Integrated treatment for dual diagnosis is a fancy term for a common-sense idea: if someone is struggling with both a substance use disorder and a mental health condition, you have to treat them at the same time. It’s a modern, evidence-based approach that finally moves past outdated models to treat the whole person, creating a much stronger foundation for lasting recovery.
Decoding Integrated Treatment for Dual Diagnosis
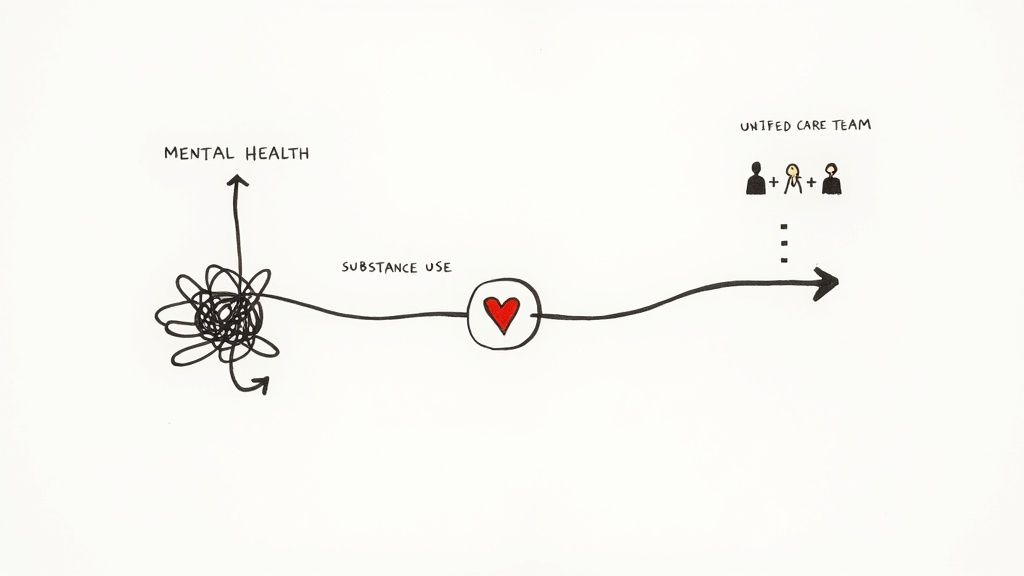
Imagine trying to patch two different holes in a sinking boat, but you’re only allowed to work on one at a time. As you fix the first hole, water keeps pouring in through the second, making all your hard work feel pointless. That’s exactly what it feels like when mental health and substance use are treated separately. An unmanaged mental health issue can easily trigger a relapse, while active substance use almost always makes symptoms of depression or anxiety worse.
Integrated treatment for dual diagnosis breaks this frustrating cycle. It’s built on a simple yet powerful philosophy: since the two conditions are so deeply intertwined, they absolutely must be treated together.
The core idea is that one clinical team addresses both the substance use and the mental health disorders at the same time, under one roof. This gets rid of the confusion and conflicting advice that happens when people see separate specialists who aren't talking to each other.
The Problem with Separated Care
In older, fragmented models, a person might be told by a mental health clinic to get sober before they can get therapy for their anxiety. At the same time, a substance use program might not have the expertise to properly address that same person's underlying panic attacks—which are the primary reason they started drinking in the first place.
This disjointed approach often leaves people feeling stuck and misunderstood, bouncing between different providers without ever making real progress.
A Widespread Challenge
This isn't a niche problem. In the United States, roughly 9.5 million adults had a dual diagnosis in a single recent year. Despite how common this is, only about 10% of people with co-occurring disorders get care that addresses both conditions simultaneously, which points to a huge gap in our healthcare system.
You can learn more about the prevalence of dual diagnosis from recent findings. This treatment gap leads to higher rates of hospitalization, relapse, and other painful consequences.
