Outpatient mental health treatment is a way to get consistent, structured support while still living your life. You attend therapy sessions and other services at a clinic during the day or evening but head back home afterward, letting you keep up with work, school, and family.
It’s designed to be a practical middle ground—more intensive than weekly therapy, but less disruptive than checking into a hospital.
Understanding the Core Concept of Outpatient Care
Think of your mental health journey like learning a new, complex skill—say, navigating a tricky trail. Inpatient or residential treatment would be like going away to a dedicated training camp for a few weeks, completely focused on that one skill, 24/7.
Outpatient mental health treatment, on the other hand, is like hiring an expert guide who meets you on your local trail several times a week. They teach you new techniques, help you read the terrain, and practice with you. Then, you go home and apply those skills on your own, knowing your guide will be back in a day or two to check your progress and teach you the next step.
This model is built on a simple but powerful idea: healing sticks when you can practice new coping skills in the real world, right as challenges pop up. It bridges the gap between round-the-clock supervision and a once-a-week therapy appointment, offering a robust support system that fits into your actual life.
To give you a clearer picture, let's compare the two main approaches side-by-side.
Outpatient vs Inpatient Care At a Glance
| Feature | Outpatient Treatment | Inpatient/Residential Treatment |
|---|---|---|
| Living Situation | Live at home, commute to treatment | Live at the facility 24/7 |
| Time Commitment | A few hours per day, several days a week | Full-time, 24 hours a day |
| Daily Life | Maintain work, school, and family roles | All daily activities paused |
| Environment | Practice skills in your real-world setting | Highly structured, controlled environment |
| Level of Support | High, but with more independence | Maximum, with constant supervision |
| Best For | Stable home environment, needing intensive support that fits a daily schedule | Medical instability, high risk of self-harm, or needing to escape a toxic environment |
This table shows how each model serves a different, crucial purpose. Outpatient care is all about integrating treatment with daily life, which is a key reason for its growing popularity.
Key Features of the Outpatient Model
The structure of outpatient care is intentionally flexible because everyone’s needs are different. Still, most quality programs share a few core characteristics:
- Living at Home: This is the defining feature. You sleep in your own bed and stay connected to your home life.
- Structured Scheduling: Treatment isn't random. You'll have a set schedule for individual therapy, group sessions, and medication management, ranging from a few hours a week to several hours a day.
- Integrated Support: You get a whole team. Your care is coordinated, often including a therapist, psychiatrist, and group facilitators all working together.
- Real-World Application: You can immediately try out the communication skills or coping strategies you learned in your morning group session at the dinner table that same night.
The Rise of Flexible and Accessible Treatment
This adaptable approach has become a cornerstone of modern mental health care for good reason. Outpatient services now make up about 35% of the behavioral health market, making it the largest single category of care. This trend reflects a major shift toward treatment that delivers high-quality clinical support without forcing people to put their entire lives on hold.
The flexibility is what makes it work. For example, more intensive options like a Partial Hospitalization Program (PHP) give you the structure and intensity of a full-day program but still allow you to return home each evening. You can learn more about how a partial hospitalization program provides intensive support while maintaining that crucial home connection. This integration is what helps recovery feel sustainable for so many people.
Exploring Different Levels of Outpatient Care
Outpatient treatment isn't a one-size-fits-all solution. It’s better to think of it as a spectrum of care with different levels of intensity—almost like a staircase where you can step up or down depending on the support you need at any given moment.
That flexibility is key, because recovery is rarely a straight line. Getting to know the main levels of care helps you find the right fit for where you are right now, ensuring you get the right amount of support without having to put your entire life on pause.
This diagram visualizes where outpatient treatment sits alongside inpatient options within the broader landscape of mental health care.
