You’ve made it through detox. The worst of the physical storm has passed, and it feels like you should be on solid ground. But for many, what comes next is a more subtle, and often more confusing, challenge. This next phase of the journey is called post-acute withdrawal syndrome, or PAWS.
It’s the unseen hurdle in long-term recovery, affecting a huge number of people who have recently stopped using substances. While acute withdrawal is the intense, largely physical process that wraps up in a few days or weeks, PAWS is a collection of psychological and emotional symptoms that can stick around, fluctuating for months or even longer.
Think of your brain and nervous system like a forest recovering from a wildfire. The immediate danger—the fire of acute withdrawal—is out. But the landscape is still fragile. PAWS is the slow, unpredictable process of regrowth. Some days are sunny and clear, while others bring sudden storms of anxiety, brain fog, or low moods as the ecosystem recalibrates itself. It’s not a straight line to recovery; it’s a natural, winding path of healing.
Who Does PAWS Affect?
This isn't a sign of weakness or a signal that you're about to relapse. PAWS is a very real, physiological process. Whether you experience it, and how intensely, often comes down to a few key factors:
- The Substance You Used: Different drugs rewire the brain in different ways. PAWS is especially common after quitting alcohol, opioids, and benzodiazepines. In fact, some studies show up to 90% of opioid users and 75% of people recovering from alcohol use disorder will face some PAWS symptoms.
- How Long and How Much You Used: The more the brain had to adapt to a substance, the longer it will take to find its balance again. A longer or heavier pattern of use often means a more pronounced PAWS experience.
- Your Overall Health: Things like co-occurring mental health conditions (like anxiety or depression), your physical health, and how much stress you're under can all influence the severity and duration of PAWS.
Understanding PAWS is a game-changer because it gives your experience a name. It confirms that the lingering mood swings, the trouble concentrating, and the waves of anxiety aren't just in your head—they are tangible signs of a brain that is actively healing.
Recognizing these symptoms for what they are—a temporary but normal part of recovery—is the first step toward getting through it. This isn't a life sentence. It’s a predictable and manageable phase. By learning to spot the signs and arming yourself with the right coping skills, you can navigate this period without letting it knock you off course.
Navigating PAWS Symptoms and Timelines
So, you’ve made it through the intense physical storm of acute withdrawal. That’s a massive accomplishment. But now, you might be dealing with a whole new set of confusing and frustrating feelings that come and go without warning. This is Post-Acute Withdrawal Syndrome, or PAWS, and it’s a very real—and very normal—part of the brain’s healing journey.
Unlike the initial detox phase, PAWS symptoms are less about the body and more about the mind. They don’t follow a straight line. Instead, they often roll in like waves, making some days feel fantastic while others feel like a huge step backward. One week, you might feel sharp and emotionally steady, only to get hit with a fog of anxiety or exhaustion the next.
This up-and-down pattern is the signature of PAWS. It’s a direct sign that your brain is working hard to recalibrate its chemistry after a long period of substance use. It's not a sign of failure; it's a sign of healing in progress.
As this visual shows, the symptoms you’re feeling aren't just in your head. They are rooted in the deep neurological repairs happening behind the scenes.
Common Symptoms You Might Experience
The challenges of PAWS tend to fall into a few key categories. While everyone’s experience is unique, many people report a similar cluster of symptoms as their brain finds its new normal. This isn’t a rare phenomenon—research shows that about 90% of people recovering from opioids and 75% from alcohol experience these lingering symptoms long after detox ends. Learn more about how long post-acute withdrawal can last.
Here’s what you might notice:
- Emotional Rollercoasters: Sudden mood swings, irritability, anxiety, or depressive feelings that seem to appear out of nowhere.
- Cognitive Fog: Difficulty concentrating, remembering things, or thinking through problems. Many people simply call it “brain fog.”
- Sleep Problems: Insomnia is incredibly common, as are vivid or disturbing dreams and a generally chaotic sleep schedule.
- Deep Fatigue: A persistent, bone-deep exhaustion that sleep doesn’t seem to fix.
- Anhedonia: This is a clinical term for the inability to feel pleasure from activities you used to love, which can be deeply discouraging.
- Heightened Stress Response: You might find yourself easily overwhelmed by situations you used to handle without a problem.
