It’s one of the most common points of confusion in healthcare: Are addiction and dependence the same thing? People often use the terms interchangeably, but they describe two very different conditions. Getting the distinction right isn't just about semantics; it's fundamental to understanding the problem and finding the right kind of help.
The simplest way to think about it is this: Dependence is a physical state, while addiction is a behavioral one.
Think of someone taking blood pressure medication. Over time, their body adapts and comes to rely on the drug to maintain normal function. If they stop taking it abruptly, they'll likely experience physical withdrawal symptoms. Their body has developed a physiological dependence. This is a predictable biological response, not a sign of addiction.
Addiction, which clinicians now call a Substance Use Disorder (SUD), is a much more complex brain disease. It’s defined by compulsive, out-of-control substance use despite obvious, mounting negative consequences. It fundamentally changes the brain's reward, motivation, and memory circuits, creating intense cravings and distorting decision-making.
You can absolutely be dependent on a substance without being addicted. However, if you are addicted, you are almost certainly physically dependent as well.
Defining Addiction and Dependence A Clear Comparison
Let's break down the core differences. While they often overlap, one is a physical adaptation and the other is a psychological and behavioral condition that lives in the brain.
Dependence is the body's natural response to consistent exposure to certain substances. Your system adapts and learns to function with the substance present, leading to tolerance (needing more for the same effect) and withdrawal (physical symptoms when you stop). This can happen with many prescribed medications, even when taken exactly as a doctor ordered.
Addiction, on the other hand, is marked by a loss of control. It’s the inability to stop using despite the damage it’s causing to your health, your job, your finances, or your relationships. It's the compulsive pursuit of a substance that hijacks your priorities and judgment.
Addiction vs Dependence At a Glance
Sometimes, seeing the contrast side-by-side makes it click. When trying to understand any health condition, precise definitions are key. Reviewing resources that explain how various mental health conditions differ can offer a good perspective on why this clarity matters so much in healthcare.
This table cuts through the noise and highlights the fundamental distinctions.
| Characteristic | Dependence | Addiction |
|---|---|---|
| Primary Nature | Physiological and physical | Behavioral and psychological |
| Key Indicators | Tolerance and physical withdrawal | Cravings, compulsive use, loss of control |
| Role of Harm | Not an inherent component | A defining characteristic |
| Decision-Making | Judgment and control are intact | Impaired judgment and decision-making |
Thinking about the scale of this helps, too. In 2023 alone, an estimated 48.5 million Americans aged 12 or older were diagnosed with a substance use disorder. The chronic nature of addiction is underscored by relapse rates, which hover between 40% and 60%—a figure that highlights how the condition is much more than just a physical issue that resolves after detox.
Ultimately, recognizing the difference between a body's physical adaptation (dependence) and the compulsive, harmful behaviors of a brain disease (addiction) is the first critical step. It’s what empowers you to seek the right diagnosis and the right level of support.
A Look Inside the Brain: Dependence vs. Addiction
To really get the difference between addiction and dependence, you have to look at what’s happening under the hood—inside the brain. These aren’t just two ways of describing the same problem. They’re distinct neurological processes, different conversations between a substance and your body’s complex wiring.
At its most basic, physical dependence is a predictable, even logical, adaptation. When you introduce a substance regularly, your brain and body scramble to maintain balance, a state called homeostasis. This constant adjustment is what leads to tolerance (needing more to get the same effect) and physical withdrawal symptoms when the drug is taken away.
This biological recalibration isn’t a disorder in itself. It's just the body's way of setting a new baseline. Think of it like the thermostat in your house kicking into overdrive to keep the room at 70 degrees during a blizzard. In the same way, your body adjusts its own chemical production to function "normally" while the substance is present.