Integrated vs Sequential Treatment Models At a Glance
To see the difference clearly, it helps to compare the modern integrated model with the older, less effective approaches.
| Feature | Integrated Treatment | Sequential or Parallel Treatment |
|---|---|---|
| Philosophy | Treats the whole person; conditions are intertwined. | Treats conditions as separate, unrelated problems. |
| Care Team | One multidisciplinary team works together. | Multiple, separate teams who rarely communicate. |
| Timing | Both conditions are addressed simultaneously. | One issue is treated first, then the other (or at different clinics). |
| Patient Experience | Cohesive, consistent, and less confusing. | Fragmented, conflicting advice, feels like bouncing around. |
| Outcomes | Higher engagement, lower relapse rates, better overall health. | Poorer outcomes, higher dropout rates, frequent relapse. |
The unified approach of an integrated treatment for dual diagnosis program is a direct solution to this chaos. By creating a single, cohesive treatment plan, it tackles the complex relationship between mental health and substance use head-on. This ensures that progress in one area supports and strengthens progress in the other, paving the way for a more stable and sustainable recovery.
Why a Unified Approach Leads to Better Outcomes
Treating co-occurring disorders at the same time isn’t just a good idea—it’s the most effective strategy for building a recovery that actually lasts. When mental health and substance use are handled separately, it often creates a frustrating "revolving door" effect. A person might leave a rehab facility with new skills for staying sober, only to relapse the moment their untreated anxiety flares up.
This happens because the two conditions are deeply intertwined, feeding each other in a destructive loop. An integrated treatment for dual diagnosis finally breaks that cycle by treating the whole person, not just a collection of symptoms. This unified approach creates a powerful synergy where getting better in one area directly fuels progress in the other.
As someone gets a handle on their substance use, the mental fog starts to lift. That newfound clarity makes it possible to truly engage in therapy and work on the underlying emotional issues. On the flip side, as they learn healthier ways to manage depression or anxiety, the urge to self-medicate with substances starts to fade.
The Tangible Benefits of Integrated Care
Research has shown time and again that when mental health and substance use are treated simultaneously, the results are dramatically better. This isn't just a theory; it's a proven model that leads to real, life-changing outcomes.
The evidence is clear: integrated treatment for dual diagnosis leads to better engagement in treatment, fewer relapses, and an improved quality of life compared to treating either condition on its own. You can explore the research on integrated care effectiveness to see the data on how this approach improves both retention and outcomes. It’s about building a much stronger foundation for the future.
Key benefits often include:
- Significantly Lower Relapse Rates: By addressing the root causes of substance use (like trauma or depression), people are far better equipped to handle triggers. Building these new coping skills for relapse prevention is a core part of a unified plan.
- Improved Housing and Employment Stability: When both conditions are managed, a person's ability to hold a job, maintain responsibilities, and secure stable housing increases substantially.
- Better Overall Quality of Life: Integrated care empowers people to build healthier relationships, engage in meaningful activities, and find a genuine sense of well-being.
- Reduced Hospitalizations and Legal Issues: A stable, cohesive treatment plan lowers the risk of the crises that so often lead to emergency room visits or legal trouble.
A unified approach stops the cycle of one untreated condition undermining the progress made on the other. It replaces fragmentation and confusion with a single, supportive plan that empowers individuals to build a resilient foundation for their future.
Building a Foundation for Lasting Recovery
Think of recovery like building a house. A sequential approach is like trying to put up the walls before you’ve poured the foundation—it’s unstable and bound to collapse. The mental health condition is the ground, and the substance use is the shaky structure built on top of it.
An integrated treatment for dual diagnosis program makes sure that foundation is solid first. It addresses the core issues driving addictive behaviors, creating a stable base upon which a healthy, sober life can be built. This method doesn't just put a temporary patch on the problem; it provides the tools, skills, and support needed to break the cycle for good and move forward with confidence.
The Building Blocks of an Effective Program
A high-quality integrated treatment program is more than a list of services—it’s a carefully built ecosystem designed to help the whole person heal. Think of it like a specialized medical team for a complex illness. You wouldn’t want a heart surgeon and a lung specialist working in separate hospitals without ever talking. You’d want a unified team working together on a single, comprehensive plan.
That's exactly how an effective program for co-occurring disorders works. It brings a multidisciplinary team of therapists, psychiatrists, and case managers together under one roof. This collaborative approach makes sure every part of a person's care is aligned, preventing the mixed messages and fractured care that often derail recovery in less coordinated settings.
The Comprehensive Assessment Process
The journey always starts with a thorough and compassionate assessment. This isn’t just a checklist; it's a deep dive to understand the unique, complex dance between a person’s mental health symptoms and their substance use patterns. The goal is to see the full picture—not just “anxiety” and “alcohol use,” but exactly how one fuels the other.
This initial evaluation is the foundation for a truly personalized treatment plan. A skilled clinical team will explore:
- The history and severity of both the mental health condition and the substance use.