It’s critical to understand that these symptoms have nothing to do with your willpower or how committed you are to recovery. They are physiological signs that your brain is healing. The best thing you can do is treat them—and yourself—with patience and compassion.
To help you identify patterns in your own experience, this table compares some of the most frequently reported PAWS symptoms across common substances.
Common PAWS Symptoms Across Different Substances
| Symptom Category | Alcohol | Opioids | Benzodiazepines | Antidepressants |
|---|---|---|---|---|
| Emotional | Anxiety, irritability, mood swings | Depression, apathy, anhedonia | Rebound anxiety, panic attacks | Emotional blunting, mood swings |
| Cognitive | Brain fog, memory issues | Trouble concentrating, apathy | Severe brain fog, memory loss | "Brain zaps," difficulty focusing |
| Sleep | Insomnia, vivid dreams | Insomnia, restless legs syndrome | Severe insomnia, nightmares | Disturbed sleep, vivid dreams |
| Physical | Fatigue, low energy | Fatigue, muscle aches | Muscle tension, tremors | Fatigue, dizziness, nausea |
While symptoms often overlap, recognizing these substance-specific tendencies can normalize what you’re feeling and reinforce that you're not alone in this.
Understanding the PAWS Timeline
Naturally, the big question is, "How long will this last?" There’s no simple answer, because the timeline is different for everyone. The most important thing to remember is that PAWS is temporary. It is a phase, not a permanent state. How long that phase lasts depends on how much healing your brain needs to do.
For most, PAWS symptoms are at their peak for the first few months of sobriety and then begin to fade, becoming less frequent and less intense over time. The entire process can last anywhere from several months up to a couple of years.
Several key factors shape your personal timeline:
- The Substance Itself: Different drugs affect brain chemistry in different ways. Withdrawal from benzodiazepines, for instance, often involves a longer and more complex PAWS journey compared to stimulants.
- History of Use: A longer period of heavy, frequent use generally means the brain needs more time to restore its natural balance.
- Your Individual Health: Your overall physical health, genetic predispositions, and any co-occurring mental health conditions (like anxiety or depression) can influence the severity and duration of PAWS.
- Your Support System: Having strong, professional support and healthy coping skills makes a huge difference. Good support can help you manage symptoms more effectively and may even shorten the overall timeline.
Knowing that this process, while variable, is finite can be a powerful source of hope. Every wave of symptoms you successfully navigate is another milestone in your brain’s journey back to stability.
The Science Behind Why PAWS Happens
Understanding what’s happening inside your brain during post-acute withdrawal can feel incredibly liberating. It reframes the whole experience, shifting it from a personal failing to a predictable, physiological healing process. This isn’t about a lack of willpower; it’s about your brain working hard to repair itself.
Think of your brain's delicate chemical balance like a finely tuned orchestra. Each neurotransmitter—like dopamine for pleasure and GABA for calm—plays its part perfectly. When a substance is introduced, it's like a rogue conductor forcing one section to play deafeningly loud while others go quiet.
When you stop using, that conductor suddenly vanishes. The orchestra is left in chaos, struggling to find its rhythm again. This is neuroadaptation—the process where your brain physically changed to accommodate the substance. Now, it’s left with a system built to rely on something that’s gone.
The Brain’s Quest for Balance
Your body’s number one job is to maintain homeostasis, or a state of steady internal balance. The disruptive symptoms of PAWS are a direct result of your brain's slow, and sometimes clumsy, attempt to restore that natural equilibrium. It has to completely relearn how to produce and regulate its own chemicals without outside help.
This is a monumental task that simply takes time. Here’s a peek at what’s going on behind the scenes:
- Neurotransmitter Rebalancing: The brain must recalibrate its own chemical production. After long-term alcohol use, for example, the brain’s calming GABA system gets suppressed. In early recovery, it scrambles to produce enough on its own, leading to intense anxiety and restlessness.
- Receptor Repair: Chronic substance use can damage or down-regulate the number of receptors that neurotransmitters dock with. During PAWS, the brain is slowly repairing these "docking stations," which can cause symptoms like brain fog and an inability to feel pleasure (anhedonia).