How Addiction Hijacks the Brain's Wiring
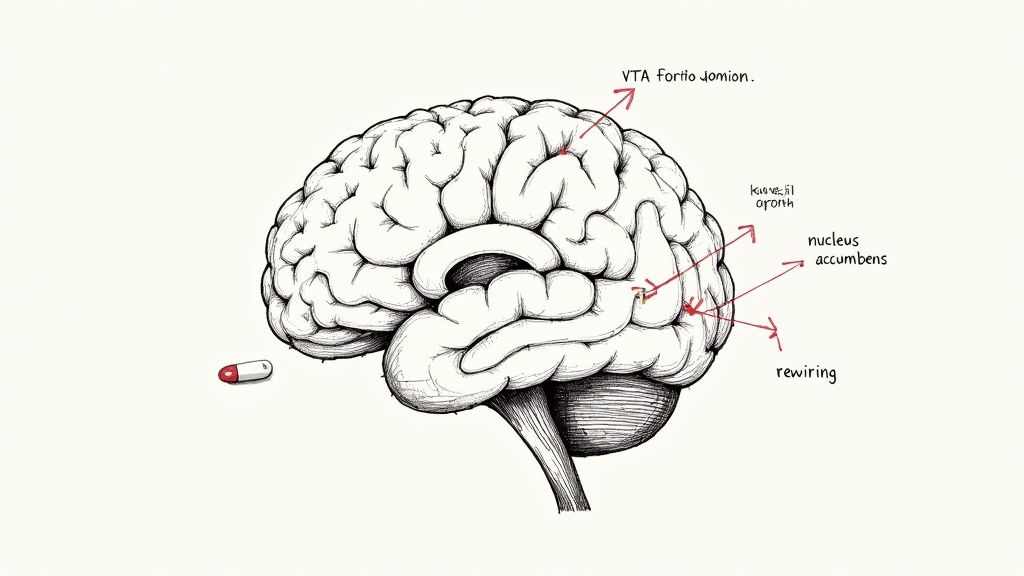
Addiction is a whole different beast. It’s a disorder that burrows deep into the brain's most primitive and powerful systems: reward, motivation, memory, and impulse control. It goes way beyond a simple physical adaptation and fundamentally rewires the circuits that guide our choices and tell us what’s important.
The main actor in this drama is dopamine, a neurotransmitter you’ve probably heard called the "feel-good" chemical. When someone uses a substance, the brain’s reward pathway gets flooded with dopamine, creating an intense feeling of pleasure and reinforcing the action. This powerful feedback loop trains the brain to see the substance as a massive reward, motivating the person to do it again and again.
Over time, the brain's reward system gets re-calibrated. It becomes less sensitive to natural, healthy pleasures like a good meal or a hug from a loved one. The substance becomes the main—and eventually, the only—thing that can deliver that sense of reward. This profound shift is what fuels the compulsive, out-of-control behaviors that define addiction.
Key Takeaway: Dependence is the body adjusting to a new chemical normal to avoid feeling sick. Addiction is the brain's motivation system getting hijacked, leading to a compulsive drive to use no matter the cost.
A Real-World Medical Scenario
Imagine a patient recovering from major surgery. They’re prescribed opioid painkillers for a few weeks to manage their pain. Without a doubt, their body will develop a physical dependence on the medication. If they were to stop cold turkey, they’d experience awful withdrawal symptoms—nausea, sweating, muscle aches.
But this patient isn't necessarily addicted. As long as they're taking the pills exactly as prescribed for pain relief, their brain’s reward circuits aren't driving compulsive, life-disrupting behavior. Once the pain is gone, they can work with their doctor to safely taper off the medication, manage the withdrawal, and let their body readjust. They won't feel the overwhelming cravings or loss of control that are the hallmarks of addiction.
This distinction is critical. Global data shows that around 2.2% of the world’s population has struggled with alcohol or illicit drug use disorders—conditions defined by the compulsive element of addiction, not just dependence. This tells us that while dependence is often part of addiction, addiction itself involves a deep-seated behavioral pathology that pushes someone to keep using even when their world is falling apart. You can learn more about these global substance use trends here.
Ultimately, the neurobiology explains why one is a manageable physiological state and the other is a chronic brain disease that requires comprehensive treatment. Dependence is about the body needing a substance to avoid withdrawal. Addiction is about the brain’s corrupted drive to chase a reward at any and all costs.
Recognizing the Distinct Signs and Symptoms
Telling the difference between physical dependence and addiction isn't just for clinicians—it’s a crucial skill for anyone trying to figure out what’s really going on. The signs for each are distinct, with one showing up in the body and the other playing out in our behaviors and choices. Getting clear on these signals is the first step toward finding the right kind of help.
Physical dependence makes itself known through clear, uncomfortable, and sometimes dangerous physical signals. When your body gets used to having a substance around, taking it away throws your system into chaos, triggering withdrawal. These symptoms are impossible to ignore.
