessing traumatic memories to reduce their emotional charge and intrusiveness. | Bilateral stimulation (eye movements, tapping), guided memory recall, cognitive restructuring. |
| Trauma-Focused CBT | Identifying and challenging negative thought patterns and beliefs related to trauma. | Psychoeducation, cognitive processing, exposure therapy, relaxation techniques. |
| DBT | Building skills to manage intense emotions, tolerate distress, and improve relationships. | Mindfulness exercises, distress tolerance skills, emotion regulation strategies, interpersonal effectiveness. |
Each of these therapies offers a unique but complementary set of tools. The best approach often integrates elements from each, tailored to an individual’s specific symptoms and goals.
Medication Management and Group Therapy
In a comprehensive treatment plan, medication can be a critical support pillar. Antidepressants like SSRIs can help take the edge off severe depressive and anxious symptoms, which often makes it easier to show up and engage fully in therapy. Other medications might be used to specifically target nightmares or hypervigilance. Medication isn't a cure-all, but it can provide the lift needed for therapy to truly take root.
Finally, never underestimate the power of trauma-informed group therapy. It provides something individual therapy can’t: community. Sharing your experiences with others who just get it creates a profound sense of connection and validation, which is a powerful antidote to the isolation that so often comes with PTSD. It’s a safe place to practice new coping skills and realize you are not in this alone.
For anyone seeking structured, proven approaches, exploring relevant clinical practice guidelines can offer valuable insight into the standards of evidence-based care.
Building a Life in Long-Term Recovery
Making it through a treatment program for comorbid PTSD is a huge win. But it’s the start of the marathon, not the finish line. The next phase is all about building a life where recovery isn't a temporary project, but a sustainable reality. It’s where you take all the skills you learned in therapy and weave them into your everyday habits.
This is where continuing care comes in. Think of it as a bridge between the intensive, structured world of treatment and the full independence of daily life. These programs are designed to meet you exactly where you are.
- Partial Hospitalization Programs (PHP) offer the highest level of outpatient support. You’ll typically spend several hours a day, five days a week, in therapy and psychiatric care, but you get to sleep in your own bed at night.
- Intensive Outpatient Programs (IOP) are a step down in time commitment, making them a great fit for people balancing recovery with a job, school, or family life.
- Supportive Outpatient Programs (SOP) provide the most flexibility, usually involving weekly check-ins to help you maintain momentum and navigate any new challenges that pop up.
Creating a Practical Relapse Prevention Plan
A solid relapse prevention plan is the bedrock of long-term recovery. This isn't just a document you create and forget; it's your personal roadmap for handling life’s stressors without resorting to old, destructive coping patterns. A good plan starts with unflinching self-awareness.
First, you have to identify your personal triggers. These can be external—a specific place, a certain person, even a time of year—or internal, like feelings of loneliness, anger, or pure exhaustion. Knowing what makes you vulnerable is the first step toward defusing those risks.
Next, it’s critical to build a reliable support network. This network should include sober friends, family you can trust, your therapist, and maybe a support group like AA, NA, or SMART Recovery. These are the people you call before a crisis feels like it’s swallowing you whole.
Long-term recovery isn't about being perfect; it's about being prepared. It involves creating a life where healthy coping skills are more accessible and rewarding than old patterns of self-medication or avoidance.
Finally, you have to actively apply healthy coping skills until they become second nature. This means actually practicing mindfulness when anxiety spikes, using your communication skills to hold a boundary, or going for a run to burn off stress. It also helps to understand the physical side of things; learning strategies to naturally reduce cortisol levels can be a game-changer for keeping your body’s stress response in check.
Family members are a huge part of this equation. When they join family therapy sessions and learn about both PTSD and addiction, they can become powerful allies. They learn how to offer real support instead of accidentally enabling old behaviors. With a strong plan and a supportive team, building a resilient, fulfilling life after treatment isn't just a hopeful idea—it’s entirely possible.
Questions We Hear All the Time About Comorbid PTSD
When you’re staring down the complexities of co-occurring PTSD and addiction, a flood of questions is completely normal. We’ve been there with countless individuals and families, and we’ve found that a few key concerns come up again and again. Here are some straight answers to help clear things up.
"Do We Treat the PTSD or the Addiction First?"
This is probably the most critical question people ask, and thankfully, years of clinical experience have given us a very clear answer: you have to treat them both at the same time.
The old-school approach was to treat one problem first—usually telling someone to "get sober, then we'll deal with the trauma." We now know this is a recipe for failure. Why? Because the two conditions are tangled up in a vicious cycle. For so many, using substances is a desperate attempt to numb the flashbacks, anxiety, and nightmares of PTSD. On the flip side, those exact same trauma symptoms are massive triggers for relapse.
An integrated treatment model tackles this head-on. It's about learning healthier ways to cope with trauma while simultaneously building the skills for sobriety. You break the feedback loop that keeps people stuck.
"Can't We Just Use Medication to Fix It?"
While medication can be an absolute game-changer, it’s not a standalone cure. It's better to think of it as a powerful tool that creates the stability needed for the real healing work to begin.
Medications like SSRIs can turn down the volume on overwhelming depression and anxiety, making daily life feel manageable again. That relief is often what makes it possible for someone to show up and fully engage in therapy.
But medication alone doesn't process the root causes of trauma. That's where therapies like EMDR, CBT, and DBT come in. These are the tools that help you build long-term coping skills, manage symptoms without substances, and build genuine resilience. The most effective approach almost always combines smart medication management with consistent, trauma-focused therapy.
"How Can I Support My Loved One Without Enabling Them?"
This is the tightrope walk every family member faces: balancing compassion with healthy boundaries. Your support is vital, but enabling behaviors—even when well-intentioned—can get in the way of their recovery.
Here are a few practical steps you can take:
- Offer Real Support, Not Rescue. Let them know you love them and that you believe in their ability to get through treatment. A great way to do this is by showing up for family therapy sessions—it shows you're in it with them.
- Draw Clear Lines. Making excuses for their behavior or shielding them from the natural consequences of their choices doesn't help. This means being firm about boundaries, like not providing money that could go toward substances.
- Get Educated. The more you learn about PTSD and addiction, the better you'll understand what they're up against. This knowledge helps you respond in ways that are genuinely helpful, not just accommodating.
And remember, you need support, too. Your well-being is not optional. Groups like Al-Anon offer a community of people who truly get what you’re going through and can be an incredible source of strength.
At Altura Recovery, we specialize in guiding individuals through the complexities of comorbid disorders with compassionate, evidence-based care. Our integrated outpatient programs are designed to help you or your loved one build a foundation for lasting recovery while maintaining daily responsibilities. Find out more about our approach at https://www.alturarecovery.com.