- Any underlying trauma or life events that keep the cycle going.
- The individual's personal strengths, motivations, and recovery goals.
This process ensures the treatment plan isn't a one-size-fits-all template but a tailored roadmap built for one person’s specific journey.
Understanding Different Levels of Care
Integrated treatment isn’t a single program. It’s a spectrum of care designed to meet people exactly where they are. Two of the most common levels you'll find in an outpatient setting are Partial Hospitalization Programs (PHP) and Intensive Outpatient Programs (IOP).
A Partial Hospitalization Program (PHP) offers a high level of support, often serving as a step-down from residential treatment. A typical PHP week involves structured therapy and psychiatric services for several hours a day, five days a week, which allows the individual to return home each evening.
An Intensive Outpatient Program (IOP) provides more flexibility. With programming for just a few hours a day, three to five days a week, IOP lets people better balance treatment with their work, school, or family responsibilities. This structure helps them practice new coping skills in the real world while still getting robust clinical support.
The goal of this step-down approach is to provide the right amount of support at the right time. As a person gains stability and confidence, their level of care can be adjusted, creating a smooth and sustainable transition back into daily life.
The infographic below shows how this unified approach directly improves key areas of a person's life, leading to more stable, lasting recovery.

This visual makes it clear: when care is truly integrated, it doesn't just treat symptoms. It builds a foundation for a better future by reducing relapse and improving overall stability.
This structured environment is where individuals dive into various therapeutic activities. From one-on-one counseling to group therapy, every component is designed to build resilience. Many programs cover a wide range of group therapy topics for addiction, helping clients connect with peers who get it and learn from their shared experiences. It's this combination of expert coordination, personalized planning, and structured support that forms the unshakable foundation of a successful integrated treatment for dual diagnosis.
Therapies That Target Co-Occurring Disorders
An effective integrated treatment for dual diagnosis program goes far beyond general support. It deploys specific, evidence-based therapies designed to untangle the knot of co-occurring conditions. Think of these therapies as specialized tools in a clinician's toolkit. You wouldn't use a sledgehammer to fix a delicate watch; likewise, we use targeted therapeutic models to address the unique challenges of dual diagnosis.
These methods aren't just about talking through problems. They’re about building practical skills to change the thoughts, emotions, and behaviors that fuel the cycle of mental health symptoms and substance use. Let's explore some of the most powerful and commonly used therapies in a unified care setting.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy, or CBT, is a cornerstone of modern treatment. It works on a straightforward principle: our thoughts, feelings, and behaviors are all deeply connected. Harmful thought patterns can trigger distressing emotions, which in turn can lead to self-destructive actions like turning to substances.
CBT helps you become a detective of your own mind, learning to spot and challenge the automatic negative thoughts that spark cravings or feelings of hopelessness.
For example, a person with social anxiety and an alcohol use disorder might think, "I can't go to that party sober; everyone will find me boring." CBT teaches them to question that belief, reframe it, and find the evidence. A new thought might be, "I might feel anxious, but I can handle it for an hour. My real friends will appreciate me for who I am, not whether I'm drinking."
By rewiring these cognitive distortions, CBT directly weakens the link between a mental health trigger and the impulse to use.
Dialectical Behavior Therapy (DBT)
While CBT hones in on thoughts, Dialectical Behavior Therapy (DBT) is especially powerful for managing intense, overwhelming emotions. Originally developed to help individuals with borderline personality disorder, its effectiveness has been proven for a wide range of issues, including substance use, PTSD, and the severe mood swings common in dual diagnosis.
DBT provides a concrete set of skills across four key areas, giving people practical tools to navigate emotional storms without turning to substances.
- Mindfulness: Learning to stay grounded in the present moment, observing thoughts and feelings without judgment.
- Distress Tolerance: Developing skills to survive painful moments without making them worse through impulsive actions.
- Emotion Regulation: Understanding and changing intense, unwanted emotions in a healthy way.
- Interpersonal Effectiveness: Building skills to communicate needs, set boundaries, and maintain healthy relationships.
For someone with bipolar disorder and a substance use issue, DBT offers a real alternative to using drugs or alcohol to cope with jarring mood shifts. Instead of reacting impulsively, they can use distress tolerance skills to get through the moment safely.