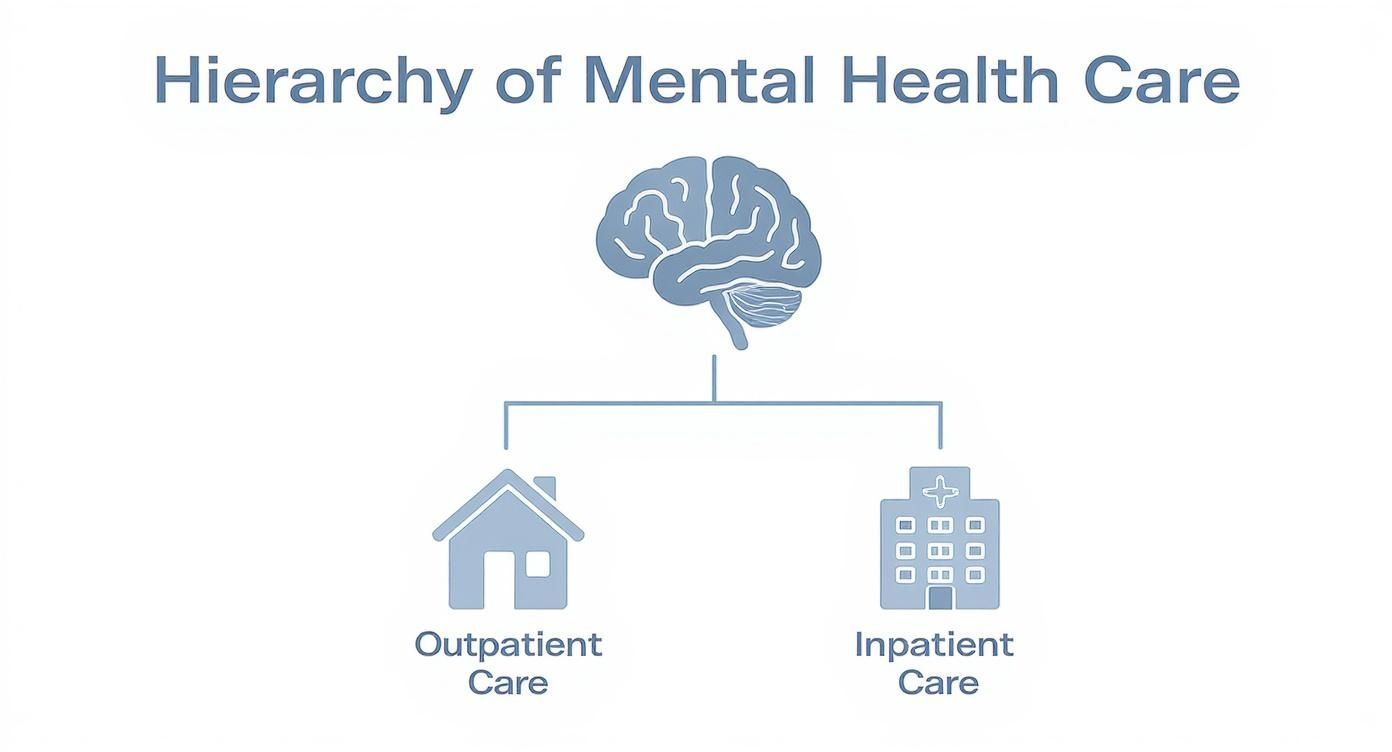
As you can see, outpatient and inpatient care are two very different paths. Outpatient models are specifically designed to be integrated into your home life, which is a crucial distinction to keep in mind as we look at the different program intensities available.
Partial Hospitalization Programs (PHP)
At the highest and most intensive end of the outpatient spectrum, you’ll find Partial Hospitalization Programs (PHP). A PHP offers the most robust level of treatment you can get outside of a residential or hospital facility. It’s built for individuals who need significant, structured support every day but have a safe and stable home to return to each evening.
Think of it as a full-time job focused squarely on your recovery. People in a PHP typically attend treatment for several hours a day, five to seven days a week. The highly structured schedule is packed with a mix of individual therapy, group sessions, and psychiatric care. This level of care is often the perfect next step for someone transitioning from an inpatient stay, or for anyone who needs more support than a less intensive program can provide to prevent hospitalization.
The main goal of a PHP is to stabilize symptoms and build a powerful foundation of coping skills in a supportive, structured environment. It masterfully bridges the gap between 24/7 care and greater independence.
Intensive Outpatient Programs (IOP)
The next step down in intensity is the Intensive Outpatient Program (IOP). An IOP provides a strong, consistent level of care but with more flexibility than a PHP, which makes it one of the most common and effective forms of outpatient mental health treatment.
An IOP allows individuals to maintain their commitments to work, school, or family while still receiving substantial therapeutic support. It’s a powerful model for integrating recovery skills directly into your daily life.
In a typical IOP, you’ll attend treatment for three to five days a week, with each session lasting about three hours. This might look like a morning program from 9 a.m. to noon or an evening program designed to fit around a standard workday. The core services almost always include:
- Group Therapy: This is the cornerstone of most IOPs. It's where you connect with peers who get what you're going through and practice new skills in a safe, supportive setting.
- Individual Counseling: You'll have regular one-on-one sessions with your therapist to work through personal challenges and track your progress.
- Medication Management: You'll have access to psychiatric professionals who can prescribe and monitor medications as part of your overall treatment plan.