- Stress System Dysregulation: Your central nervous system becomes incredibly sensitive. The "fight-or-flight" response, which should be reserved for genuine threats, can get triggered by minor daily hassles. This explains the hair-trigger irritability, anxiety, and sleep problems so common in PAWS.
The unease, fogginess, and emotional ups and downs aren't random. They are the tangible proof that your brain is working tirelessly to rebuild its internal factory and repair its communication lines. The symptoms are just the side effects of this intensive reconstruction project.
From Chaos to Calm: A Healing Process
Picture the brain’s recovery as a major construction site. Some days, the crew makes smooth, quiet progress, and you feel great. Other days, a massive rewiring project causes disruptions across the whole system, triggering a wave of symptoms. This explains the roller-coaster nature of post-acute withdrawal syndrome.
Grasping this biological reality is a game-changer. It helps you depersonalize the entire experience. Instead of thinking, "What’s wrong with me?" you can recognize a bad day for what it is: "My dopamine system is recalibrating today."
This simple shift in perspective can transform the journey. It's no longer a battle against yourself, but a partnership with your healing brain. You become an active participant in your own recovery, giving your brain the support—like good nutrition, rest, and therapy—it needs to get the job done.
Professional Support for Managing PAWS
Trying to get through post-acute withdrawal on your own is like navigating a storm without a compass. One minute the seas are calm, the next you’re hit by a wave of anxiety or brain fog. This is where getting professional support becomes less of a nice-to-have and more of a necessity. Clinical strategies give you the structure, tools, and medical oversight needed to manage this unpredictable phase and stay the course.
With trained professionals, you get a roadmap. Instead of just reacting to every symptom that pops up, you learn to see them coming, understand why they’re happening, and use proven techniques to keep moving forward. This support system is the anchor that keeps you steady when the emotional waters get rough.
The Role of Evidence-Based Therapies
Therapy is the bedrock of managing PAWS because it directly tackles the psychological chaos of this period. Two approaches, in particular, are incredibly effective at helping you rebuild emotional control and resilience.
- Cognitive Behavioral Therapy (CBT): This therapy helps you catch and reframe the negative, automatic thoughts that PAWS loves to generate. For instance, when brain fog hits and you think, "I'll never be sharp again," CBT teaches you to challenge that thought with something more realistic, like, "This is a temporary symptom of my brain healing, and it will pass."
- Dialectical Behavior Therapy (DBT): DBT is a game-changer for handling the intense mood swings and stress sensitivity that define PAWS. It gives you practical skills in mindfulness, distress tolerance, and emotional regulation so you can navigate a surge of anxiety or irritability without falling back on old, destructive coping habits.
These aren't just "talk therapies." They give you a real, tangible toolkit for changing how you respond to the very real symptoms of post-acute withdrawal.
Think of therapy as learning a new language to communicate with your healing brain. It helps you understand what its signals of distress mean and gives you the right vocabulary—coping skills—to respond constructively.
Medication Management for Symptom Relief
While there isn't a single pill that "cures" PAWS, certain non-addictive medications can offer serious relief from specific, debilitating symptoms. The goal isn't to replace one substance with another; it's about using targeted medical support to create enough stability so you can actually do the work in therapy and in your life. Working closely with a doctor is key here.
Commonly addressed symptoms include:
- Insomnia: Medications like Trazodone or Hydroxyzine can help reset your sleep cycle, which is absolutely critical for brain repair and emotional balance.
- Anxiety and Depression: A doctor might prescribe non-addictive antidepressants or anti-anxiety meds to help rebalance neurotransmitter levels, easing the relentless low moods or agitation PAWS can bring on.
- Cravings: Some medications can dial down the intensity of cravings, freeing up mental energy to focus on building new, healthier routines.
The whole point of medication management is to quiet the loudest, most disruptive symptoms, clearing the way for you to focus on the deeper work of recovery. This integrated approach creates a much stronger foundation for long-term success. The long-lasting and draining nature of PAWS is even seen in antidepressant withdrawal, where symptoms like anxiety and depression can last, on average, for about 3 years. One study analyzing 69 cases found that 81% of individuals experienced affective symptoms, while 75% reported somatic issues like headaches and muscle aches after stopping their medication. You can explore the full study on antidepressant withdrawal to learn more about these findings.