For someone dependent on opioids, withdrawal might feel like a terrible flu:
- Deep muscle aches and cramping
- Nausea, vomiting, or diarrhea
- Sweating, chills, and goosebumps
- A runny nose and watery eyes that won’t quit
Someone coming off alcohol or benzodiazepines faces a different storm, including tremors, headaches, or even life-threatening seizures. These are not subtle hints; they are the body’s alarm bells, screaming that its chemical balance has been hijacked.
The Behavioral Red Flags of Addiction
Addiction, on the other hand, tells its story through actions, priorities, and consequences. While physical dependence is often part of the picture, the real markers of addiction are behavioral. These are the red flags that show substance use has morphed from a physical issue into a compulsive pattern that has taken over the driver's seat.
To spot addiction, we have to look past the physical symptoms and start asking tough questions about how a person is living their life. The focus shifts from, "How does my body feel without it?" to "How is my life falling apart because of it?"
Addiction is less about physical withdrawal and more about a person's relationship with a substance—a relationship that becomes prioritized above health, family, and personal responsibilities.
Think of these questions as a mirror for spotting the behavioral patterns of addiction:
- Neglecting Responsibilities: Have you started dropping the ball at work, school, or home because of your substance use?
- Social and Interpersonal Problems: Are you still using even though it’s causing fights with the people you care about most?
- Loss of Interest: Have you given up on hobbies or activities that used to bring you joy?
- Risky Use: Do you find yourself using in dangerous situations, like before driving a car?
- Loss of Control: Do you often use more than you planned, or for longer than you intended?
- Failed Attempts to Quit: Have you tried to cut back or stop completely but found you couldn't?
These questions get to the heart of the matter. One condition is about the body’s chemistry; the other is about a life losing its way.
A Tale of Two Scenarios
Let's look at two people using the same prescribed opioid medication to see how this plays out in the real world.
Scenario 1: The Dependent Patient
Sarah is recovering from major knee surgery. She takes her pain medication exactly as her doctor directs, never taking an extra dose and using it only to manage her post-op pain. Once the pain subsides, her doctor helps her slowly taper the dose to avoid severe withdrawal. She feels some physical discomfort as her body readjusts, but she has zero cravings or desire to get more of the drug. Sarah experienced physical dependence.
Scenario 2: The Addicted Individual
Mark also started taking opioids after an injury. But soon, he wasn’t just using them for pain—he was taking extra pills to numb his stress. He started running out of his prescription early, "doctor shopping" for more, and lying to his family about his use. His work is suffering and he’s constantly arguing with his partner, but he can’t imagine stopping. Mark is showing the compulsive behaviors of addiction.
The global scale of these issues is staggering. The World Health Organization (WHO) reports that over 3 million deaths each year are linked to alcohol and drug use. In 2019, around 209 million people met the criteria for alcohol dependence alone. But it’s the compulsive behaviors of addiction that fuel the most severe health crises and social damage behind that number. While physical dependence is a widespread medical issue, addiction is what truly devastates lives. You can learn more from the WHO report on substance use.
How Treatment Approaches Differ For Each Condition

Because addiction and dependence are fundamentally different, throwing a one-size-fits-all treatment at them just doesn't work. Each condition presents its own unique set of challenges, so the strategies we use must be just as distinct. Getting this right is the first step toward finding support that actually heals.
When we're dealing with physical dependence, the first stop is almost always medically supervised detoxification. The entire point of detox is to safely manage the body's withdrawal symptoms as a substance leaves the system. It’s a clinical process focused squarely on physical stabilization, making a rough and sometimes dangerous transition as comfortable as possible.
But here’s a critical—and dangerous—misconception: detox is not a cure for addiction. It’s a necessary first step for someone who is both dependent and addicted, but on its own, detox does nothing to address the deep-seated behaviors and psychological drivers that keep addiction going.
Beyond Detox: The Core of Addiction Treatment
True recovery from addiction demands a much broader, more intensive game plan. The goal isn't just to get the substance out of the body; it's about healing the brain, rewiring behaviors, and building a new life where substances are no longer the focal point. This is where comprehensive, integrated care becomes absolutely vital.
Effective addiction treatment moves far beyond the physical and dives straight into the mind. It involves therapies that help people understand the root causes of their substance use, develop healthy ways to cope, and unlearn the compulsive patterns that took over.
Treatment for dependence stops when the body is stable. Treatment for addiction is a long-term journey of healing the mind, repairing relationships, and building a foundation for a life in recovery.