IOPs are an ideal fit for individuals whose mental health is stable but who need consistent support to manage symptoms, prevent relapse, and continue building on their recovery. To get a better sense of the structure and goals, you can learn more about what defines rehab and recovery programs and see how the pieces fit together.
Standard Outpatient Programs (SOP)
The most flexible option on the outpatient staircase is the Standard Outpatient Program (SOP). This is often what people picture when they hear the words "therapy" or "counseling." It simply means meeting with a therapist, psychiatrist, or counselor on a regular but less frequent schedule—usually once or twice a week.
SOPs are perfect for individuals who have already developed a solid set of coping skills and are managing their symptoms well, but still benefit from ongoing professional support. This level of care works like a maintenance plan, helping you navigate life's challenges and reinforcing the progress you’ve already made in more intensive programs.
It's also a common starting point for people seeking help for the very first time who don't require a higher level of care. SOP services are tailored to your specific needs and goals, providing a consistent touchstone for your mental wellness. This "step-down" approach is designed to ensure a smooth transition back into daily life and promote long-term stability.
What Services Are Included in Outpatient Treatment
Knowing the different levels of outpatient care is one thing, but picturing what you'll actually do during treatment is another. A good outpatient program is so much more than just talking; it's a structured, multi-layered experience designed to help you build skills, connect with others, and create lasting change. Each service is like a building block, creating a strong foundation for your recovery.
The core of any quality program is a mix of therapeutic approaches that work together. Think of it like a personalized fitness plan: you don't just use one machine at the gym. A trainer combines strength training, cardio, and flexibility to get a balanced result. In the same way, outpatient mental health treatment blends different services to address your needs from every angle.
Individual Therapy: A Personal Space for Healing
One-on-one therapy is the cornerstone of outpatient treatment. This is your dedicated time with a licensed clinician to explore the roots of your challenges in a safe, confidential setting. It’s where you can dig deep into your personal history, specific thought patterns, and sensitive topics you might not be ready to share in a group.
Your therapist will use evidence-based approaches to guide these sessions. Some of the most common and effective methods include:
- Cognitive Behavioral Therapy (CBT): This practical, goal-oriented therapy helps you identify, challenge, and reframe negative thoughts and behaviors to build new coping skills.
- Dialectical Behavior Therapy (DBT): DBT is incredibly effective for managing intense emotions and improving relationships. It teaches crucial skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
- Eye Movement Desensitization and Reprocessing (EMDR): For those dealing with trauma, EMDR is a powerful technique that helps the brain process traumatic memories so they lose their emotional charge.
Many programs also integrate other powerful approaches. For example, some may incorporate complementary interventions like Deep Pressure Therapy for anxiety, which is known for its calming effect on the nervous system. It's also vital to learn more about what trauma-informed therapy involves and why this approach is so critical for creating a safe healing environment.
Group Therapy: The Power of Shared Experience
While individual therapy provides depth, group therapy provides connection and perspective. It's often the heart of an intensive outpatient program, offering a unique space to heal alongside others who genuinely get what you’re going through. Sharing your story with peers chips away at the feelings of isolation and shame that are often major barriers to recovery.
In a professionally facilitated group, you don't just receive support—you also give it. This dynamic builds self-esteem and reinforces your own progress as you help others on their journey.
Groups are typically focused on specific topics or skills, such as:
- Relapse Prevention Strategies
- Developing Healthy Coping Skills
- Managing Anxiety and Depression
- Building Communication Skills
This peer support is invaluable. It’s where you can practice the skills you’re learning in a safe, real-time social setting before taking them out into your daily life.
Psychiatric Care and Medication Management
For many people, mental wellness involves both therapeutic and biological support. That's why outpatient programs integrate psychiatric services to make sure your treatment plan is complete. This includes an initial psychiatric evaluation to get an accurate diagnosis and ongoing medication management.
A psychiatrist or psychiatric nurse practitioner works closely with your therapist to monitor your progress. They help figure out if medication could be a helpful tool for managing symptoms, find the right type and dosage, and make adjustments as needed. This collaborative approach ensures your mental and physical health are treated together.
Family Therapy and Case Management
Healing rarely happens in a vacuum. Outpatient programs recognize that family dynamics play a huge role in recovery, so family therapy sessions are often included. These sessions help repair relationships, improve communication, and teach loved ones how they can best support you.
On top of that, case management services help with the practical side of life. A case manager can connect you with community resources, assist with housing or employment needs, and coordinate with other healthcare providers. This ensures you have a stable foundation to build your recovery on.