Structured Support from Outpatient Programs
The jump from an inpatient facility back to the realities of daily life is one of the most vulnerable times in anyone's recovery. This is the gap that outpatient programs—like a Partial Hospitalization Program (PHP) or an Intensive Outpatient Program (IOP)—are designed to bridge. At Altura Recovery, these programs provide the consistency, community, and skill-building you need to get through post-acute withdrawal successfully.
These structured settings offer a powerful combination of support:
- Consistency: Regular therapy sessions and check-ins create a predictable routine that helps calm a nervous system that's all over the place.
- Community: In group therapy, you connect with people who know exactly what you’re feeling, which cuts through the isolation that often comes with PAWS.
- Accountability: A supportive clinical team helps you stick to your recovery goals, especially on the days when you feel like giving up.
Outpatient care acts as a safety net. It ensures you have immediate access to professional guidance while you practice using your new coping skills in the real world, turning the challenges of PAWS into opportunities for lasting growth.
Building Your Daily PAWS Management Toolkit
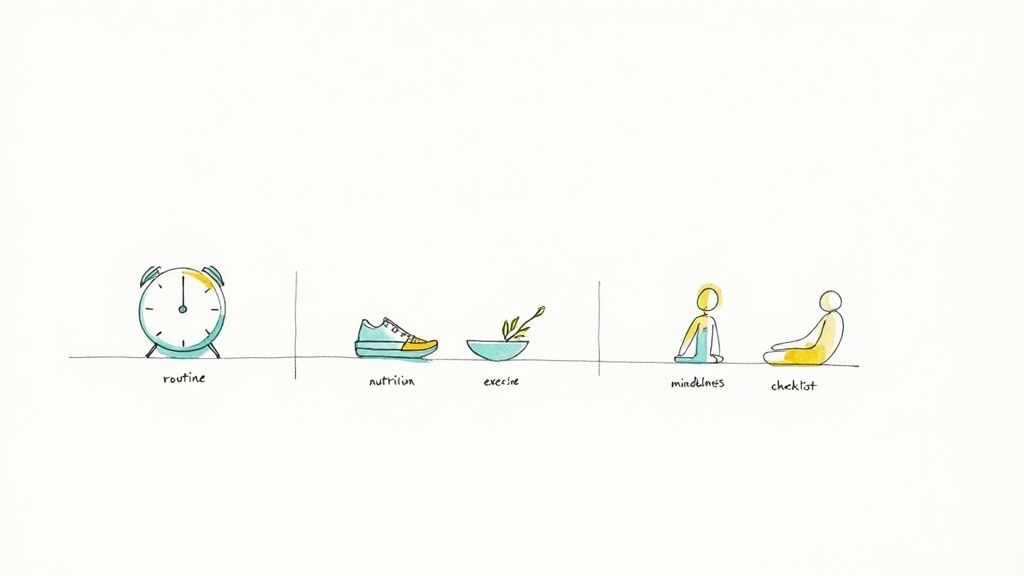
While professional support builds the foundation for recovery, your daily habits are the tools you use to actively manage the ups and downs of PAWS. Think of it as assembling a personal toolkit—a collection of simple, actionable strategies that empower you to navigate symptom waves and support your brain's healing process.
These aren't complicated fixes. They're small, consistent actions that create stability during a period of internal chaos. By focusing on these lifestyle adjustments, you start to take back a sense of control and become an active partner in your own neurological repair.
Create Stability with a Consistent Routine
During PAWS, your internal clock is often completely out of whack, which can crank up feelings of anxiety and disorientation. A predictable daily routine acts as an external regulator, giving your brain the structure it’s currently missing. It’s like giving a rudder to a ship in a storm.
This doesn’t have to be rigid or military-style, but it does need to be consistent. The goal is to cut down on decision fatigue and create a powerful sense of safety.
- Wake and Sleep at the Same Times: This is probably the single most powerful thing you can do to support your circadian rhythm, which is crucial for regulating your mood, energy, and sleep.
- Schedule Your Meals: Eating at regular intervals helps stabilize blood sugar and energy levels, preventing the sharp crashes that can easily trigger mood swings.
- Block Out Time for Self-Care: Whether it's 15 minutes of quiet reading or a walk after dinner, schedule it. Treat it like you would any other important appointment.