This deeper work is the cornerstone of programs like a Partial Hospitalization Program (PHP) or an Intensive Outpatient Program (IOP). These structured, supportive settings provide the tools needed for a change that actually lasts.
Integrated Care for Lasting Recovery
Outpatient programs like IOP and PHP offer a powerful blend of therapeutic services designed to address every facet of addiction. Unlike a simple detox, they equip people with the skills to navigate life's challenges without turning back to substances.
So, how does the focus of care really differ? Let's break it down.
Treatment Focus for Dependence vs Addiction
The following table makes the distinction crystal clear: managing dependence is a short-term medical task, while treating addiction is a long-term healing process.
| Aspect of Care | Focus for Dependence | Focus for Addiction |
|---|---|---|
| Primary Goal | Safely manage physical withdrawal symptoms | Address compulsive behaviors and underlying psychological issues |
| Duration of Care | Short-term, lasting days to weeks | Long-term, involving months of therapy and ongoing support |
| Core Methods | Medical supervision and medication management | Psychotherapy, counseling, skill-building, and relapse prevention |
| Outcome | Physical stabilization | Sustainable behavioral change and improved quality of life |
As you can see, the methods and goals are worlds apart. One stabilizes the body, while the other rebuilds a life.
These programs integrate various evidence-based therapies to make that happen. For instance, exploring the goals of Cognitive Behavioral Therapy shows how individuals learn to identify and change the destructive thought patterns that fuel addictive behavior. This is the kind of work that creates real, sustainable recovery.
Beyond traditional talk therapy, many find strength in complementary practices. Learning about the transformative benefits of journaling for mental health can provide a powerful outlet for self-reflection and emotional regulation—an essential skill when navigating the ups and downs of recovery. It's all about building a robust toolkit of coping strategies.
Ultimately, the difference is night and day. Managing dependence is a short-term medical procedure. Overcoming addiction is a comprehensive journey of personal growth and healing that requires structured, long-term support.
Debunking Common Myths About Addiction
Misunderstandings about addiction and dependence are everywhere. More than just being inaccurate, they fuel a stigma that can stop people from ever reaching out for help. Getting the facts straight isn't an academic exercise—it’s about creating a more compassionate and effective way to approach a serious health issue.
Let’s clear up some of the most persistent and damaging misconceptions.
A major myth is that addiction is a problem reserved for illegal substances like heroin or cocaine. That’s completely off the mark. Addiction can take root with any substance that rewires the brain’s reward system, including perfectly legal ones like alcohol, nicotine, and prescription medications.
The legal status of a substance is irrelevant. The real issue is its effect on a person's behavior. For instance, the compulsive use of prescribed opioids can be every bit as devastating as a street drug habit. The defining factor is always the loss of control and continuing to use despite the mounting negative consequences.
Myth 1: Experiencing Withdrawal Means You Are Addicted
This is probably the single most common point of confusion. Many people assume that if someone has physical withdrawal symptoms when they stop using a substance, they must be addicted. While withdrawal is a clear sign of physical dependence, it is not the defining feature of addiction.
Think back to the patient taking prescribed pain medication after surgery. Their body adapts and will definitely protest with withdrawal symptoms if they stop cold turkey. But if they have no psychological cravings or compulsive need to use the drug for non-medical reasons, they are not experiencing addiction.
The critical difference is the presence of compulsive, harmful behavior. Dependence is a physiological state; addiction is a behavioral disease rooted in the brain's reward circuitry.
Myth 2: Addiction Is Just a Lack of Willpower
Another incredibly harmful myth is that addiction is a moral failing or a simple lack of self-control, suggesting people could just “stop if they really wanted to.” This idea flies in the face of decades of neuroscience. We now know that addiction is a chronic brain disorder that fundamentally hijacks decision-making, impulse control, and judgment.
The brain's reward pathways become so profoundly rewired that the urge to use a substance can feel as non-negotiable as the need for food or water. It’s not about willpower; it’s about a brain that has been structurally and chemically altered. Overcoming addiction requires medical and therapeutic intervention, not shame.
The Shift to More Accurate Language
To fight this stigma, the clinical community has largely moved away from loaded terms like "addict" and "abuse." The preferred diagnosis is now Substance Use Disorder (SUD), which is understood to exist on a spectrum from mild to severe.