Who Is a Good Candidate for Outpatient Programs?
Choosing the right level of mental health care is a huge step, and outpatient treatment isn't a one-size-fits-all solution. Just as a doctor matches a specific prescription to a specific illness, the most effective path forward is the one that aligns with your unique circumstances, needs, and goals.
So, how do you know if an outpatient program is the right fit for you or someone you care about?
The ideal candidate is someone who needs more structure and support than a weekly therapy session can offer but doesn't require the 24/7 medical supervision of an inpatient facility. They can generally function day-to-day but are finding it hard to manage their symptoms on their own.
Key Indicators of a Good Fit
Think of it like this: outpatient care builds on the foundation of your existing life. For the program to work, that foundation needs to be reasonably stable. If you see yourself or a loved one in these descriptions, outpatient treatment could be a fantastic choice.
- A Stable Home Environment: Your home should be a safe, supportive space. Since you'll return home after each session, having a non-chaotic environment that's free of major triggers is vital for putting what you learn into practice.
- Internal Motivation to Engage: Real, lasting change has to come from within. While nobody feels motivated 100% of the time, a genuine desire to show up, participate, and do the hard work of recovery is one of the strongest predictors of success.
- Medical and Psychological Stability: Outpatient care is not designed for acute crises. A good candidate is not an immediate danger to themselves or others and doesn't need intensive medical detox for substance use.
- Ability to Manage Daily Responsibilities: You might be struggling, but you're still able to handle basic duties like work, school, or family care, even if it feels overwhelming. Outpatient programs are built to support you in these roles, not take them over completely.
The core idea is simple: outpatient treatment is for people who can safely navigate their daily lives but need a professional, structured framework to build coping skills and address underlying mental health conditions.
Conditions Well-Suited for Outpatient Care
While every person is different, outpatient programs are especially effective for a wide range of common mental health conditions. They provide just enough structure to stabilize symptoms and the flexibility to practice new skills in the real world.
For example, people dealing with the following conditions often thrive in an outpatient setting:
- Anxiety Disorders: Including generalized anxiety, panic disorder, and social anxiety.
- Depressive Disorders: Such as major depressive disorder and persistent depressive disorder.
- Post-Traumatic Stress Disorder (PTSD): For cases where symptoms are manageable without constant supervision.
- Co-Occurring Disorders: Situations where both a mental health and substance use disorder are present, as long as the person is medically stable.
Research on community-based care models—which often serve individuals with behavioral health needs—shows that structured outpatient services lead to better follow-up after hospitalization and more consistent use of helpful resources. This just reinforces how effective it is to provide robust support right in a person's home community.
When Inpatient Care Is the Better Option
It's just as important to recognize when outpatient treatment is not the right choice. In some situations, the safety and constant supervision of an inpatient or residential program are non-negotiable.
Inpatient care is typically the right call for:
- Acute Crisis: If someone is having suicidal thoughts with a plan, experiencing psychosis, or is otherwise unable to keep themselves safe.
- Severe Substance Withdrawal: When medical detoxification is necessary to manage dangerous physical withdrawal symptoms.
- Unstable Living Situation: If the home environment is abusive, chaotic, or actively fuels substance use or mental health symptoms.
- Previous Failed Outpatient Attempts: If less intensive levels of care have already proven insufficient to stabilize the person's condition.
Making an informed decision comes down to an honest assessment of your current needs. At Altura Recovery, our programs are specifically designed for those who are ready for outpatient care. We offer a clear step-down model that provides the right amount of support as you move toward greater independence.
How to Choose the Right Outpatient Provider

Finding the right team for outpatient mental health treatment is easily one of the most important decisions you’ll make on your recovery journey. The right fit can make all the difference, creating a safe, supportive space where you feel seen, understood, and truly empowered to heal.
But with so many programs out there, how can you tell which one actually aligns with your needs?
Making a confident choice starts with knowing what to look for. Think of it like interviewing a potential partner in your health—you need to make sure their qualifications, philosophy, and overall approach match your goals. This goes way beyond finding a convenient location; it’s about finding a place that offers high-quality, evidence-based care delivered with genuine compassion.
Look for Credentials and Licensing
First things first, and this is non-negotiable: verify the provider’s credentials. Legitimate treatment centers should be fully licensed by the state and, ideally, accredited by national organizations. These aren't just fancy badges; they’re your assurance that the facility meets strict standards for safety, quality of care, and ethical practices.
Keep an eye out for accreditation from bodies like:
- The Joint Commission: A nationally recognized seal of quality that shows a commitment to meeting rigorous performance standards.