Motivational Interviewing (MI)
Change is hard. Simply telling someone they have to change rarely works and often backfires. Motivational Interviewing (MI) flips the script. It’s a collaborative, respectful counseling style designed to help you discover your own internal motivation to change.
Instead of acting as an authority figure, the therapist becomes a guide, helping the person resolve their ambivalence about recovery. MI is incredibly useful in integrated treatment for dual diagnosis because it meets people exactly where they are, without judgment.
An MI session isn't a lecture. It’s a guided conversation where the therapist asks open-ended questions like, "What are some of the good things about using, and what are some of the not-so-good things?" This helps the individual weigh the pros and cons for themselves, strengthening their own commitment to building a better life.
This process empowers people to find their own reasons for wanting to heal, which is a far more powerful and lasting motivator than any external pressure.
These core therapies are often just the beginning. A comprehensive integrated treatment plan will also include other powerful approaches tailored to the individual's needs.
Common Therapies Used in Integrated Treatment
Here's a quick look at how different therapeutic models are applied to the specific challenges of dual diagnosis, each playing a unique role in the healing process.
| Therapy Model | Primary Focus | Example Application in Dual Diagnosis |
|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Identifying and changing negative thought patterns and behaviors. | Helping a client with depression and alcohol use recognize that the thought "I'm a failure" triggers the urge to drink, then developing healthier self-talk. |
| Dialectical Behavior Therapy (DBT) | Building skills for emotion regulation, distress tolerance, and mindfulness. | Teaching someone with PTSD and a benzo dependency how to use grounding techniques during a flashback instead of taking an unprescribed pill. |
| Motivational Interviewing (MI) | Resolving ambivalence and strengthening internal motivation for change. | Guiding a conversation with someone who is unsure about quitting cannabis, helping them connect their use to their stalled career goals. |
| Family Systems Therapy | Improving communication and resolving conflict within family dynamics. | Working with a family to change enabling behaviors and build a supportive home environment for a loved one with bipolar disorder and a stimulant use disorder. |
| Trauma-Informed Therapies (e.g., EMDR) | Processing and healing from past traumatic experiences. | Using Eye Movement Desensitization and Reprocessing (EMDR) to reduce the emotional charge of a traumatic memory that fuels an opioid use disorder. |
By combining these proven methods, an integrated program gives individuals a robust toolkit to manage both their mental health and their sobriety.
These therapies are delivered in various formats, including one-on-one counseling, group sessions, and family therapy. Understanding how family dynamics impact recovery is crucial, as a supportive home environment can make all the difference. To dive deeper, you can learn more about how relational patterns are addressed through what is family systems therapy in our detailed article.
When addressing co-occurring disorders, a holistic approach may also include supportive tools. For individuals with ADHD as part of their dual diagnosis, assistive technology for ADHD can play a crucial role in managing symptoms and improving engagement with treatment plans. By weaving these proven methods together, an integrated program paves the way for sustainable, long-term wellness.
Navigating Your Path to Integrated Care
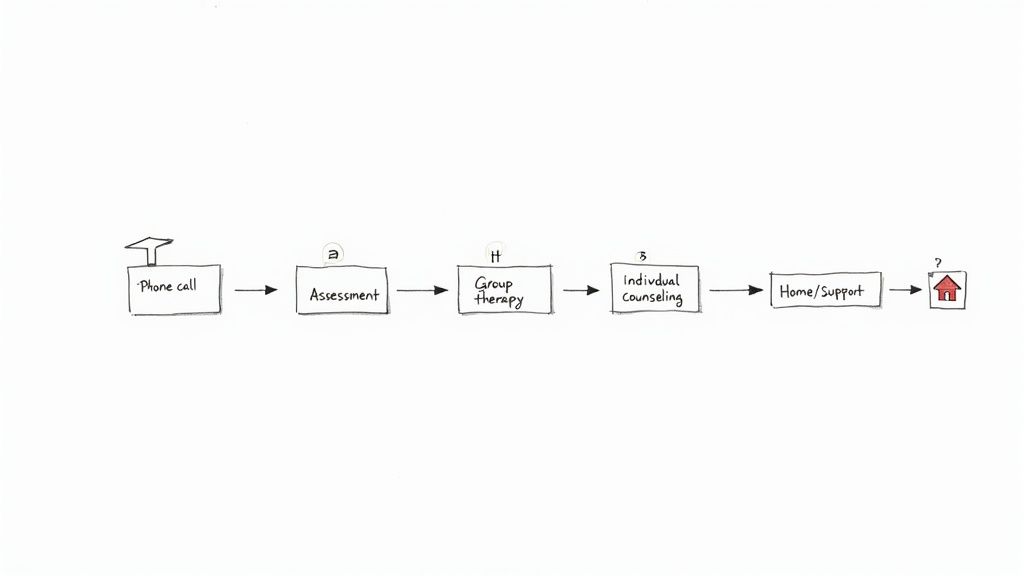
Making that first move toward recovery can feel like the hardest part. The fear of the unknown often paralyzes people, but getting a clear picture of the path ahead can replace that anxiety with confidence. Your journey into integrated treatment for dual diagnosis is a straightforward, supportive process designed to meet you exactly where you are today.