This consistency sends a clear signal to your nervous system that it's safe, helping to lower the constant, low-grade stress that often comes with PAWS.
Fuel Your Brain with Smart Nutrition
Your brain is working overtime to rebuild its chemical pathways, and it needs the right raw materials to get the job done. Nutrition isn't just about physical health in recovery; it's about providing the essential building blocks for neurotransmitters like serotonin and dopamine.
Think of it like supplying a construction site with high-quality bricks and mortar instead of flimsy, cheap materials.
Your diet can either help or hinder your brain’s healing process. Simple nutritional choices are one of the most direct ways you can support your recovery from post acute withdrawal syndrome every single day.
Focus on bringing in whole, nutrient-dense foods:
- Complex Carbohydrates: Foods like oats, brown rice, and quinoa deliver a steady supply of glucose, which is the brain’s main fuel source.
- Lean Proteins: Turkey, chicken, beans, and lentils are packed with the amino acids needed to produce those key neurotransmitters.
- Healthy Fats:Omega-3 fatty acids, found in fish, walnuts, and flaxseeds, are vital for the structure and function of your brain cells.
At the same time, it’s just as important to minimize sugar, caffeine, and highly processed foods. These can cause energy spikes and crashes that feel almost identical to—or even worsen—PAWS symptoms.
Master Your Mind with Mindfulness and Stress Reduction
So many PAWS symptoms stem from a dysregulated nervous system. That constant feeling of being on edge is completely exhausting and can make you feel powerless. Learning practical stress-reduction techniques is essential for regaining a sense of control. Figuring out how to calm your nervous system gives you simple, effective steps for lasting relief.
Mindfulness and meditation are incredibly powerful tools for this. They train you to observe your thoughts and feelings without getting swept away by them.
One of the most effective techniques for this is called urge surfing. When a wave of anxiety or a craving hits, instead of fighting it, you just observe it with curiosity. Notice how it feels in your body, watch it build, crest, and eventually fade away on its own. This practice teaches you that these intense feelings are temporary and that you have the power to ride them out without acting on them.
To help put all of this into practice, we've created a simple checklist. Think of it as your daily guide to proactively managing PAWS and supporting your brain's recovery, one small step at a time.
Your Daily PAWS Management Checklist
| Activity | Benefit | Practical Tip |
|---|---|---|
| Consistent Wake/Sleep | Regulates circadian rhythm, improving mood and sleep quality. | Set an alarm for both waking up and winding down for bed. |
| Scheduled Meals | Stabilizes blood sugar and energy, reducing mood swings. | Eat a small, balanced meal or snack every 3-4 hours. |
| Hydration | Supports brain function and reduces fatigue and brain fog. | Keep a water bottle with you and aim for 8 glasses a day. |
| Mindful Movement | Releases endorphins and reduces stress hormones like cortisol. | Take a 15-20 minute walk outside without your phone. |
| Mindfulness Practice | Calms the nervous system and helps you detach from cravings. | Try a 5-minute guided meditation or "urge surfing" when a craving hits. |
| Limit Caffeine/Sugar | Prevents energy crashes that can mimic or worsen PAWS symptoms. | Swap your afternoon coffee for herbal tea or sparkling water. |
Using this checklist daily helps build the small, consistent habits that make the biggest difference in navigating PAWS. It's about taking intentional action to support your healing, day in and day out.
The Role of Community in Navigating PAWS
Making it through post-acute withdrawal syndrome is rarely a solo mission. The emotional waves and cognitive fog can feel incredibly isolating, which is why a strong support system isn't just nice to have—it's one of the most essential tools for staying the course.
Connection is a powerful antidote to the confusion of PAWS. It’s the constant reminder that you aren’t alone on this path, even when your own mind feels like an unfamiliar place. Your inner circle of family and friends can be your greatest champions, but they often need a little coaching on how to help in a way that actually helps.
Educating Your Support System
For your loved ones to give you the backup you really need, they have to understand what you're up against. The first step is explaining that PAWS isn't a relapse or a sign of weakness; it's a physical healing process happening inside your brain. Patience is the single most important gift they can give you.