This change in language is deliberate and powerful:
- It’s Person-First: It reminds us that we're talking about a person with a medical condition, not someone defined by their illness.
- It’s Medically Accurate: It correctly frames the issue as a diagnosable disorder, putting it in the same category as other chronic conditions like diabetes or heart disease.
- It Reduces Stigma: It shifts the conversation from morality and judgment to healthcare and solutions.
Using the right words and debunking these myths helps everyone see the situation more clearly. It also highlights the need for structured, professional care. Understanding what a real recovery journey looks like, including exploring questions like how long outpatient rehab lasts, provides a realistic view that goes far beyond just getting through withdrawal.
Knowing When to Seek Professional Help
Taking that first, honest look at yourself or a loved one and admitting something feels wrong is a huge step. But the crucial follow-up question is, “Is it bad enough to need professional help?”
While self-awareness is the starting point, a clinical diagnosis is what sets the stage for a recovery plan that is both effective and, most importantly, safe.
If substance use is creating constant friction in your life—blowing up relationships, getting in the way of work or school, or causing serious financial stress—it’s time. It’s definitely time if you've tried to stop on your own, maybe even succeeded for a bit, but always find yourself right back where you started. Those are the classic signs that a manageable dependence has crossed over into a substance use disorder.
Picking up the phone to call a healthcare provider or a treatment center like ours is the single most powerful thing you can do to take back control. An initial assessment isn’t an interrogation; it's a confidential, judgment-free conversation where our clinicians simply try to understand your story.
What to Expect During an Assessment
During this evaluation, we'll ask about your history with substances, your mental health, and what’s been going on in your life. This isn't just about checking boxes. It’s about figuring out the right level of care for you.
The goal is to build a personalized treatment plan that addresses your specific needs, whether that means managing the physical side of dependence, treating the compulsive behaviors of addiction, or—as is often the case—both.
This infographic can help clear up some of the key distinctions and bust a few common myths that unfortunately keep people from reaching out sooner.
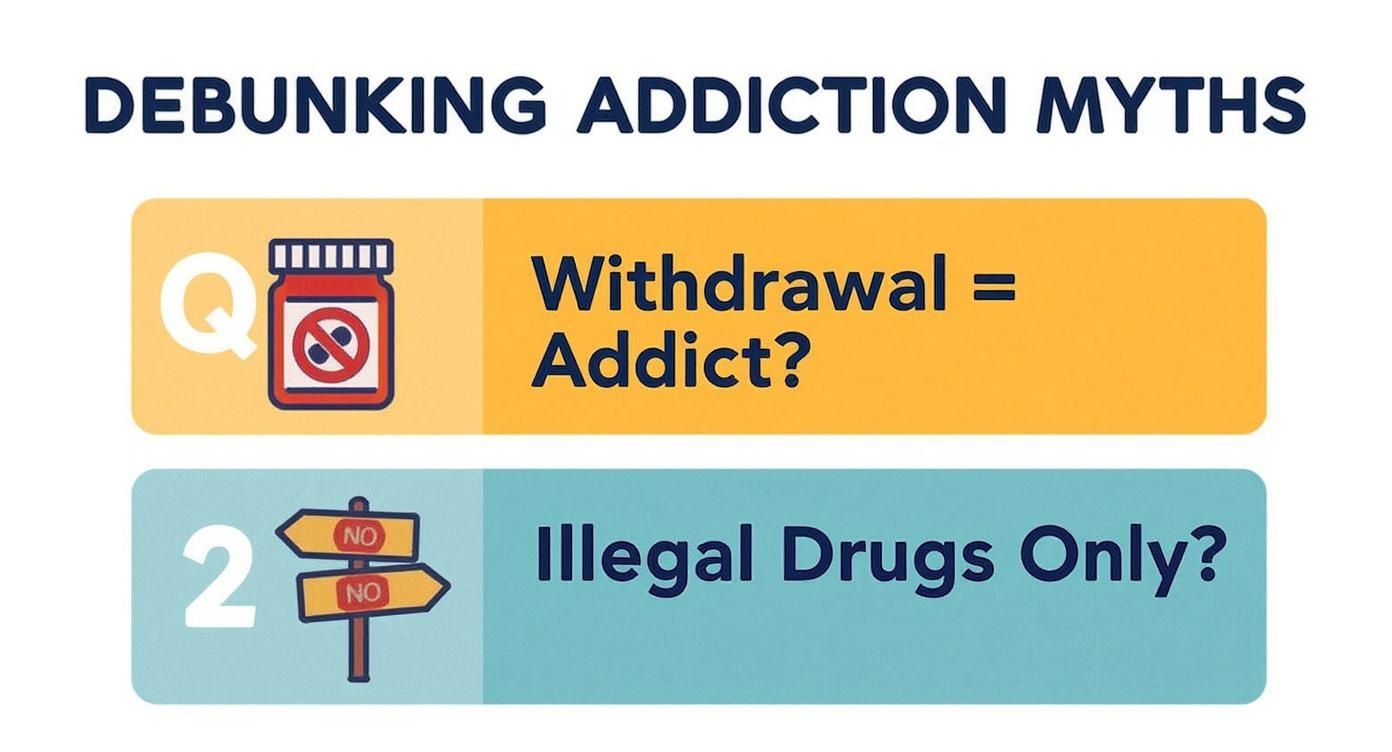
As you can see, experiencing withdrawal doesn't automatically mean someone is addicted, just as addiction isn't something that only happens with illegal drugs.