It all starts with a simple, completely confidential phone call. This is just a conversation—a no-pressure chance for you to ask questions and tell us what’s going on. From there, we’ll schedule a comprehensive assessment, which becomes the foundation for your entire recovery plan.
What to Expect During Your Initial Assessment
Think of the assessment as a compassionate, in-depth conversation with a clinical professional, not an interrogation. It’s a team effort to understand your unique story. The whole point is to see the complete picture of how your mental health and substance use are connected.
During this meeting, we’ll talk about things like:
- Your personal history with substance use.
- The mental health symptoms you've been experiencing.
- Your family background and current living situation.
- Your personal strengths and what you hope to achieve in recovery.
This honest dialogue is what allows our clinical team to build a treatment plan that’s actually built for you, ensuring both conditions get the attention they need right from the start.
Crafting Your Personalized Treatment Plan
After the assessment, our clinical team gets together to map out your treatment. This isn’t a one-size-fits-all handout; it’s a detailed strategy that reflects your specific needs, history, and goals. It will include a recommendation for a starting level of care, like a Partial Hospitalization Program (PHP) or an Intensive Outpatient Program (IOP).
Your personalized plan is a living document. It’s designed to be flexible, adapting to your progress as you move through different phases of recovery. The primary goal is to provide the right amount of support at every stage of your journey.
A typical week in an outpatient program is structured but flexible, weaving together different therapeutic activities that support real healing. For a deeper look into the day-to-day of our most intensive outpatient option, check out our guide to understanding a partial hospitalization program rehab.
Your schedule is designed to build skills and foster connection, ensuring you are constantly building resilience.
A Look at Daily Life in an Outpatient Program
Life in an integrated program is all about active engagement and learning new ways to live. You’ll be participating in different types of sessions that work together to address every angle of your dual diagnosis.
Your schedule will likely include a mix of:
- Individual Therapy: One-on-one sessions to dig deep into personal challenges and set clear therapeutic goals.
- Group Therapy: Small, professionally-led groups where you can share what you’re going through and learn from peers who actually get it.
- Psychiatric Care: Meetings with a psychiatrist for evaluation and medication management to support your mental health.
- Family Support: Workshops and therapy sessions designed to heal relationships and build a strong, reliable support system at home.
The journey ahead might seem daunting, but it’s a path you will never walk alone. From the first call to your last day in the program, our team is here to guide you. By taking the mystery out of the process, you can focus on what truly matters: getting better.
Overcoming Barriers to Accessing Treatment
Even when you know that integrated treatment for dual diagnosis is the gold standard, actually finding it can feel like navigating a maze. It’s not your fault. Individuals and families run into real, frustrating roadblocks that can make getting help feel overwhelming before it even starts.
Let's be honest about why this is so hard. For decades, mental health care and substance use treatment lived in two completely different worlds. They were separate systems, with separate rules and separate funding. You’d go to a mental health clinic for depression, and they’d tell you to come back after you handled your drinking. Then you’d go to a rehab, and they’d say they couldn’t help until your anxiety was stable. It was a classic catch-22. While that’s finally changing, the ghosts of that old, fragmented system are still around, creating gaps in care.
Systemic and Global Challenges
These aren't just local problems; they're baked into healthcare systems worldwide. Even in the countries that do the most research on dual diagnosis, people are falling through the cracks. A massive analysis of over 900 publications found that while places like the United States, Canada, and the UK lead the pack in studying integrated care, actually delivering that care consistently is a different story. You can discover more about these global research trends and see just how deep this fragmentation runs.