Encourage them to learn about the common symptoms and the rollercoaster timeline of recovery. When they know that a sudden mood swing or a bout of fatigue is just your brain recalibrating, they can respond with empathy instead of frustration. It also helps to celebrate the small wins together—a week of stable moods, a full night of good sleep—because it reinforces progress and boosts morale for everyone.
A supportive community acts as an external anchor, providing stability when your internal world feels chaotic. Shared understanding transforms the recovery journey from a private struggle into a collaborative effort.
The Power of Peer Support
While family offers one kind of crucial support, there’s a unique validation that comes from connecting with people who have walked this exact same path. Peer support groups create a space where you don’t have to waste energy explaining yourself, because everyone in the room just gets it.
- Alcoholics Anonymous (AA) and Narcotics Anonymous (NA): These 12-step programs provide a time-tested framework for recovery built on shared experience. The sense of belonging you find there can be a powerful shield against the loneliness of PAWS.
- SMART Recovery: If you're looking for a secular, science-based alternative, SMART Recovery focuses on self-empowerment. It teaches practical, cognitive skills for managing the thoughts, feelings, and behaviors that PAWS can throw your way.
These groups do more than just reduce isolation; they provide living proof that you can get through this. Hearing stories from people who have successfully navigated PAWS gives you tangible hope on the days you need it most. Many people also discover that exploring the link between spirituality in the recovery process adds another layer of strength to their journey.
Ultimately, building this network is a proactive strategy for protecting your recovery. It means communicating your needs clearly, educating the people who care about you, and having the courage to connect with others who share your experience. This network becomes your safety net, ensuring that even when the symptoms feel overwhelming, you never have to face them alone.
Common Questions About Post Acute Withdrawal Syndrome
Navigating the strange and often frustrating territory of recovery brings up a ton of questions. When it comes to post acute withdrawal syndrome, getting clear, straightforward answers can make all the difference. Let's tackle some of the most common concerns to help you feel more grounded on your journey.
One of the biggest fears is whether this feeling is permanent. The short answer is a definite no. While the experience is different for everyone, PAWS is a temporary phase of recovery. Think of it as your brain's healing process playing out in real-time. It’s a sign that your mind is working hard to recalibrate, and while that process takes time, it absolutely has an end point.
Is This PAWS or Something Else?
It’s completely normal to wonder if what you're feeling is PAWS or a separate mental health issue like depression or an anxiety disorder. The key difference is often in the pattern of the symptoms. PAWS symptoms tend to show up in waves, with good days or even weeks sprinkled in between the tough ones.
In contrast, a primary mental health condition usually involves more persistent, chronic symptoms that don't let up as frequently. The only way to know for sure is to get a professional evaluation. Co-occurring conditions are incredibly common, and getting an accurate diagnosis ensures you get the integrated treatment needed to address both.
Can PAWS Be Cured?
There isn't a magic pill or a single "cure" for PAWS in the way you might cure an infection. Instead, it’s something you manage and move through over time with consistent, healthy choices. The most effective approach involves a combination of strategies:
- Evidence-based therapies like Cognitive Behavioral Therapy (CBT) to build practical coping skills.
- Healthy lifestyle habits, including good nutrition, regular exercise, and a predictable routine.
- Strong community support from peers, support groups, and family.
- Professional medical oversight to help manage any severe symptoms that crop up.
This multifaceted approach doesn't make PAWS disappear overnight, but it does dramatically shorten the timeline and lessen the intensity of the symptoms. Each positive step actively helps your brain complete its healing process.
The goal isn't to find a quick fix but to build a resilient foundation that supports your brain's natural recovery. Every healthy choice you make is a direct investment in shortening the PAWS timeline.
When Should I Seek Immediate Help?
While most PAWS symptoms are manageable, some signs are red flags that require immediate professional attention. If you experience any thoughts of self-harm or suicide, it is critical to contact a healthcare provider or a crisis service right away.
Additionally, if your symptoms suddenly become much worse or you have signs of a medical emergency, don't wait. It’s always better to be cautious and seek help when you're unsure.
Navigating the ups and downs of post acute withdrawal syndrome is a serious challenge, but you don't have to do it alone. The structured support and expert guidance at Altura Recovery provide a steady hand through this critical phase of healing. Learn more about our outpatient programs and start your journey to lasting recovery today.