The good news? Recovery is absolutely achievable when you have the right support system in place. Structured programs are designed to offer intensive therapeutic care while still letting you handle your responsibilities at home and work. To get a better feel for how these flexible yet powerful models work, you can learn more about what outpatient mental health treatment entails and how it helps create real, lasting change.
Reaching out is the first and most important action you can take. It’s the move that starts building a healthier future, today.
Frequently Asked Questions
When you start digging into the world of substance use, a lot of questions pop up. It's a confusing landscape. Here, we'll clear up some of the most common points of confusion around addiction and dependence, giving you straight answers based on years of clinical experience.
Can You Have an Addiction Without Being Physically Dependent?
Absolutely. It’s a common misconception that addiction is all about physical withdrawal, but the reality is more nuanced. Addiction is driven by the brain's reward system, not just the body's physical adaptation to a substance.
You can be addicted to something without ever experiencing the shakes or flu-like symptoms of physical withdrawal. Think about behaviors like gambling or substances like cannabis. While they might not cause severe physical dependence, they can absolutely fuel a powerful psychological addiction. The core of addiction is compulsive use, intense cravings, and continuing the behavior despite watching your life get worse. It’s a disorder of motivation and choice, which is why it can exist entirely separate from physical dependence.
How Long Does It Take to Develop a Physical Dependence?
There’s no magic number or universal timeline here. How quickly someone develops a physical dependence varies wildly from person to person and from substance to substance. It’s a complex mix of chemistry and biology.
Several key factors determine the speed:
- The specific substance: Some drugs, like opioids and benzodiazepines, can create physical dependence surprisingly fast—sometimes in just a few weeks of consistent use.
- Dosage and frequency: Taking higher doses more often is like hitting the fast-forward button on dependence.
- Your own biology: Things like your metabolism, genetic predispositions, and overall health play a huge role in how your body adapts.
Because of this, trying to pin down a specific timeframe is impossible. The more important thing is to recognize the signs when they appear and understand that dependence is simply a predictable physiological response when a substance is taken consistently over time.
What’s the First Step if I Think I Have an Addiction?
That moment of realization—when you first suspect you might have an addiction—is huge. It’s a brave and critical turning point. The most important first step you can take is to get a professional, confidential assessment to figure out what’s really going on. Reaching out isn’t a sign of weakness; it’s an act of strength.
The goal of this first step isn't to sign up for a lifelong program. It's simply about getting information—a clear, expert opinion on your situation. This one action can set the entire course for healing and getting your life back.
Here are a few effective first steps:
- Talk to your primary care doctor. They can do an initial screening and point you toward a specialist.
- Call a confidential support line. You can talk to a trained professional who understands what you're going through.
- Contact a treatment center for a formal evaluation. This will help determine exactly what level of care is right for you.
For many people, addiction doesn't travel alone; it's often tangled up with mental health challenges like anxiety or depression. Knowing how to get help for both is key, which is why learning about finding effective dual diagnosis treatment programs can be such a valuable part of this process. A good assessment will clarify the best path forward for your specific needs.
At Altura Recovery, we know that understanding your situation is the first step toward getting better. If you or someone you care about is struggling, our team is here to provide a confidential assessment and create a personalized outpatient treatment plan that fits your life. Contact us today to begin your journey toward real healing and lasting freedom.