This broken system creates some very specific hurdles for families trying to find help:
- Insurance Hurdles: This is often the first and biggest headache. Insurance plans can have bafflingly different rules for mental health versus substance use, making it a nightmare to get a single, unified program approved.
- Shortage of Trained Professionals: Finding a clinical team that is genuinely cross-trained to treat both conditions at the same time is harder than it should be. True expertise in integrated treatment for dual diagnosis is still a specialized skill, and there just aren't enough people who have it.
- Geographic Limitations: Top-tier integrated treatment centers simply don’t exist in every town. This reality forces many families to either travel long distances or settle for a less effective, non-integrated program just because it's closer to home.
Knowing about these barriers isn’t meant to discourage you—it’s about preparing you for the fight. It validates the struggle you might already be feeling and helps you become a smarter, more effective advocate for yourself or your loved one.
Understanding that the system itself is complicated gives you the perspective to approach this search with patience and grit. It also shines a spotlight on why finding a provider like Altura Recovery—one built from the ground up to provide seamless, truly integrated care—is so critical to cutting through the red tape and getting on the path to lasting wellness.
Your Questions About Integrated Treatment, Answered
Deciding to start recovery brings up a lot of practical questions, and getting straight answers is the first step toward feeling confident and in control. We’ve put together a list of the most common things people ask when they're looking into integrated treatment for a dual diagnosis.
Our goal here is to cut through the confusion and show you that effective, accessible help is closer than you think.
How Do I Know If I Really Need Integrated Treatment?
If you catch yourself using alcohol or other substances to quiet your anxiety, numb depression, or push away traumatic memories, an integrated program is almost certainly the right move. The biggest telltale sign is a vicious cycle: when your mental health dips, your substance use climbs, and then the substance use makes your mental health even worse.
Another clue is feeling completely stuck, like you can't make progress on one problem without the other one flaring up and getting in the way. If you're fighting both battles at once, trying to treat them together isn’t just a good idea—it’s the only approach that really works. A professional assessment will give you a clear diagnosis and confirm the best path forward.
What’s the Difference Between PHP and IOP?
You'll hear these acronyms a lot. They're just different levels of outpatient care, designed to give you the right amount of support at the right time. The key thing to know is that with both, you get to go home every night.
Partial Hospitalization Program (PHP): This is the more structured, intensive option. Think of it as a bridge from residential treatment back to daily life. You'll typically have clinical programming for several hours a day, five days a week, giving you a ton of support as you start putting recovery skills into practice.
Intensive Outpatient Program (IOP): This level offers more flexibility. With fewer hours per week (usually 9-12 hours over three to five days), an IOP lets you keep up with work, school, or family life while still getting consistent, powerful therapy.
After your first assessment, our clinical team will talk with you about which level of care makes the most sense for your immediate needs and long-term goals.
The whole idea is to use a "step-down" approach. As you build confidence and stability, the intensity of your treatment adjusts, creating a smooth, sustainable ramp toward lasting wellness.
Will My Insurance Cover Integrated Treatment?
Yes, in most cases. The vast majority of major health insurance plans cover both mental health and substance use disorders, and that includes integrated programs like ours. A federal law called the Mental Health Parity and Addiction Equity Act (MHPAEA) actually requires insurance companies to provide coverage for these services that's on par with their coverage for medical or surgical care.
Of course, the specifics—like your copay, deductible, or how many sessions are covered—depend entirely on your plan. The quickest, easiest way to get concrete answers is to let our admissions coordinators help. They can verify your benefits for you (at no cost) and walk you through any out-of-pocket expenses. It takes all the guesswork out of the financial side of things.
How Long Is Treatment Going to Last?
There’s no magic number or one-size-fits-all schedule for recovery. The length of your program is completely personalized, based on your progress and clinical needs. The focus is always on making sure you're stable and feeling strong, not on hitting a date on the calendar.
Someone might start in our PHP for a few weeks, then transition to the IOP for a couple of months, and finally step down to a less intensive supportive outpatient program (SOP). The goal is to make sure that by the time you're done, you feel genuinely equipped with the coping skills you need to succeed for the long haul. Your care team works with you every step of the way to create a timeline that supports your entire recovery journey.
At Altura Recovery, we know you have questions, and we're here with answers. Our team is committed to making the first step toward healing as clear and supportive as it can be. If you or someone you care about is struggling with co-occurring disorders, reach out to us today to learn how our integrated treatment programs can help build a foundation for real, lasting freedom.