- CARF International (Commission on Accreditation of Rehabilitation Facilities): This accreditation focuses specifically on ensuring providers deliver the best possible outcomes for their clients.
These certifications confirm that the provider is held accountable to a higher authority, giving you peace of mind that you’re in a safe and professional environment.
Evaluate the Clinical Team and Their Approach
A program is only as good as its people. Before committing, take some time to learn about the clinical team's qualifications and specializations. Are there licensed therapists, counselors, and psychiatrists on staff? Do they have deep experience with the specific challenges you’re facing, like trauma, anxiety, or co-occurring disorders?
Just as important is their therapeutic approach. A quality provider will be transparent about the treatment methods they use, like CBT, DBT, or EMDR. They should put a heavy emphasis on evidence-based therapies—methods that are backed by solid scientific research to be effective.
When you choose a provider, you are entrusting them with your well-being. A commitment to evidence-based practices shows that their treatment plans are built on proven methods, not guesswork, leading to more sustainable recovery outcomes.
Ask About Personalized Treatment Planning
Be wary of any provider that pushes a one-size-fits-all solution. Your history, your needs, and your goals are unique, and your treatment plan should reflect that. A key marker of a high-quality outpatient provider is their dedication to creating a truly personalized care plan.
During your initial consultation, don't be shy. Ask direct questions about their process:
- How exactly do you develop an individual's treatment plan?
- How often is my plan reviewed and adjusted based on my progress?
- How will my personal goals be woven into therapy?
- What does a successful outcome look like in your program?
At Altura Recovery, we build every treatment plan from the ground up, starting with a comprehensive assessment. Our step-down model—from PHP to IOP to SOP—is designed to adapt as you progress, ensuring you always have the right level of support at the right time. This personalized approach is fundamental to helping you achieve real, lasting healing on your own terms.
Common Questions About Outpatient Treatment
Stepping into any kind of mental health care brings up a lot of practical questions. Knowing the answers ahead of time can make the whole process feel less intimidating and help you figure out if an outpatient program is the right fit for your life.
Let's clear up some of the most common questions people have.
How Long Does an Outpatient Program Usually Last?
There’s no one-size-fits-all timeline for healing, so the length of any program is always tailored to you. How long you’re in treatment really depends on your specific needs, the progress you’re making, and which level of care you’re in.
- Higher Intensity (PHP & IOP): These programs are more structured and focused. A Partial Hospitalization Program (PHP) or an Intensive Outpatient Program (IOP) usually runs for several weeks to a few months. The idea is to stabilize your symptoms and give you a strong set of skills in a short, concentrated period.
- Ongoing Support (SOP): A Standard Outpatient Program (SOP), which might be just one or two therapy sessions a week, can be more of a long-term thing. It works like a maintenance plan to help you sustain your recovery over time.
The best programs, like ours at Altura Recovery, are constantly checking in on your progress. We adjust your treatment plan as you go, making sure you step down to a lower level of care only when you’re truly ready.
Can I Still Work or Go to School?
Yes, absolutely. In fact, that's one of the biggest benefits of outpatient care. This model is specifically built to fit into your life, not take you out of it. You get the strong support system you need while staying connected to your job, your classes, and your family.
To make it work, many programs offer flexible schedules:
- Daytime Programs: A great option if you work evenings or have other commitments later in the day.
- Evening Programs: Perfect for people who have a traditional 9-to-5 job or are in school during the day.
This setup lets you take what you learn in therapy—like new coping skills—and immediately put them to the test in real-world situations at work or home. It makes recovery feel much more grounded and achievable.
What's the Difference Between Just Going to Therapy and an Outpatient Program?
While individual therapy is a huge piece of the puzzle, a formal outpatient program is a much more complete and structured approach. Think of it like this: therapy is like seeing a single specialist, while an outpatient program is like having a whole coordinated team of doctors working together on your case.
A one-on-one therapist can help you do deep, personalized work. But an outpatient program wraps you in a multi-layered support system, tackling your needs from several angles at once.
A program will almost always include individual therapy, but it adds other critical services like group therapy sessions, skills-building workshops, psychiatric check-ins, and medication management. This layered strategy offers a much higher level of support and accountability than a single weekly therapy session can, creating a powerful framework for real change.
At Altura Recovery, we know that no two recovery journeys are the same. Our flexible outpatient programs are designed to meet you where you are, providing evidence-based care that empowers you to build a foundation for lasting wellness. To see how our step-down model can support you, please visit us online.